Clinical coding is an essential component of the healthcare system, providing a standardized method of classifying diagnoses, procedures, and treatments. As a crucial part of medical documentation, clinical coding ensures accurate documentation and efficient communication between healthcare professionals, insurance companies, and regulatory bodies. By assigning specific codes to medical information, clinical coders play a pivotal role in facilitating medical research, tracking healthcare trends, and ensuring proper reimbursement for services provided. Understanding the basics of clinical coding is not only vital for healthcare professionals but also for patients who rely on accurate coding for a comprehensive understanding of their medical history and treatment.
Overview of Clinical Coding

Definition of Clinical Coding
Clinical coding is a vital process in healthcare that involves the transformation of medical diagnoses, procedures, and other healthcare services into standardized codes. These codes are used for various purposes such as medical documentation, billing, statistical analysis, and research. Clinical coders play a crucial role in ensuring accurate and consistent coding, which is essential for efficient healthcare operations.
Importance of Clinical Coding
accurate clinical coding is essential for a wide range of reasons. Firstly, it is crucial for proper reimbursement of healthcare services. Insurance companies and government payers rely on coded information to determine the amount of reimbursement healthcare providers should receive. Additionally, clinical coding plays a crucial role in capturing accurate healthcare data, which is essential for medical research, public health monitoring, and healthcare planning. Proper coding also helps in improving the overall quality and safety of patient care by ensuring that relevant information is accurately recorded and communicated.
Role of Clinical Coders
Clinical coders are essential members of the healthcare team who are responsible for assigning appropriate codes to medical diagnoses and procedures based on the provided documentation. These professionals possess in-depth knowledge of medical terminology, anatomy, physiology, and coding guidelines. They review medical records, interpret physician documentation, and select the most accurate codes. Clinical coders also collaborate with physicians and other healthcare professionals to clarify any ambiguous or incomplete documentation. Their attention to detail and expertise in coding standards ensure accurate and consistent coding, which is vital for efficient healthcare operations and optimal patient care.
Classification Systems
Clinical coding is facilitated by the use of standardized classification systems, the most widely used being the International Statistical Classification of Diseases and Related Health Problems (ICD). The ICD provides a comprehensive framework for classifying diseases, injuries, and other health conditions. The current edition, ICD-10, is widely used worldwide. In addition to the ICD, other coding systems such as Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) are used for coding medical procedures and services.
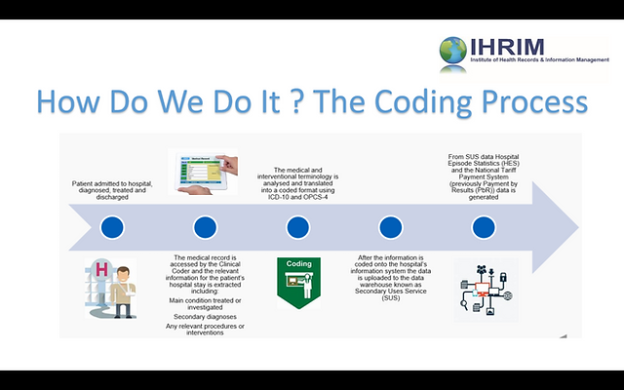
Clinical Coding Process

