In the complex world of medical billing, understanding the concept of bill types is essential. Bill type refers to a specific code that classifies the type of services provided, allowing healthcare providers to accurately communicate and process claims with insurance companies. Identifying the correct bill type is crucial for ensuring timely payments and preventing claim denials. In this article, you will gain a clear understanding of what bill types are in medical billing and why they are vital for efficient and accurate reimbursement.
Overview of Medical Billing
Medical cost concept with stethoscope and medical bill
Definition of medical billing
Medical billing refers to the process of submitting and following up on claims with health insurance companies in order to receive payment for services provided by healthcare providers. It involves translating medical procedures and diagnoses into standardized codes, compiling the necessary documentation, and submitting claims to insurance companies for reimbursement.
Importance of medical billing
Medical billing is a crucial aspect of the healthcare industry as it ensures that healthcare providers receive timely and accurate payment for the services they deliver. Efficient and accurate medical billing practices help to maintain the financial stability of healthcare organizations, allowing them to continue providing quality care to patients. Additionally, medical billing plays a vital role in maintaining compliance with healthcare regulations and ensuring healthcare providers are reimbursed appropriately for the services they render.
Key components of medical billing
- Patient demographics: Medical billing starts with capturing and verifying patient demographic information such as name, address, contact details, and insurance information. Accurate patient information is essential for successful claims submission and reimbursement.
- Coding: Medical coding involves assigning specific codes to medical procedures, diagnoses, and services. This ensures that healthcare services are accurately represented, facilitating proper billing and reimbursement processes.
- Claim submission: Once coding is completed, medical billing professionals compile all the necessary documentation and submit claims to insurance companies for reimbursement. This includes submitting claims electronically or in paper form, adhering to specific timelines and regulations.
- Follow-up and appeals: Medical billing professionals follow up with insurance companies on submitted claims to ensure prompt payment. In cases where claims are denied or not fully reimbursed, professionals may need to file appeals or resubmit claims with additional documentation to secure payment.
- Payment posting: Once reimbursement is received from insurance companies, accurate payment posting is crucial. Medical billing professionals match payments to claims, reconcile any discrepancies, and update patient accounts accordingly.
- Reporting and analysis: Medical billing also involves generating reports and analyzing billing data to identify trends, measure performance, and identify areas for improvement. This information helps healthcare organizations optimize their billing processes and financial outcomes.
Understanding Bill Types in Medical Billing
Definition of bill type
In medical billing, a bill type refers to a specific code that categorizes the type of healthcare service provided. It categorizes claims based on the setting or type of care, aiding in the reimbursement process and determining the appropriate payment rates.
Why bill types are used in medical billing
Bill types are used in medical billing for several reasons. Firstly, they help insurance companies classify claims and determine the appropriate reimbursement rates for specific services. Secondly, bill types allow healthcare organizations to keep track of the different types of services they provide and analyze reimbursement patterns.
How bill types impact the reimbursement process
Bill types play a significant role in the reimbursement process for healthcare providers. Insurance companies use bill types to determine the reimbursement rates for services rendered by healthcare providers. Each bill type corresponds to a specific payment methodology that outlines the reimbursement rates and guidelines for that particular service category. By assigning the correct bill type, healthcare providers can ensure they are reimbursed correctly and in a timely manner.
Types of Bill Types in Medical Billing
There are various types of bill types in medical billing, each corresponding to a specific type of healthcare service or setting. Understanding these bill types is crucial for accurately coding and billing claims. The following are some of the common bill types in medical billing:
Inpatient bill types
Inpatient bill types are used for services provided to patients who require admission to a hospital or other healthcare facility for a specific period. These bill types are used for comprehensive services, including room charges, ancillary services, surgical procedures, and medications provided during the inpatient stay.
Outpatient bill types
Outpatient bill types are used for services provided to patients who do not require admission to a healthcare facility and receive care on an outpatient basis. These bill types cover services such as clinic visits, diagnostic tests, minor surgical procedures, and outpatient therapies.
Professional bill types
Professional bill types are used for services provided by healthcare professionals that are not performed in a hospital or facility setting. These bill types include services rendered by physicians, nurses, therapists, and other licensed healthcare providers.
