Understanding the purpose and significance of medical billing is crucial for healthcare professionals and patients alike. This integral process encompasses the submission and tracking of medical claims, ensuring accurate reimbursement from insurance companies. By efficiently managing medical billing, healthcare providers can focus their attention on patient care, while patients can receive the necessary treatments and services without bearing the burden of excessive out-of-pocket expenses. In this article, we will explore the purpose, benefits, and key elements of medical billing to shed light on its importance in the healthcare industry.
Definition of Medical Billing
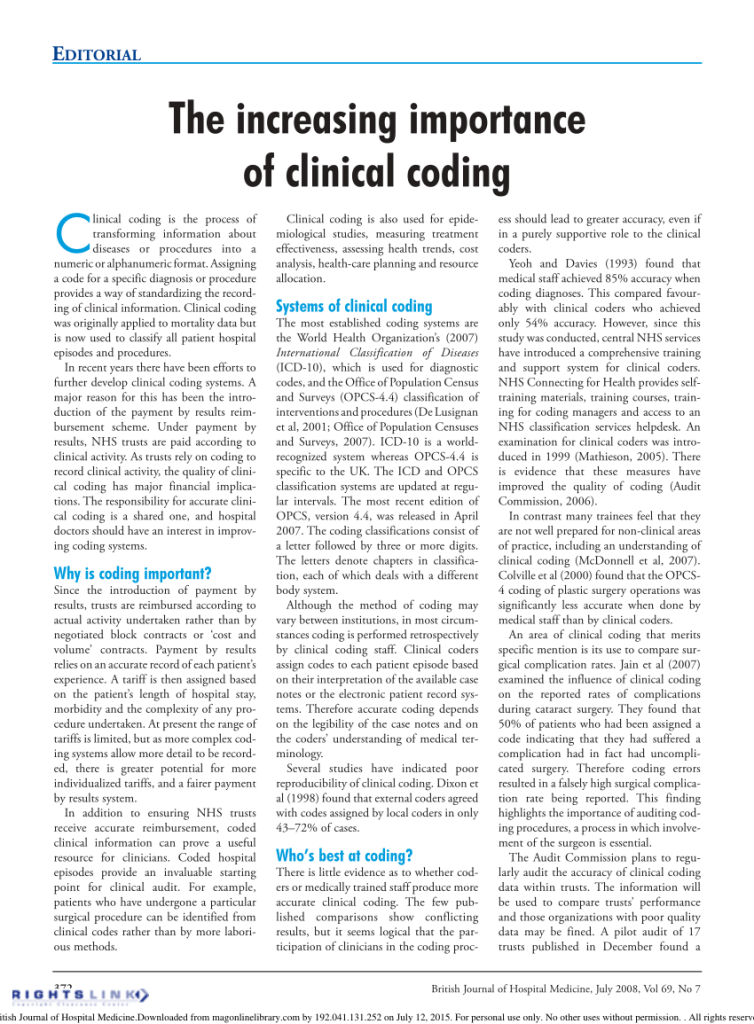
Medical cost concept with stethoscope and medical bill
Explanation of medical billing
Medical billing is a critical process in the healthcare industry that involves the submission and management of patient claims to insurance companies for reimbursement of provided medical services. It encompasses a wide range of tasks and responsibilities, from verifying patient insurance coverage to submitting claims and following up on payment. Effective medical billing ensures accurate financial transactions, facilitates healthcare reimbursements, maintains patient records, and supports the overall revenue cycle management of healthcare organizations.
Different types of medical billing
There are various types of medical billing, depending on the setting in which it is conducted. Some common types include:
- Professional Billing: This type of billing is performed by healthcare professionals, such as physicians, dentists, and therapists, who bill for their services rendered.
- Facility Billing: Facility billing involves billing for services provided by hospitals, clinics, and other healthcare facilities. It includes both inpatient and outpatient services.
- Institutional Billing: This type of billing is specific to institutions such as nursing homes, hospices, and rehabilitation centers, which provide a range of healthcare services.
