Introduction
Welcome to our website, where we provide valuable information to help you understand the medical billing process. Medical billing can be complex and confusing, but having a grasp of the steps involved can empower you to navigate through it with ease. This article will outline the key stages in the medical billing process, ensuring that you have a clear understanding of how it works.
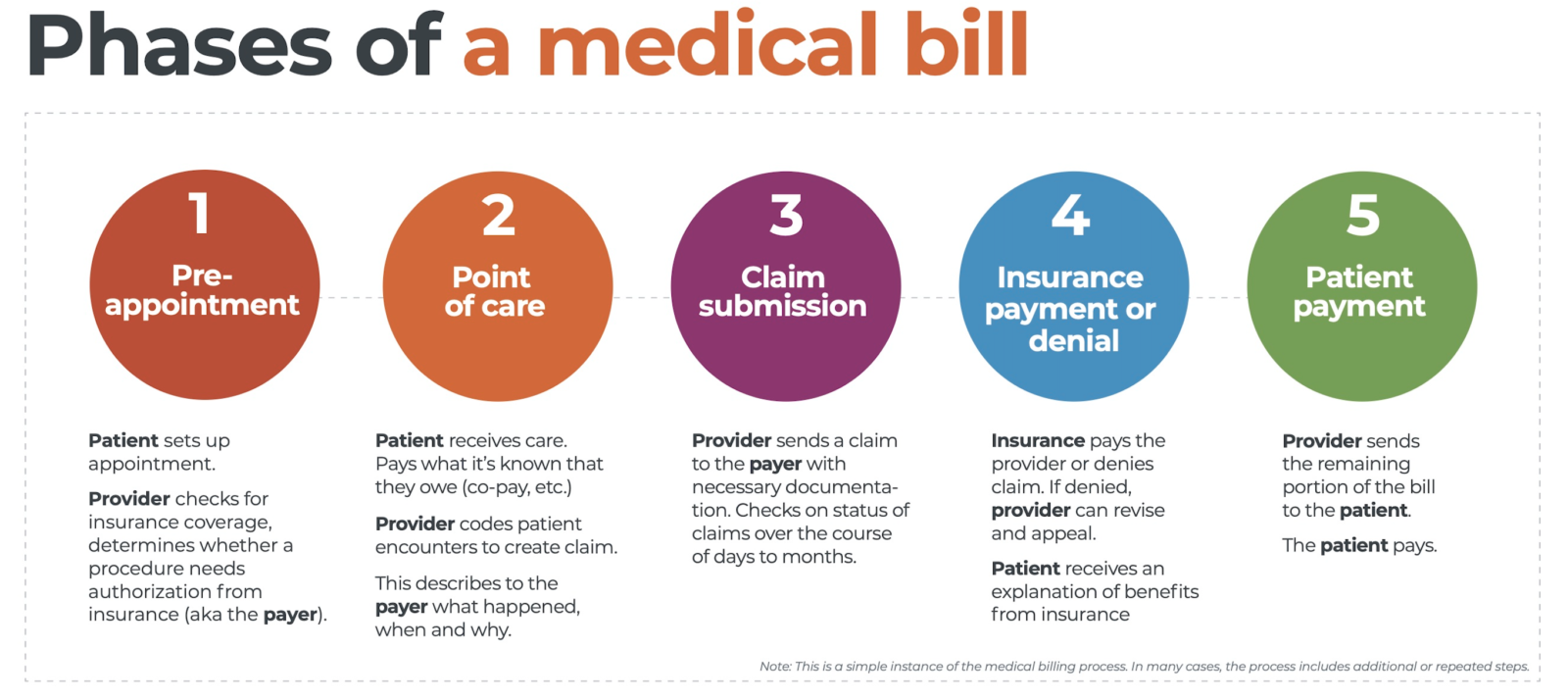
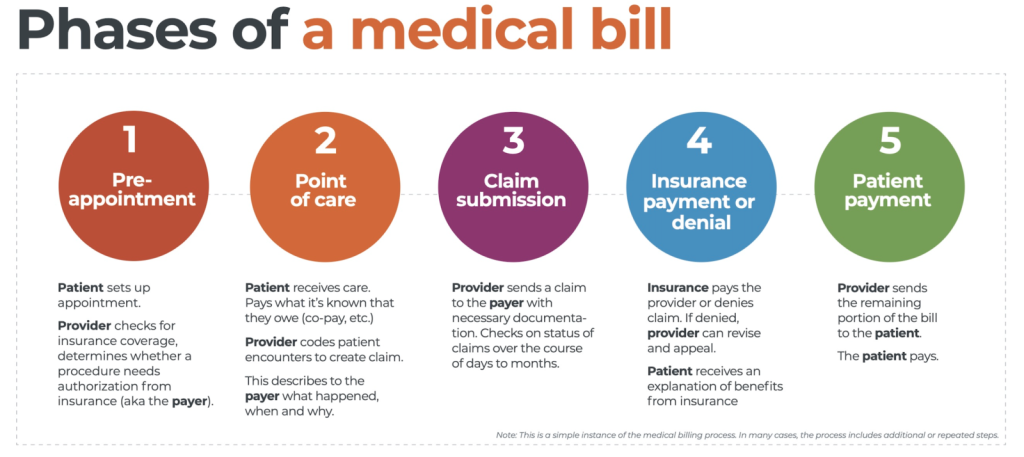
Step 1: Patient Registration and Insurance Verification
Before any medical services are provided, you will need to complete the patient registration process. This involves providing your personal and insurance information, which will be verified by the healthcare facility. The accuracy of this information is crucial to ensure smooth processing of your medical claims.
Step 2: Documentation and Coding
Once you have received medical services, the healthcare provider will document the details of your visit or procedure using specific codes. These codes describe the nature of the service provided, and they are essential for accurately billing your insurance company.
Step 3: Claim Submission
After the coding is complete, the healthcare provider will submit a claim to your insurance company. This claim includes the codes, along with any supporting documentation required by the insurer. The claim is then reviewed by the insurance company for payment determination.
Step 4: Insurance Adjudication
During this stage, the insurance company processes the claim and determines the amount they will cover. This can include various factors such as deductibles, co-pays, and policy limitations. Once the claim has been adjudicated, the healthcare provider will receive payment or an explanation of benefits.
Step 5: Patient Billing