Medical Documentation
The clinical coding process begins with the review of medical documentation, which includes various types of healthcare records such as physician notes, test results, and operative reports. Clinical coders carefully analyze these records to extract relevant information regarding the patient’s diagnosis, procedures performed, and other pertinent details.
Code Selection
Once the necessary information has been extracted from the medical documentation, clinical coders proceed to assign appropriate codes. This involves matching the documented diagnoses and procedures to the corresponding codes within the classification system being used. The selection of accurate codes requires a deep understanding of coding guidelines, conventions, and the specific requirements of the coding system employed.
Code Validation
After assigning the initial codes, clinical coders conduct a thorough review and validation process to ensure the accuracy and appropriateness of the codes assigned. This may involve cross-referencing the codes with the corresponding documentation and conducting additional research if necessary.
Error Correction
In cases where errors or discrepancies are identified during the validation process, clinical coders are responsible for making the necessary corrections. This may involve revisiting the medical documentation, consulting with healthcare professionals for clarification, or seeking additional resources and references to resolve any coding uncertainties.
ICD-10-CM
Introduction to ICD-10-CM
ICD-10-CM is the clinical modification of the International Classification of Diseases, Tenth Revision (ICD-10) specifically designed for coding diagnoses in the United States. It provides a standardized system for classifying and coding diseases, injuries, and other health conditions. ICD-10-CM codes are alphanumeric and more detailed compared to its predecessor, ICD-9-CM.
Structure of ICD-10-CM
ICD-10-CM codes are structured hierarchically. The codes begin with a letter, followed by two digits representing the category, three digits representing the subcategory, and additional digits for specificity. This hierarchical structure allows for a more granular classification of diseases and conditions, providing greater detail and accuracy in coding.
Coding Guidelines
ICD-10-CM coding guidelines provide specific instructions and rules for assigning codes. These guidelines outline instructions for coding categories, sequencing codes, coding conventions, and other important considerations. It is vital for clinical coders to adhere to these guidelines to ensure accurate and consistent coding.
Code Categories and Subcategories
ICD-10-CM is organized into various categories and subcategories that cover a wide range of diseases, injuries, and health conditions. Each category or subcategory represents a specific body system or condition. For example, category G00-G99 represents diseases of the nervous system. Within each category, there are further subdivisions to provide greater specificity. Clinical coders must navigate these categories and subcategories to accurately assign the most appropriate code based on the documentation provided.
ICD-10-PCS
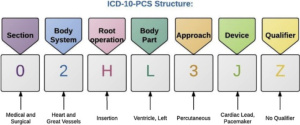
Introduction to ICD-10-PCS
ICD-10-PCS stands for International Classification of Diseases, Tenth Revision, Procedure Coding System. Unlike ICD-10-CM, which focuses on diagnoses, ICD-10-PCS is specifically designed for coding medical procedures and interventions. It provides a standardized system for recording the details of surgical, diagnostic, and therapeutic procedures performed in healthcare settings.
Structure of ICD-10-PCS
ICD-10-PCS codes are structured differently compared to ICD-10-CM. Each code is comprised of seven characters, each representing a specific aspect of the procedure performed. These characters represent the body system or general procedure, root operation, body part, approach, device, qualifier, and extension. This detailed structure allows for the precise classification and coding of medical procedures.
Medical and Surgical Section
ICD-10-PCS is divided into several sections to facilitate the coding of different types of procedures. The most relevant sections for clinical coders include the Medical and Surgical section, which encompasses a wide range of surgical and non-surgical procedures performed in healthcare settings. Each section provides a detailed breakdown of procedures according to body system, making it easier for clinical coders to locate the appropriate codes.
Procedures, Devices, and Qualifiers
ICD-10-PCS codes not only capture the procedure performed but also provide additional information about the devices used and any qualifiers associated with the procedure. This additional specificity allows for accurate coding and billing, as well as improved statistical analysis and research capabilities. Clinical coders must carefully review the documentation to capture all relevant details and select the appropriate codes accordingly.
CPT Coding
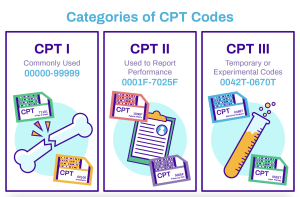
Overview of CPT Coding
The Current Procedural Terminology (CPT) coding system is used for coding medical procedures and services in the United States. Developed and maintained by the American Medical Association (AMA), CPT codes provide a comprehensive and uniform language for reporting medical procedures performed by healthcare professionals.
CPT Code Structure
CPT codes consist of five digits, each representing a specific aspect of the procedure or service provided. The first digit represents the main section of the CPT code, while each subsequent digit provides further specificity. CPT codes are organized into sections, subsections, and categories to facilitate easy navigation and accurate coding.
Evaluation and Management Codes
One of the essential components of CPT coding is the evaluation and management (E/M) codes. These codes capture the services provided during patient encounters such as office visits, hospital visits, and consultations. E/M codes are categorized into different levels, which depend on the complexity and intensity of the patient encounter.
Surgical Codes
CPT coding also includes a variety of surgical codes that capture specific procedures performed by surgeons and other healthcare professionals. These codes cover a broad range of surgical interventions, both minor and major, and provide detailed information about the procedure itself, any associated services, and modifiers that may affect reimbursement.
DRG Coding

Definition of DRG Coding
Diagnosis-related group (DRG) coding is a classification system used for grouping inpatient hospital stays into categories based on similar clinical characteristics and resource utilization. DRG coding is primarily used for determining reimbursement rates for hospital inpatient services.
Purpose of DRG Coding
The main purpose of DRG coding is to establish a standardized method for classifying and reimbursing hospital services. By grouping similar cases together, DRG coding streamlines the billing and reimbursement process while also providing a means for evaluating the quality and efficiency of care provided.
DRG Classification System
DRGs are organized into a hierarchical structure that groups related diagnoses and procedures. Each DRG has a specific payment weight assigned to it, representing the average cost of treating patients with that particular diagnosis. The DRG classification system allows for the fair and consistent reimbursement of hospital services based on the complexity and resources required for each case.
Reimbursement Based on DRGs
Hospitals are reimbursed based on the DRG assigned to each inpatient stay. The reimbursement amount is determined by multiplying the hospital’s base payment rate by the weight assigned to the DRG. This payment system incentivizes hospitals to provide efficient and cost-effective care, as higher-cost cases may impact the hospital’s financial performance. Accurate DRG coding is crucial for ensuring fair reimbursement and financial stability for healthcare facilities.
HCPCS Level II