- Durable Medical Equipment (DME) Billing: DME billing involves billing for specialized medical equipment, such as wheelchairs, oxygen supplies, and prosthetics.
- Ambulance Billing: Ambulance services require their own specific billing processes due to the unique nature of their services.
It is important to note that each type of medical billing has its own specific requirements and coding systems, and medical billers need to be well-versed in these distinctions to effectively navigate the billing process.
Importance of Medical Billing

Ensuring accurate financial transactions
Accurate medical billing is crucial for healthcare providers to receive proper compensation for the services they render. It involves accurately documenting and coding the services provided, ensuring that the appropriate charges are billed to insurance companies or patients. Without accurate billing, healthcare organizations may experience financial losses or face legal issues due to improper reimbursement.
Facilitating healthcare reimbursements
Medical billing plays a pivotal role in facilitating reimbursements from insurance companies. By submitting accurately coded claims with supporting documentation, medical billers help ensure that healthcare providers are reimbursed in a timely manner. This, in turn, allows healthcare organizations to maintain a steady revenue stream and continue providing quality care to patients.
Maintaining patient records
Medical billing is closely linked to patient records management. Through the billing process, medical billers maintain detailed records of patient encounters, services provided, and insurance information. This documentation not only enables accurate billing but also serves as a comprehensive record of a patient’s medical history. These records are essential for continuity of care and can be used for future reference by healthcare providers.
Supporting healthcare revenue cycle management
Medical billing is a vital component of the healthcare revenue cycle, which encompasses all financial processes from patient registration to the final collection of payment. By diligently managing the billing process, medical billers contribute to the overall efficiency and effectiveness of revenue cycle management. This includes monitoring claim status, identifying billing errors, and addressing denied claims. By optimizing the revenue cycle, healthcare organizations can improve their financial performance and enhance their ability to provide quality care.
Role of Medical Billers

Responsibilities of medical billers
Medical billers are responsible for a variety of tasks related to the billing and reimbursement process. Their main responsibilities include:
- Verifying patient insurance coverage and eligibility
- Accurately coding medical procedures and diagnoses
- Preparing and submitting claims to insurance companies
- Following up on claim status and addressing denials
- Processing patient payments and reconciling accounts
- Ensuring compliance with regulatory requirements
- Maintaining detailed and accurate patient records
- Collaborating with healthcare providers and insurance companies to resolve billing issues
Medical billers are crucial members of the healthcare team and play a significant role in ensuring the financial viability of healthcare organizations.
Working with healthcare providers and insurance companies
Medical billers act as intermediaries between healthcare providers and insurance companies. They work closely with healthcare providers to gather necessary documentation, such as medical records and explanation of benefits (EOB), to support claim submission. Additionally, medical billers communicate with insurance companies to verify patient coverage, resolve claim inquiries, and negotiate payment terms.
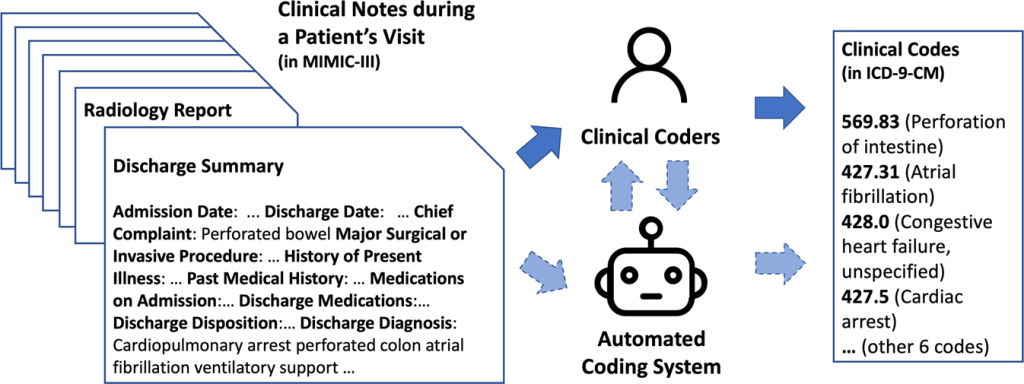
Navigating complex medical coding systems
Medical coding is an integral part of the medical billing process. It involves assigning specific codes to medical procedures, diagnoses, and services provided during patient encounters. Medical billers must be proficient in various coding systems, such as the International Classification of Diseases (ICD) and the Current Procedural Terminology (CPT). Navigating these coding systems accurately ensures proper reimbursement and reduces the risk of billing errors or claim denials.