If there is any remaining balance after insurance coverage, you will receive a bill from the healthcare provider for your portion. This bill will outline the amount owed and provide payment instructions. It is important to review the bill carefully and promptly settle any outstanding balance.
By understanding the medical billing process, you can be better prepared to navigate the administrative side of healthcare effectively. Take the time to familiarize yourself with these steps to ensure a smooth and less stressful experience. Remember, if you have any questions or concerns, reach out to your healthcare provider or our website for assistance.
Overview of Medical Billing
Medical billing is a crucial part of the healthcare system that ensures accurate and timely payment for medical services provided to patients. It is a complex and multi-step process involving various stakeholders, including healthcare providers, insurance companies, and patients. Understanding the medical billing process is essential for both healthcare professionals and patients to navigate the intricacies of healthcare finances effectively.
Definition of Medical Billing
Medical billing refers to the process of creating and submitting claims to insurance companies or other third-party payers to receive payment for healthcare services rendered. This includes documenting patient information, coding diagnoses and procedures, and preparing and submitting claims for reimbursement. It also involves communicating with insurance companies to resolve any discrepancies or denials.
Importance of Medical Billing
Accurate and efficient medical billing is vital for healthcare providers to ensure proper revenue management and reimbursements. It enables healthcare professionals to focus on delivering quality care without worrying about financial aspects. Additionally, medical billing helps insurance companies evaluate claims, determine coverage, and facilitate timely payments to healthcare providers.
