In the complex realm of medical billing, having a solid understanding of Revenue Cycle Management (RCM) is crucial for healthcare professionals. RCM refers to the process of effectively managing the financial aspects of patient care, from the initial appointment to the final payment. By grasping the basics of RCM, healthcare providers can streamline their billing practices, maximize revenue, and ensure a seamless experience for both patients and healthcare organizations. This article will provide a concise overview of the fundamentals of RCM in medical billing, offering key insights and practical tips for professionals in the field.
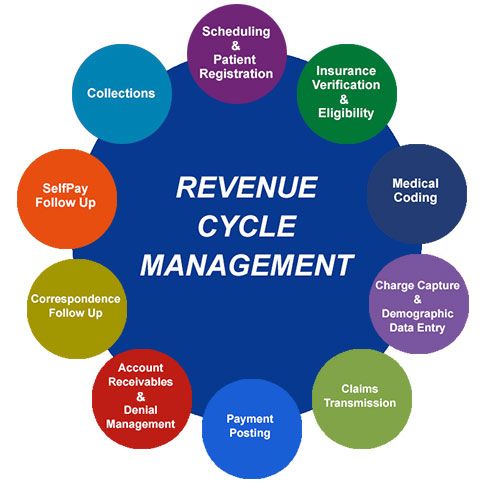
Definition of RCM in Medical Billing
Revenue Cycle Management (RCM) in medical billing refers to the process of managing financial transactions and capturing revenue for healthcare providers. It encompasses a series of steps that start from patient registration and extend to claims submission, payment processing, denial management, and accounts receivable follow-up. The primary goal of RCM is to streamline the entire revenue cycle to ensure timely and accurate reimbursement for healthcare services provided.
Components of RCM

This image is property of www.imagineteam.com.
Registration
The first step in the revenue cycle management process is patient registration. This involves gathering demographic and insurance information from the patient, verifying their eligibility and coverage, and entering the details into the system. Accurate and complete registration is crucial for generating clean claims and minimizing billing errors.
Charge Capture
Charge capture involves capturing and documenting all the services provided to a patient during their visit. This includes procedures, tests, medications, and other billable items. It is essential to ensure that all services rendered are recorded accurately to prevent underbilling or missing out on potential revenue.
Coding and Documentation
Coding and documentation is a critical component of RCM that involves assigning the appropriate medical codes to the services provided. Medical coders review the medical documentation to translate the diagnoses, procedures, and treatments into standardized codes, such as Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes. Accurate coding is vital for proper claims submission and reimbursement.
Claims Submission
After coding and documentation, the claims submission process begins. Healthcare providers compile the necessary information, including patient demographics, insurance details, and coded procedures, to generate claims. These claims are then submitted to the respective insurance companies or third-party payers for reimbursement. Timely and accurate claims submission is crucial to prevent delays in payment.
Payment Processing
Payment processing involves receiving and reconciling payments from insurance companies or patients. This includes posting payments, applying contractual adjustments, and handling any patient copayments or deductibles. Efficient payment processing ensures that providers receive the correct reimbursement for the services rendered.
Denial Management
Denial management is the process of handling claim denials and rejections. When claims are denied, healthcare providers need to identify the reason for the denial, rectify any errors, and resubmit the claim for reimbursement. effective denial management strategies are essential to minimize revenue losses and improve the overall financial health of the organization.
Accounts Receivable Follow-Up
accounts receivable follow-up involves tracking and managing unpaid or partially paid claims. Healthcare providers need to regularly follow up on outstanding claims, identify any issues causing delayed payments, and take appropriate actions to resolve them. Timely follow-up on accounts receivable ensures that providers receive the maximum reimbursement for their services.
Reporting and Analytics
Reporting and analytics play a crucial role in RCM. It involves generating financial reports, analyzing key performance indicators (KPIs), and identifying areas of improvement. Robust reporting and analytics help healthcare organizations gain insights into their revenue cycle, identify trends, and make informed decisions to optimize their financial performance.
Compliance
Compliance is an integral part of RCM in medical billing. Healthcare providers must adhere to various regulations, coding guidelines, and payer policies to ensure accurate and ethical billing practices. Compliance with these rules is essential to avoid legal and financial penalties.
Importance of RCM in Medical Billing
Effective revenue cycle management is essential for the financial viability and success of healthcare providers. It allows them to optimize their reimbursement processes, minimize billing errors, and maximize revenue. The benefits of implementing RCM include:
- Improved financial performance: Proper management of the revenue cycle helps healthcare providers optimize their revenue, resulting in better financial stability and profitability.