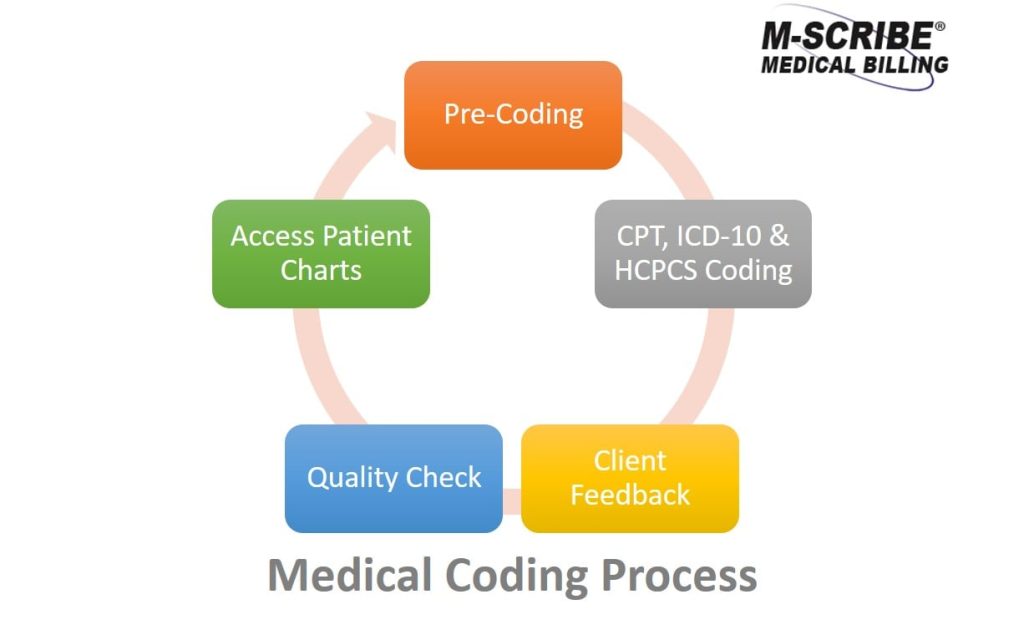
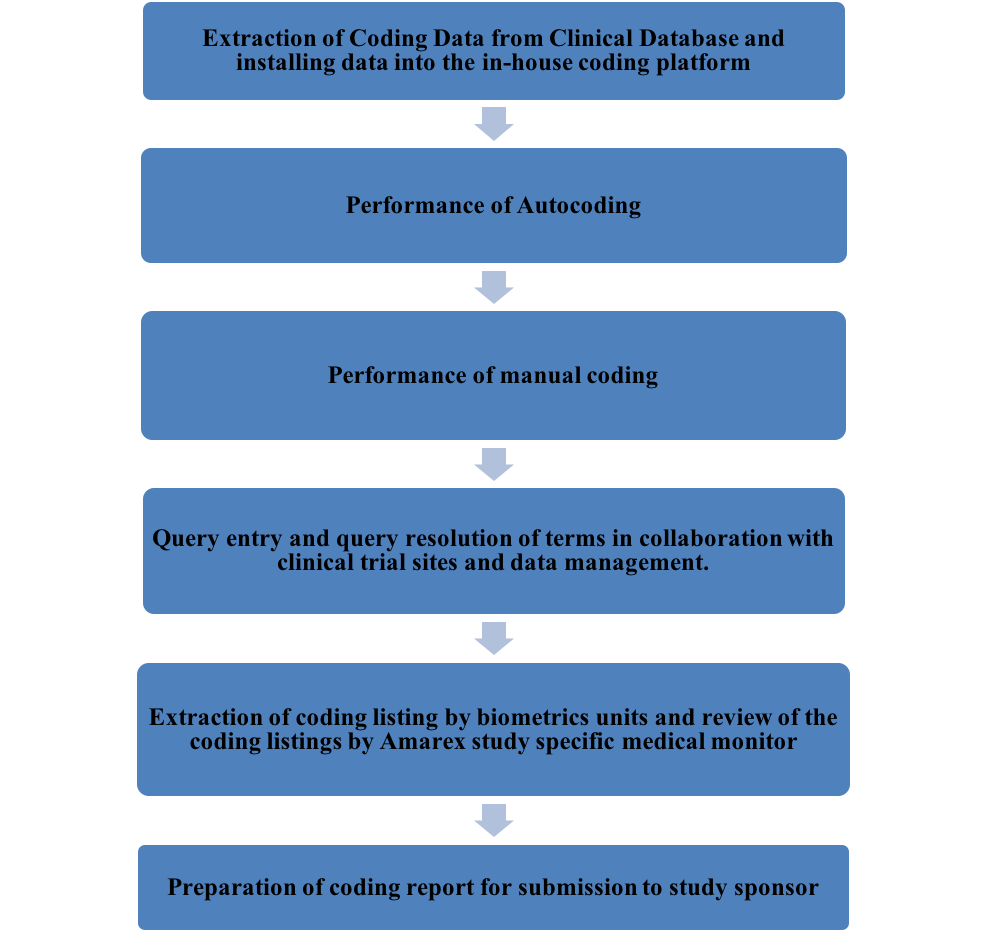
The Process of Medical Billing

Patient demographics and insurance verification
The medical billing process begins with the collection of patient demographics and insurance information. Medical billers gather relevant patient details, such as name, address, contact information, and insurance policy information. They then verify the patient’s insurance coverage and eligibility to ensure they are eligible for reimbursement.
Medical coding and charge capture
Once patient information is verified, medical billers proceed to the coding and charge capture phase. They accurately code medical procedures, diagnoses, and services provided during patient encounters using standardized coding systems. These codes help translate the healthcare services into a language that insurance companies understand for reimbursement purposes.
Claim submission and follow-up
After coding and charge capture, medical billers prepare and submit claims to insurance companies for reimbursement. Electronic claims submission is the most common method used today, as it expedites the process and reduces the chances of errors. Medical billers closely monitor the status of submitted claims and follow up with insurance companies to ensure timely reimbursement.
Payment posting and reconciliation
Once insurance companies process the claims and reimburse the healthcare provider, medical billers post the payments to the patient’s account. They record the payment amounts and reconcile them with the billed charges to ensure accuracy. In cases where patients are responsible for co-pays, deductibles, or other out-of-pocket expenses, medical billers generate patient statements and facilitate the collection of payments.
Appeals and denial management
In some cases, insurance companies may deny or question the reimbursement claims. Medical billers are responsible for evaluating and addressing these denials. They may appeal the denial with additional documentation or engage in negotiations with insurance companies to resolve claim disputes. Denial management requires strong communication skills and attention to detail to ensure that healthcare providers receive fair compensation for services rendered.
Medical Billing Software

Overview of medical billing software
medical billing software is designed to streamline and automate the billing process, enhancing the efficiency and accuracy of medical billing tasks. These software solutions are specifically tailored for medical billing professionals and offer a comprehensive set of features and functionalities to support the billing workflow.
Features and functionalities
Medical billing software typically includes features such as:
- Patient data management: Software allows for the easy organization and retrieval of patient demographics, insurance information, and medical records.