Key Players in Medical Billing
The medical billing process involves several key players, each with specific roles and responsibilities. These include healthcare providers, who deliver medical services and generate claims; billing and coding specialists, who ensure accurate coding and claim submission; insurance companies, who process and reimburse claims; and patients, who may need to provide insurance information and pay any outstanding balances.
Understanding the medical billing process empowers healthcare professionals and patients alike by minimizing confusion and facilitating effective communication. By gaining insight into the intricacies of medical billing, individuals can better navigate the complexities of healthcare finances and ensure timely and accurate payments for medical services provided.
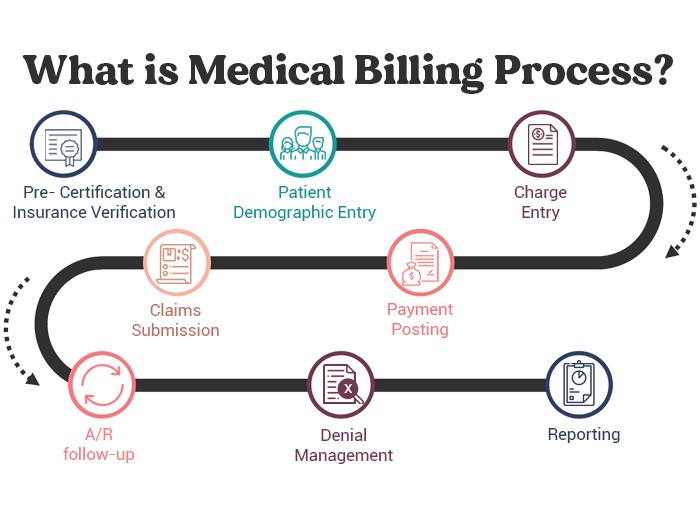
Pre-Billing Process
The pre-billing process is an essential step in ensuring a smooth medical billing experience. It involves several crucial tasks that need to be completed accurately and efficiently. First, the patient registration process begins as soon as you arrive at a healthcare facility. During this step, your personal and insurance information is collected, including your name, address, contact details, and insurance policy details. This information is crucial for the billing process, as it helps determine the coverage and benefits provided by your insurance plan.
The next step is insurance verification, where the healthcare provider contacts your insurance company to confirm your coverage and eligibility for the services received. This ensures that any necessary pre-authorization or referrals are obtained prior to treatment or procedures. It is important to ensure that your insurance information is up to date and that you inform the provider of any changes to prevent any billing issues.
Once the patient registration and insurance verification are completed, the medical coding and documentation process begins. During this step, the healthcare provider assigns appropriate diagnosis and procedure codes to the services provided. These codes are crucial for ensuring accurate billing and reimbursement from both the insurance company and the patient. Additionally, proper documentation of the services rendered is vital for supporting the medical necessity and appropriateness of the billed charges.
Understanding the pre-billing process is important to ensure that your medical billing experience is efficient and error-free. By ensuring accurate patient registration, insurance verification, and proper medical coding and documentation, you can help prevent billing issues and expedite the reimbursement process. So, next time you visit a healthcare facility, rest assured that these steps are being followed to ensure a seamless billing experience for you.
This image is property of cdn2.hubspot.net.
Billing Process
Understanding the medical billing process is crucial to ensure accurate and timely payment for healthcare services. This article will guide you through the steps involved in medical billing, providing you with valuable insights into how this complex system works.
Claim Submission
The first step in the medical billing process is claim submission. After receiving treatment, your healthcare provider will create an itemized bill that lists the services rendered, along with corresponding billing codes. These codes accurately describe the procedures performed and enable insurance companies to determine coverage and reimbursement amounts. Once the claim is prepared, it is electronically submitted to the insurance provider for review and processing.
Claim Adjudication
Claim adjudication is the next stage wherein the insurance company reviews your claim to determine its accuracy and compliance with their guidelines. This process involves verifying your eligibility for coverage, assessing the medical necessity of the services provided, and comparing the billed amount against the agreed-upon rates. The insurance company may request additional documentation or clarification before reaching a final decision.
