In the world of medical coding, it is crucial to know the distinction between a CPC and a COC medical coder. The Comparative Trial Pharmaceuticals (CPC) and the Center for Occupational Certifications (COC) both play essential roles in the healthcare industry, but their responsibilities and expertise differ significantly. Understanding the variations between these two types of medical coders is vital for medical professionals and institutions to ensure accurate and efficient coding processes. In this article, we will explore the disparities between a CPC and a COC medical coder, providing valuable insights into the unique skill sets and qualifications required for each role.
Education and Certification
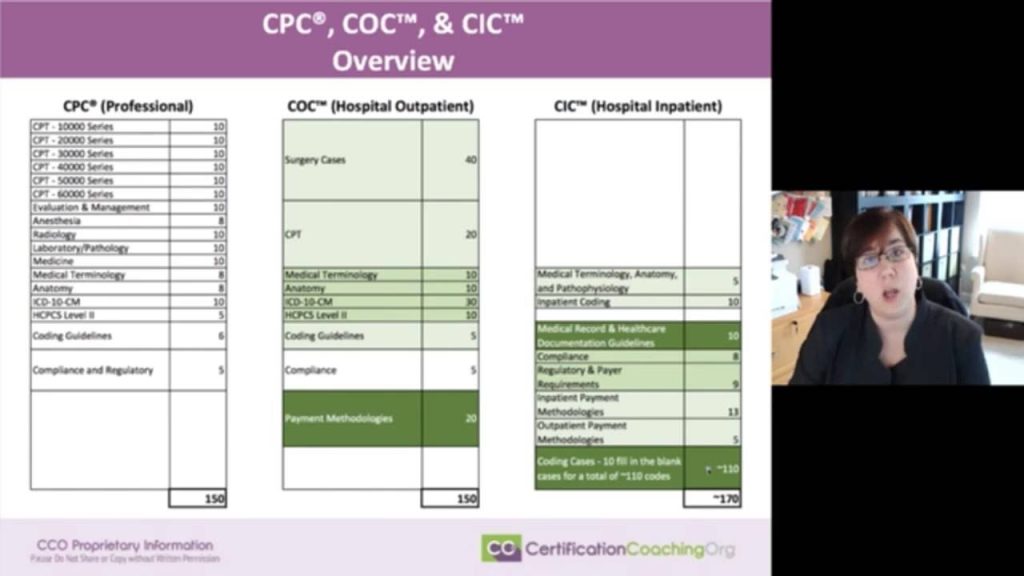
This image is property of www.cco.us.
CPC Education and Certification
To become a Certified Professional Coder (CPC), you must complete the required education and obtain certification through the American Academy of Professional Coders (AAPC). The education for CPC covers in-depth knowledge of medical coding principles and guidelines, anatomy, physiology, medical terminology, and medical procedures. It typically requires completing a coding program or having two years of coding experience. After completing the education, you need to pass the CPC exam, which tests your coding skills and knowledge.
COC Education and Certification
On the other hand, to become a Certified Outpatient Coder (COC), you need to focus more on outpatient coding skills. The education for COC includes learning about outpatient coding guidelines, billing procedures, and reimbursement processes. This specialization allows you to work in outpatient facilities like clinics, ambulatory surgical centers, and emergency departments. To obtain COC certification, you must complete the required education and pass the COC exam conducted by the AAPC.
Job Responsibilities

CPC Job Responsibilities
As a CPC, your primary responsibility is to ensure accurate coding and documentation of medical services rendered by healthcare providers. You will review medical records, abstract information, assign appropriate codes using Current Procedural Terminology (CPT), and International Classification of Diseases (ICD) coding systems. CPCs work in various healthcare settings, such as hospitals, physician offices, and insurance companies, ensuring compliance with coding guidelines and regulations.
COC Job Responsibilities
As a COC, your job responsibilities primarily involve outpatient coding. You will review medical records for outpatient visits, surgeries, and procedures, ensuring that the appropriate codes for billing and reimbursement are assigned accurately. COCs need to stay updated with the latest coding guidelines and regulations specific to outpatient services. They often collaborate with healthcare providers and insurance companies to ensure proper documentation and coding accuracy.
Specializations
CPC Specializations
CPCs have the opportunity to specialize in a particular field within the medical coding profession. Some of the common CPC specializations include anesthesia, cardiology, orthopedics, and evaluation and management. Specializing in a specific field allows CPCs to develop expertise and in-depth knowledge in that area, making them valuable assets to organizations focusing on those specialties.
COC Specializations
Although COCs primarily focus on outpatient coding, they also have specializations within this field. COC specialties may include ambulatory surgical centers (ASC), emergency department coding, or professional fee coding. These specializations enable COCs to develop expertise in specific areas of outpatient coding, making them highly sought after in facilities that specialize in these areas.
Coding Guidelines