- Increased efficiency: RCM streamlines the billing and reimbursement processes, reducing administrative burdens and improving operational efficiency.
- Enhanced patient satisfaction: Efficient RCM ensures accurate and timely processing of claims, leading to faster reimbursements and reduced delays in patient billing, thus improving patient satisfaction.
- Compliance with regulations and policies: RCM helps healthcare providers stay updated with the constantly changing rules and regulations in the healthcare industry, ensuring compliance and minimizing the risk of legal and financial penalties.
Benefits of Implementing RCM
Implementing a comprehensive RCM system brings several benefits to healthcare providers. Some of the key benefits include:
- Increased revenue: By optimizing the revenue cycle and streamlining billing processes, healthcare organizations can maximize their reimbursement and revenue.
- Improved cash flow: Timely and accurate claims submission, payment processing, and accounts receivable follow-up help speed up cash flow, ensuring a steady revenue stream.
- Enhanced operational efficiency: RCM automates manual processes, reduces paperwork, and improves staff productivity, resulting in better operational efficiency.
- Reduced billing errors and claim denials: Effective RCM strategies minimize billing errors and denials, leading to quicker reimbursement and reduced revenue leakage.
- Better financial management: With robust reporting and analytics tools, healthcare providers can gain insights into their financial performance, identify bottlenecks, and plan strategies for better financial management.
Challenges in RCM
While revenue cycle management is crucial for healthcare providers, there are several challenges they may face in the process:
Changing Regulations and Policies
Healthcare regulations and payer policies are constantly evolving, making it challenging for providers to stay updated and ensure compliance. Keeping track of these changes and implementing necessary updates in the billing processes can be a complex task.
Complex Coding and Documentation
Proper coding and documentation are essential for accurate claims submission and reimbursement. However, the complexity of medical coding and documentation requirements can pose challenges for healthcare providers, leading to coding errors and claim denials.
Denials and Claim Rejections
Claim denials and rejections can have a significant impact on the revenue cycle. Providers must invest time and resources in identifying the reasons for denials, rectifying errors, and resubmitting claims, adding to the administrative burden and delaying reimbursement.
Incomplete or Inaccurate Patient Information
Incomplete or inaccurate patient information can lead to billing errors, claim denials, and delayed reimbursements. Verifying patient demographic and insurance details during the registration process is crucial to ensure clean claims and minimize billing issues.
Evolving Technology and Software Solutions
The healthcare industry constantly embraces new technology and software solutions to improve efficiency and patient care. However, keeping up with these technological advancements and implementing the right tools can be challenging for healthcare organizations.
Best Practices for Effective RCM
To overcome the challenges and optimize their revenue cycle, healthcare providers can implement the following best practices:
Streamline Patient Registration
Implementing automated patient registration processes, including online forms and electronic eligibility verification, can ensure accurate and complete patient information, leading to cleaner claims and reduced billing errors.
Improve Coding and Documentation Processes
Healthcare organizations should invest in training and education for their coding and documentation staff. Regular audits and quality checks can help identify areas for improvement and ensure accurate coding and documentation, minimizing claim denials.
Enhance Claims Submission and Follow-Up
Automating claims submission processes, using clearinghouses, and establishing robust follow-up systems can accelerate reimbursement cycles and reduce the administrative burden associated with managing claims.
Implement Robust Denial Management Strategies
Developing effective denial management strategies, including denials tracking, analysis of denial trends, and proactive measures to prevent recurring denials, can significantly reduce revenue losses and improve the financial performance of healthcare organizations.
Optimize Payment Processing and Accounts Receivable
Implementing electronic payment solutions, such as electronic remittance advice (ERA), and leveraging technology to handle payment posting and accounts receivable follow-up, can streamline the payment processing workflow and improve cash flow.
Utilize Reporting and Analytics Tools
Healthcare providers should invest in robust reporting and analytics tools that provide real-time data on key performance indicators (KPIs), allowing them to monitor financial performance, identify trends, and make data-driven decisions for process improvement.
Stay Updated with Compliance Requirements
Healthcare organizations must allocate resources to stay updated with the latest healthcare regulations, coding guidelines, and payer policies. Regular training and education sessions for staff can ensure compliance and minimize the risk of legal and financial penalties.
Continuously Train and Educate Staff
Investing in ongoing training and education for staff members involved in the revenue cycle can help improve their skills and knowledge, leading to more accurate coding, documentation, and billing practices.