- Coding assistance: Medical billing software often provides built-in coding tools and reference databases to assist billers in assigning accurate codes.
- Claim generation and submission: Software facilitates the creation and submission of claims electronically, reducing manual errors and expediting the reimbursement process.
- Claim status tracking: Medical billing software allows billers to monitor the status of submitted claims and receive real-time updates on claim processing.
- Reporting and analytics: Software often includes reporting and analytics capabilities, providing insights into billing trends, denial rates, and overall revenue performance.
- Integration with electronic health records (EHR): Many medical billing software solutions integrate with EHR systems, enabling seamless transfer of patient data and minimizing duplication of efforts.
Benefits of using medical billing software
The adoption of medical billing software offers several advantages, including:
- Increased efficiency: Automation of billing tasks reduces manual labor and allows medical billers to focus on more complex and critical processes.
- Improved accuracy: Software solutions reduce the risk of human error in coding and claim submission, leading to higher levels of accuracy in billing.
- Faster reimbursement: Electronic claim submission and real-time claim tracking accelerate the reimbursement process, ensuring timely payments to healthcare providers.
- Enhanced compliance: Medical billing software often incorporates built-in compliance checks, reducing the risk of errors and ensuring adherence to regulatory requirements.
- Cost savings: By optimizing the billing workflow and reducing denials, medical billing software can help healthcare organizations save time and resources, ultimately improving their financial performance.
Ensuring Compliance in Medical Billing

Importance of compliance in medical billing
Compliance in medical billing is of paramount importance to ensure ethical and legal practices in healthcare. Compliance involves adhering to regulations, guidelines, and standards set by various entities, including government agencies and industry bodies. It helps protect patient privacy, prevent fraud, and maintain the integrity of the healthcare billing system.
HIPAA regulations and patient privacy
The health insurance Portability and Accountability Act (HIPAA) sets the standards for protecting patient privacy and the security of health information. Medical billers must comply with HIPAA regulations by safeguarding patient information and ensuring its confidentiality. This involves implementing strict access controls, encrypting electronic data, and maintaining secure storage and transmission of patient records.
Medical coding compliance
Medical coding compliance refers to the accurate application of coding guidelines and rules established by coding systems such as the ICD and CPT. Medical billers must follow these coding guidelines to ensure proper reimbursement and avoid compliance issues. Non-compliance with coding regulations can result in claim denials, delays in reimbursement, or even legal penalties.
Audits and fraud prevention
Regular audits and internal controls are essential to identify and prevent fraudulent activities in medical billing. Healthcare organizations often conduct internal audits to review billing practices and ensure compliance with regulations. Medical billers play a crucial role in supporting these audits by maintaining accurate documentation, reconciling financial records, and participating in compliance training and education programs.
Current Trends and Challenges

Aerial view of businessman using computer laptop
Transition to electronic medical records
The healthcare industry is undergoing a significant shift from traditional paper-based records to electronic medical records (EMRs) or electronic health records (EHRs). This transition has posed both opportunities and challenges for medical billing professionals. While EMRs/EHRs have streamlined the documentation and data sharing process, medical billers must adapt to new billing software systems and ensure that information is accurately extracted from electronic records for coding and billing purposes.
Adoption of telehealth services
The COVID-19 pandemic has accelerated the adoption of telehealth services, allowing healthcare providers to deliver virtual care and consultations remotely. While telehealth offers numerous benefits, it also presents billing complexities. Medical billers need to understand the reimbursement policies and guidelines specific to telehealth services, ensure accurate coding and billing, and navigate the evolving regulatory landscape surrounding this rapidly expanding area of healthcare.
Changing healthcare regulations
The healthcare industry is subject to continuous regulatory changes, which impact medical billing practices. Medical billers need to stay updated with changing regulations, such as updates to the Medicare or Medicaid programs, changes in coding guidelines, and modifications to billing regulations. This requires ongoing education and training to stay abreast of the latest developments and ensure compliance with current regulations.