Payment Posting
Once the claim is approved, payment posting occurs. This step involves recording the payment received and applying it to the appropriate accounts. Payments can come from various sources, including insurance companies, patients, or government programs. The medical billing team ensures that payments are correctly credited, and any remaining balance not covered by insurance is accurately billed to you.
Understanding the medical billing process is essential for both healthcare providers and patients. By educating yourself about each step, you can navigate the system with confidence and ensure fair and accurate payment for the services you receive.
Post-Billing Process
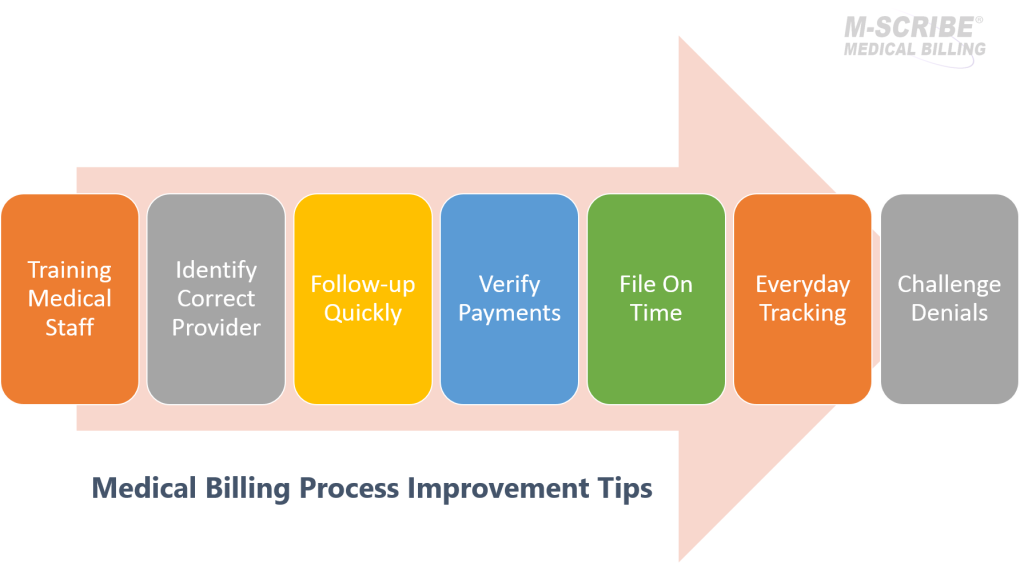
After the billing process is completed, there are a few important steps that follow to ensure that all claims are properly handled and any denials or discrepancies are addressed promptly. This section will provide an overview of the post-billing process, including denial management, appeals process, and patient statements and collections.
Denial Management
Denials happen when a claim is rejected by the insurance company. These can occur for various reasons, such as incorrect coding or missing information. It’s crucial to have a denial management system in place to identify and rectify these denials. This involves investigating the reason for denial, correcting any errors, resubmitting the claim, and following up until it gets resolved.
Appeals Process
If a claim is denied, you have the option to appeal the decision. The appeals process involves gathering all necessary documentation, such as medical records and supporting documents, and submitting them to the insurance company for review. It is important to follow the specific guidelines and deadlines set by the insurance company when filing an appeal.
Patient Statements and Collections
Once the claims have been processed and any denials or appeals have been resolved, patient statements are generated. These statements detail the amount owed by the patient, including deductibles, co-pays, or any remaining balance after insurance payments. It is crucial to have an efficient system in place for sending these statements and tracking payments. In cases where patients fail to make payments, a collections process may be necessary to recover the outstanding balance.
Understanding the post-billing process is essential for effectively managing medical billing and ensuring timely and accurate reimbursements. By closely monitoring denial management, navigating the appeals process, and maintaining an efficient patient statement and collections system, you can streamline your medical billing operations and optimize financial outcomes.
This image is property of www.caplinehealthcaremanagement.com.