Durable Medical Equipment (DME) bill types
Durable Medical Equipment (DME) bill types are used for equipment or supplies that are medically necessary and prescribed by a healthcare provider. These bill types include items such as wheelchairs, oxygen tanks, prosthetic devices, and other durable medical equipment.
Laboratory bill types
Laboratory bill types are used for services provided by clinical laboratories, including blood tests, urine tests, genetic tests, and other laboratory procedures.
Home Health Agency bill types
Home Health Agency bill types are used for services provided to patients in their own homes by home health agencies. These bill types cover services such as skilled nursing care, physical therapy, home health aide services, and medical social services.
Skilled Nursing Facility bill types
Skilled Nursing Facility bill types are used for services provided to patients in skilled nursing facilities. These bill types cover services such as skilled nursing care, rehabilitation therapies, and room charges.
Hospice bill types
Hospice bill types are used for services provided to patients who are in the terminal stages of an illness and receiving hospice care. These bill types cover comprehensive services provided by hospice agencies, including medical care, pain management, counseling, and emotional support.
Ambulatory Surgical Center bill types
Ambulatory Surgical Center bill types are used for services provided in ambulatory surgical centers. These bill types include surgical procedures, diagnostic tests, and other services provided in an outpatient surgical setting.
Other bill types
In addition to the aforementioned bill types, there are various other bill types that cater to specific healthcare services or settings. These include mental health services, radiology services, emergency department services, and more.
Inpatient Bill Types

Definition of inpatient bill types
Inpatient bill types are specific codes used in medical billing to categorize services provided to patients who require admission to a hospital or other healthcare facility for a specific period. Inpatient bill types encompass various charges during the time a patient is admitted, including room charges, ancillary services, surgical procedures, and medications.
Examples of inpatient bill types
Some common examples of inpatient bill types include:
- Bill Type 111: Hospital Inpatient Part A General Classification.
- Bill Type 121: Hospital Inpatient Part B Inpatient Only for Medical Certification.
- Bill Type 131: Hospital Inpatient Part B Inpatient Only.
Reimbursement considerations for inpatient bill types
When submitting claims with inpatient bill types, healthcare providers should ensure that all necessary documentation, including medical records and surgical reports, are included to support the claim. The reimbursement for inpatient services is typically based on a diagnosis-related group (DRG) system, where specific payment rates are assigned based on the patient’s diagnosis, procedures performed, and length of stay. Healthcare providers should accurately code and document these factors to ensure appropriate reimbursement. Additionally, understanding the various rules and regulations associated with inpatient billing, such as Medicare guidelines, is essential to maximize reimbursement for inpatient services.
Outpatient Bill Types

Definition of outpatient bill types
Outpatient bill types are specific codes used in medical billing to categorize services provided to patients who receive care on an outpatient basis, without the need for admission to a healthcare facility. Outpatient bill types include services such as clinic visits, diagnostic tests, minor surgical procedures, therapeutic services, and more.
Examples of outpatient bill types
Examples of outpatient bill types include:
- Bill Type 131: Clinic or hospital department visit performed on an outpatient basis.
- Bill Type 141: Comprehensive outpatient rehabilitation facility.
- Bill Type 151: Hospital outpatient part B only.
Reimbursement considerations for outpatient bill types
Reimbursement for outpatient services is typically based on the Medicare Outpatient Prospective Payment System (OPPS), which assigns payment rates based on specific Current Procedural Terminology (CPT) codes and Ambulatory Payment Classifications (APCs). To ensure correct reimbursement, healthcare providers must accurately code procedures, diagnoses, and other relevant information. Additionally, understanding the specific guidelines and requirements set forth by insurance companies is crucial to avoid claim denials and maximize reimbursement for outpatient services.
Professional Bill Types
This image is property of www.verywellhealth.com.
Definition of professional bill types
Professional bill types are specific codes used in medical billing to categorize services provided by healthcare professionals outside of a hospital or facility setting. These bill types encompass services rendered by physicians, nurses, therapists, and other licensed healthcare providers.