Increasing complexity of medical coding
Medical coding is becoming increasingly complex due to advancements in medical technologies and procedures. New procedures and treatments require the creation of new codes and guidelines to accurately capture the services provided. Medical billers must continually update their knowledge and skills to adapt to these changes, ensuring accurate coding and billing to avoid claim denials and reimbursement delays.
The Future of Medical Billing

Automation and artificial intelligence
The future of medical billing is closely tied to advancements in automation and artificial intelligence (AI). Automation technologies can streamline routine billing tasks, such as claim generation and payment posting, reducing the administrative burden on medical billers. AI systems can analyze historical billing data and identify patterns to optimize coding and improve reimbursement accuracy. These technologies have the potential to significantly enhance the efficiency and accuracy of medical billing processes.
Integration with healthcare systems
As healthcare systems become more interconnected, the integration of medical billing systems with other healthcare technology platforms is expected to increase. Seamless integration with EHRs, practice management systems, and revenue cycle management software will enable real-time data exchange, reducing duplication of efforts and improving billing accuracy. This integration will further streamline the billing process and enhance overall revenue cycle management.
Improved interoperability
Interoperability, the ability of different healthcare systems to exchange and use data, is a critical aspect of efficient medical billing. Efforts are being made to establish standardized data formats and protocols to promote interoperability between billing systems, insurance companies, and electronic health record systems. Improved interoperability will facilitate seamless data exchange between stakeholders, leading to more accurate and efficient medical billing processes.
Enhanced security and privacy measures
As the healthcare industry continues its digital transformation, security and privacy will remain paramount concerns in medical billing. Strong encryption methods, robust access controls, and advanced authentication techniques will be crucial for protecting patient data from unauthorized access or cyber threats. Continued advancements in security technology will ensure that medical billing systems remain secure and patient information remains confidential.
Training and Education for Medical Billers

Certifications and qualifications
Medical billing professionals have the opportunity to obtain various certifications and qualifications to enhance their skills and demonstrate their expertise. Some common certifications in medical billing include Certified Professional Biller (CPB) from the American Academy of Professional Coders (AAPC) and Certified Medical Reimbursement Specialist (CMRS) from the American Medical Billing Association (AMBA). These certifications validate the knowledge and proficiency of medical billers and provide a competitive edge in the job market.
Training programs and courses
Numerous training programs and courses are available to aspiring medical billers to acquire the necessary knowledge and skills for the field. These programs cover topics such as medical coding, billing regulations, insurance procedures, and billing software usage. Many educational institutions, vocational schools, and online platforms offer comprehensive training programs to prepare individuals for a career in medical billing.
Continuing education requirements
Medical billing professionals are encouraged to engage in continuing education to stay updated with the latest developments in the field. Professional organizations, such as the AAPC and AMBA, offer continuing education opportunities through seminars, webinars, conferences, and online courses. Continuing education helps medical billers stay current with evolving coding guidelines, regulatory changes, and best practices in medical billing.
Conclusion
In conclusion, medical billing plays a crucial role in the healthcare industry by ensuring accurate financial transactions, facilitating healthcare reimbursements, maintaining patient records, and supporting healthcare revenue cycle management. Medical billers have significant responsibilities, including verifying insurance coverage, accurately coding medical procedures, and submitting claims to insurance companies. The medical billing process involves several steps, such as patient demographics verification, medical coding, claim submission, payment posting, and appeals management. The adoption of medical billing software offers numerous benefits, including increased efficiency, improved accuracy, and faster reimbursement. Compliance in medical billing is essential to protect patient privacy, maintain coding accuracy, and prevent fraud. Current trends in medical billing include the transition to electronic medical records, the adoption of telehealth services, changing healthcare regulations, and the increasing complexity of medical coding. The future of medical billing involves the integration of automation and AI, improved interoperability, enhanced security measures, and the continued need for training and education for medical billers. By understanding the purpose and importance of medical billing, healthcare professionals can ensure efficient and accurate financial operations within their organizations.