Understanding the Medical Billing Process
The medical billing process involves a series of steps to ensure that healthcare providers are appropriately reimbursed for the services they provide. To gain a better understanding of this complex process, let’s delve into the details.
Electronic Medical Billing

Benefits of Electronic Billing
Electronic medical billing has revolutionized the healthcare industry, streamlining the billing process and reducing human error. By submitting claims electronically, healthcare providers can ensure faster processing times and quicker reimbursement. Additionally, electronic billing allows for real-time eligibility verification and claim status updates, optimizing efficiency and reducing administrative costs.
Implementation and Challenges
Implementing electronic billing systems can be a challenging task, requiring healthcare facilities to invest in technology infrastructure and staff training. However, despite the initial hurdles, the long-term benefits outweigh the challenges. Electronic billing systems enable healthcare providers to accurately track and manage claims, reducing the risk of claim denials and increasing revenue.
Security and Privacy Concerns
One major concern surrounding electronic medical billing is the security and privacy of patient information. Healthcare providers must ensure that they have robust data security measures in place to protect sensitive patient data and comply with HIPAA regulations. Strict encryption protocols, access controls, and regular system audits are essential to maintaining patient privacy and preventing unauthorized access to medical records.
Understanding the medical billing process is vital for both healthcare providers and patients. By embracing electronic billing methods, healthcare facilities can enhance efficiency, reduce errors, and ensure timely reimbursement, ultimately leading to better patient care. So, embrace the advantages of electronic billing and streamline your medical billing process today.
Billing Errors and Fraud
Understanding the medical billing process is essential in order to ensure accurate reimbursement and prevent fraudulent activities. This section will delve into the common billing errors that can occur, the various types of billing fraud, and the measures you can take to prevent and detect such fraudulent activities.
Common Billing Errors
Billing errors can range from simple mistakes to intentional misrepresentations. Some common errors include incorrect patient information, coding errors, duplicate billing, and upcoding or unbundling services. These errors can result in delayed or denied payments, financial losses, and even legal consequences.
Types of Billing Fraud
Billing fraud involves intentionally submitting false or misleading claims for reimbursement. Some examples of billing fraud include phantom billing (billing for services not provided), unbundling services to inflate charges, billing for unnecessary procedures, and altering medical records. These fraudulent activities not only harm the healthcare system financially but also compromise patient care.
Preventing and Detecting Fraud
To prevent and detect billing fraud, it is crucial to implement effective internal control measures. This includes regular audits, proper training on coding and billing guidelines, thorough documentation and record-keeping, and utilizing technological tools to identify irregularities. It is also important to report any suspicion of fraud to the appropriate authorities.
Understanding the common billing errors and various types of billing fraud can help you navigate the medical billing process with confidence, ensuring fair reimbursement and safeguarding against fraudulent activities.
This image is property of www.waystar.com.
Conclusion
Understanding the medical billing process is crucial for anyone who wishes to navigate the complex world of healthcare payments. By familiarizing yourself with the various steps involved in medical billing, you can better understand the billing statements you receive and ensure that you are being charged accurately for the healthcare services you have received.
In this article, we have explored the key steps involved in the medical billing process. We began by discussing the importance of accurate documentation, including the gathering of patient information, insurance verification, and the creation of encounter forms. We then moved on to the coding and billing process, explaining how healthcare providers assign specific codes to the services they provide and submit claims to the insurance companies. Next, we discussed the role of insurance in the medical billing process, including the common types of insurance plans and how they impact payment.
Finally, we explored the payment process, detailing how healthcare providers receive reimbursements from insurance companies and how patients are responsible for any remaining balance. We also touched on the various payment options available to patients, such as payment plans and assistance programs.
By understanding the medical billing process, you can advocate for yourself and ensure that you are being billed accurately and fairly for the medical services you receive. Whether you are a patient or a healthcare provider, having a working knowledge of medical billing is essential in today’s complex healthcare landscape.