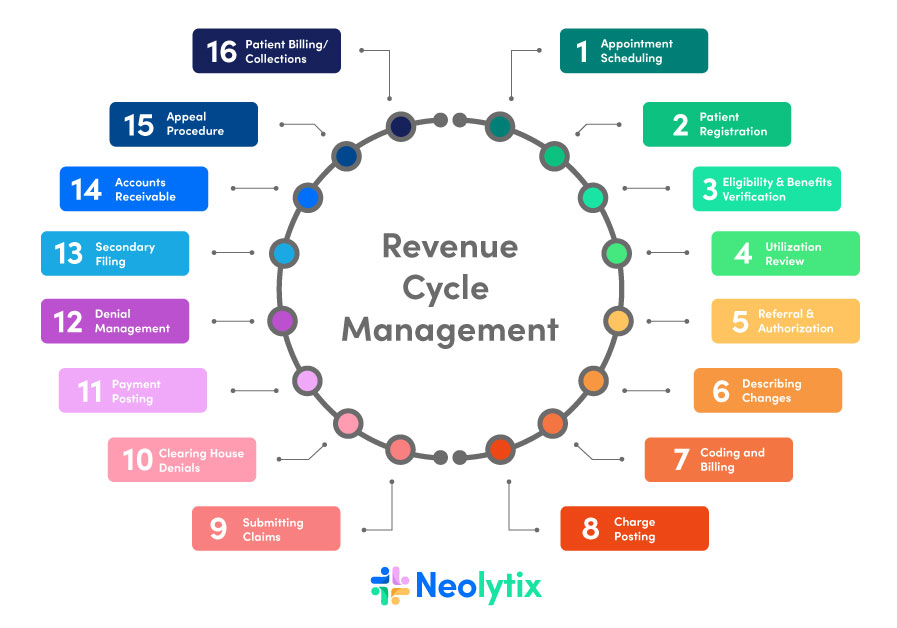
This image is property of neolytix.com.
RCM Software and Tools
To support effective revenue cycle management, healthcare organizations can utilize various software and tools:
Electronic Health Record (EHR) Systems
EHR systems play a critical role in RCM by capturing and storing patient health information, facilitating coding and documentation, and supporting clinical decision-making. Integrated EHR systems streamline the billing process and improve accuracy and efficiency.
Practice Management Systems
Practice management systems are comprehensive software solutions that assist in managing administrative and financial operations in healthcare organizations. These systems include features such as scheduling, billing, and reporting, enabling efficient revenue cycle management.
Medical Coding Software
Medical coding software automates the coding process, reducing errors and improving coding accuracy. These tools provide a user-friendly interface for coders to assign appropriate codes based on the documentation, making the coding and documentation process more efficient.
Clearinghouses
Clearinghouses are intermediaries between healthcare providers and insurance companies. They validate and format claims before forwarding them to payers, reducing errors and improving the chances of reimbursement.
Revenue Cycle Management Software
RCM software integrates various components of the revenue cycle, providing a unified platform for managing patient registration, charge capture, claims submission, payment processing, denial management, and accounts receivable follow-up. These tools automate and streamline the entire RCM process, improving efficiency and revenue.
Outsourcing RCM Services
For healthcare organizations that lack the resources or expertise to manage the revenue cycle effectively, outsourcing RCM services can be a viable option. Outsourcing allows providers to leverage the expertise and technology of dedicated RCM service providers, resulting in better financial outcomes and reduced administrative burden.
Future Trends in RCM
As the healthcare industry continues to evolve, several trends are shaping the future of revenue cycle management:
Artificial Intelligence (AI) and Automation
AI and automation are revolutionizing healthcare operations, including RCM. Machine learning algorithms can assist in coding and reviewing claims for accuracy, automating routine tasks, and improving overall efficiency and accuracy in revenue cycle processes.
Blockchain Technology
Blockchain technology has the potential to transform RCM by providing secure and transparent transactions, reducing third-party intermediaries, and streamlining the claims settlement process. Implementing blockchain in RCM can enhance data security, reduce fraud, and improve the speed of reimbursement.
Telehealth and Remote Patient Monitoring
The rise of telehealth and remote patient monitoring is changing the way healthcare services are delivered. These technologies offer new opportunities for revenue cycle management, including improved remote documentation, virtual claims submission, and efficient reimbursement processes.
Conclusion
Revenue Cycle Management is a critical aspect of medical billing that encompasses various components and processes. By implementing effective RCM strategies and utilizing the right software and tools, healthcare organizations can optimize their revenue, improve cash flow, reduce billing errors, and enhance their overall financial performance. Staying updated with evolving regulations, training and educating staff, and embracing future trends in RCM will ensure the successful management of the revenue cycle in the ever-changing healthcare landscape.