Introduction to HCPCS Level II
The Healthcare Common Procedure Coding System (HCPCS) Level II is a standardized coding system used for reporting medical procedures, services, and supplies not covered by CPT codes. HCPCS Level II codes are primarily used for billing Medicare, Medicaid, and other federal healthcare programs.
Structure of HCPCS Level II Codes
HCPCS Level II codes are alphanumeric and consist of one letter followed by four digits. The letter at the beginning indicates the category of the service or supply being coded. The digits provide additional specificity and details about the particular item or service.
Types of HCPCS Level II Codes
HCPCS Level II codes cover a wide range of medical services and supplies, including durable medical equipment, prosthetics, orthotics, supplies, and certain medications. These codes are used to accurately document and bill for items and services that are not adequately represented by CPT codes alone.
Use in Medicare Billing
HCPCS Level II codes are essential for Medicare billing, as they provide a standardized language for reporting services and supplies. Medicare requires the use of HCPCS Level II codes when billing for procedures and supplies covered by the program. Accurate and compliant coding with HCPCS Level II ensures appropriate reimbursement and adherence to Medicare billing guidelines.
Code Books and Resources
ICD-10-CM Code Book
The ICD-10-CM code book is a fundamental resource for clinical coders working with diagnoses. It provides a comprehensive list of codes, their descriptions, and coding guidelines specific to ICD-10-CM. The code book also includes supplementary information such as code changes, conventions, and other relevant coding instructions.
ICD-10-PCS Code Book
For clinical coders working with procedures, the ICD-10-PCS code book is an essential resource. It provides an extensive range of codes, their definitions, and guidelines specific to ICD-10-PCS. The code book also includes tables, index references, and examples to assist coders in accurately assigning codes.
CPT Code Book
The CPT code book is the primary resource for clinical coders dealing with medical procedures and services. It contains a comprehensive list of CPT codes, their descriptions, and guidelines for accurate coding. The CPT code book also includes modifiers, appendixes, and instructional notes to provide additional guidance for coders.
DRG Code Book
The DRG code book is an essential resource for clinical coders involved in inpatient hospital coding. It includes the complete list of DRGs, their descriptions, and various evaluation parameters. The DRG code book also provides information on coding rules, reimbursement criteria, and other relevant information for accurate DRG coding.
Training and Certification

Clinical Coding Courses
To become a proficient clinical coder, individuals can pursue specialized training courses that provide comprehensive knowledge of coding systems, guidelines, and practices. These courses cover topics such as medical terminology, anatomy, coding conventions, and coding software. They also provide opportunities to develop practical coding skills through hands-on exercises and case studies.
Certification in Clinical Coding
Obtaining certification in clinical coding demonstrates proficiency and expertise in the field. Various organizations offer certification programs that assess knowledge, skills, and competency in clinical coding. Certification exams typically cover coding guidelines, documentation requirements, and coding accuracy. Holding a recognized certification enhances professional credibility and can lead to better job prospects and career advancement opportunities.
Continuous Education
Clinical coding is a constantly evolving field, with coding systems regularly updated and new coding challenges emerging. It is essential for clinical coders to engage in continuous education to stay updated with the latest coding guidelines and advancements. This may involve attending workshops, webinars, conferences, or pursuing advanced coding courses to enhance proficiency and ensure compliance with changing coding standards.
Challenges and Future Trends

Complexity and Updates
Clinical coding is a complex process that requires a deep understanding of medical terminology, coding guidelines, and documentation requirements. Keeping up with updates and changes in coding systems can be challenging, as new codes, guidelines, and conventions are regularly introduced. Clinical coders must invest time and effort into continuous learning and staying updated to maintain accuracy and compliance in coding practices.
Artificial Intelligence in Clinical Coding
The advent of artificial intelligence (AI) has the potential to revolutionize clinical coding processes. AI-powered coding systems and software can analyze medical documentation, identify relevant information, and assign accurate codes. This technology has the potential to improve coding efficiency, reduce errors, and streamline the coding workflow. However, the implementation of AI in clinical coding requires careful consideration of ethical, legal, and privacy implications.
Interoperability and Electronic Health Records
The transition to electronic health records (EHRs) has brought both opportunities and challenges in clinical coding. Interoperability among different EHR systems and coding software is crucial for seamless data exchange and accurate coding. Efforts to standardize coding systems and improve interoperability can enhance coding efficiency, reduce duplication of work, and improve data quality. However, challenges such as varying EHR platforms and non-standardized documentation practices need to be addressed to maximize the benefits of EHRs in clinical coding.
In conclusion, clinical coding plays a critical role in healthcare operations, reimbursement, and data analysis. Clinical coders, armed with in-depth knowledge of coding systems and guidelines, accurately assign codes to diagnoses and procedures, ensuring efficient healthcare delivery and optimal patient care. The utilization of standardized classification systems such as ICD-10-CM, ICD-10-PCS, CPT, and HCPCS Level II, along with comprehensive code books and resources, is essential for accurate coding. Continuous education, training, and certification opportunities further enhance the proficiency and credibility of clinical coders. Challenges such as the evolving complexity of coding systems, the integration of AI, and the need for interoperability pose both opportunities and hurdles for the future of clinical coding. By addressing these challenges and embracing technological advancements, clinical coding can continue to evolve and contribute to the improving landscape of healthcare.