CPC Coding Guidelines
CPC coders must adhere to specific coding guidelines when assigning codes to medical procedures and services. These guidelines ensure consistency and accuracy in medical coding. CPCs follow the Current Procedural Terminology (CPT) guidelines, which provide detailed instructions on how to select the appropriate code for a given medical procedure. Additionally, they need to follow the International Classification of Diseases (ICD) guidelines to assign the correct diagnosis codes.
COC Coding Guidelines
COC coders also follow coding guidelines but focus more on outpatient services. They need to be well-versed in the rules and regulations specific to outpatient coding. COCs may use the CPT guidelines to assign codes for outpatient procedures and services, along with other specific coding guidelines related to outpatient visits, surgeries, and procedures.
Coding Systems
This image is property of i.ytimg.com.
CPC Coding Systems
CPCs utilize two main coding systems for accurate representation of medical procedures and diagnoses. They use the Current Procedural Terminology (CPT) coding system, which contains codes for procedures and services performed by healthcare providers. Additionally, CPCs use the International Classification of Diseases (ICD) coding system to assign diagnosis codes. These coding systems ensure standardized communication between healthcare providers, insurance companies, and other entities involved in the healthcare industry.
COC Coding Systems
Similar to CPCs, COCs also rely on the CPT and ICD coding systems. However, COCs focus more on outpatient procedures and services, utilizing these coding systems specific to outpatient care. They assign codes from the CPT system for outpatient procedures and services, while also using the ICD system for diagnosis coding related to outpatient visits and treatments.
Reimbursement Processes
CPC Reimbursement Processes
CPCs play a crucial role in the reimbursement process for healthcare providers. They ensure accurate coding and documentation, which directly impacts the reimbursement received for medical services. CPCs work closely with insurance companies, reviewing claims, and providing necessary documentation to support the assigned codes. They play a significant role in optimizing coding accuracy to ensure proper reimbursement for healthcare services.
COC Reimbursement Processes
COCs are also involved in the reimbursement process, particularly within the outpatient setting. They are responsible for assigning appropriate codes for outpatient procedures and services to facilitate proper billing and reimbursement. COCs collaborate with healthcare providers, insurance companies, and other stakeholders to ensure accurate documentation and coding, maximizing the reimbursement received for outpatient services.
Coding Accuracy
This image is property of i.ytimg.com.
CPC Coding Accuracy
Coding accuracy is of utmost importance for CPCs to ensure proper reimbursement, compliance with regulations, and efficient healthcare operations. CPCs must have in-depth knowledge of coding guidelines, procedures, and medical terminologies to assign codes accurately. They audit medical records, perform coding validations, and conduct quality assessments to maintain high coding accuracy standards. This ensures that the codes assigned reflect the medical services provided accurately.
COC Coding Accuracy
COCs also prioritize coding accuracy, particularly for outpatient procedures and services. They must understand the specific guidelines for outpatient coding to assign appropriate codes. COCs review medical records, collaborate with healthcare providers, and conduct coding audits to ensure codes are assigned with precision. Accuracy in outpatient coding is crucial for proper reimbursement and documentation, making coding accuracy a significant focus for COCs.
Employment Settings
CPC Employment Settings
CPCs have a range of employment settings to choose from. They can work in hospitals, clinics, physician offices, insurance companies, or billing companies. CPCs are highly sought after in healthcare organizations as they play a vital role in accurate coding and billing practices. They also have the flexibility to work remotely as medical coding and documentation can often be done electronically.
COC Employment Settings
COCs primarily work in outpatient healthcare settings. They can be employed in clinics, ambulatory surgical centers, emergency departments, or outpatient departments within hospitals. COCs are responsible for assigning codes to outpatient visits, procedures, and surgeries, making them integral to outpatient billing and reimbursement processes.
Career Advancement
CPC Career Advancement
As a CPC, there are numerous opportunities for career advancement. With experience and expertise, CPCs can move into management roles, such as coding managers or compliance officers. They can also pursue careers in medical auditing or medical coding education, sharing their knowledge and skills with aspiring coders. CPCs may choose to specialize further in a particular medical field, enhancing their career prospects and earning potential.
COC Career Advancement
COCs can also progress in their careers by gaining experience and expanding their knowledge in outpatient coding. They can take on leadership positions within outpatient healthcare facilities or specialize in specific areas such as professional fee coding or ambulatory surgical centers. There are opportunities to become coding managers, educators, or even consultants, utilizing their expertise to improve outpatient coding practices.
Salary

CPC Salary
The salary of a CPC can vary depending on factors such as experience, geographic location, and employment setting. According to the AAPC Salary Survey, the average salary for a CPC is around $54,000 per year. However, salaries can range from $38,000 to over $74,000, with experienced coders and those in managerial positions earning higher salaries. Additional certifications, specializations, and advanced coding skills can also contribute to higher earning potential.
COC Salary
Similarly, the salary of a COC is influenced by various factors, including experience, location, and job responsibilities. According to the AAPC Salary Survey, the average salary for a COC is approximately $47,000 per year. However, depending on the aforementioned factors, COCs can earn between $36,000 and $61,000 annually. Advancing in their career, gaining expertise in specific outpatient coding areas, and obtaining additional certifications can positively impact their earning potential.
In conclusion, both CPCs and COCs play critical roles in the healthcare industry, ensuring accurate coding, proper reimbursement, and efficient healthcare operations. While CPCs focus on comprehensive medical coding, COCs specialize in outpatient coding. The education, certifications, job responsibilities, and skills required for these two roles may differ, but they are equally important in maintaining the integrity of healthcare coding and documentation processes.