Examples of professional bill types
Examples of professional bill types include:
- Bill Type 121: Physician services provided in an inpatient setting.
- Bill Type 131: Physician services provided in an outpatient setting.
- Bill Type 141: Physical therapy services.
- Bill Type 151: Ambulance services.
Reimbursement considerations for professional bill types
The reimbursement for professional services is typically based on the Medicare Physician Fee Schedule (MPFS), which assigns payments based on relative value units (RVUs) and specific conversion factors. Healthcare providers must accurately code procedures, evaluation and management services, and other professional services to ensure appropriate reimbursement. It is important to stay up-to-date with the latest coding guidelines and documentation requirements to maximize reimbursement for professional services.
Durable Medical Equipment (DME) Bill Types

Definition of DME bill types
Durable Medical Equipment (DME) bill types are specific codes used in medical billing to categorize medically necessary equipment or supplies prescribed by a healthcare provider. DME bill types encompass items such as wheelchairs, oxygen tanks, prosthetic devices, and other durable medical equipment.
Examples of DME bill types
Examples of DME bill types include:
- Bill Type 121: Prosthetic devices.
- Bill Type 131: Medical equipment.
- Bill Type 141: Orthotic devices.
Reimbursement considerations for DME bill types
When billing for DME, healthcare providers must ensure that all necessary documentation, including prescriptions and medical necessity forms, are included to support the claim. Reimbursement for DME is typically based on fee schedules or specific payment methodologies set by insurance companies or Medicare. Accurate coding and documentation are crucial to ensuring appropriate reimbursement for DME services.
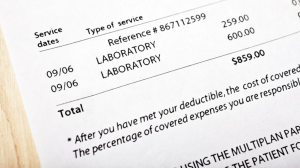
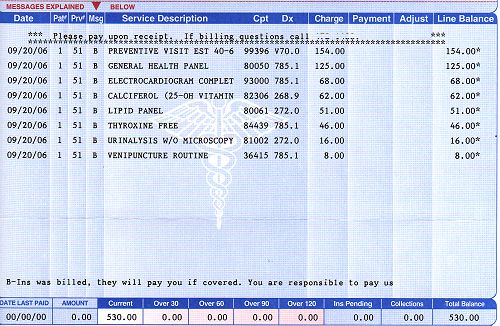
Laboratory Bill Types

Definition of laboratory bill types
Laboratory bill types are specific codes used in medical billing to categorize services provided by clinical laboratories. These bill types encompass a wide range of laboratory tests and procedures, including blood tests, urine tests, genetic tests, and other laboratory-based diagnostics.
Examples of laboratory bill types
Examples of laboratory bill types include:
- Bill Type 110: Independent laboratory testing.
- Bill Type 120: Independent laboratory specimen draw.
- Bill Type 130: Independent laboratory CLIA waiver.
Reimbursement considerations for laboratory bill types
Reimbursement for laboratory services is typically based on fee schedules or specific payment methodologies set by insurance companies or Medicare. Accurate coding and documentation of laboratory tests, appropriate use of modifiers when necessary, and adherence to specific guidelines are essential for proper reimbursement. Compliance with Clinical Laboratory Improvement Amendments (CLIA) regulations and ensuring proper documentation of medical necessity are also crucial for obtaining reimbursement for laboratory services.
Home Health Agency Bill Types
These bill types encompass a broad spectrum of care, spanning skilled nursing services, physical therapy, home health aide assistance, medical social services, and much more. Accurate and systematic utilization of these bill types is crucial for both healthcare providers and insurance companies to ensure proper reimbursement and transparent record-keeping of the care provided to patients in home health settings.
Definition of Home Health Agency bill types
Home Health Agency bill types are specific codes used in medical billing to categorize services provided to patients in their own homes by home health agencies. These bill types encompass a wide range of services, including skilled nursing care, physical therapy, home health aide services, medical social services, and more.
Examples of Home Health Agency bill types
Examples of Home Health Agency bill types include:
- Bill Type 323: Home health – part A.
- Bill Type 324: Home health – part B.
- Bill Type 329: Parenteral, enteral, and/or nutrition home care.
Reimbursement considerations for Home Health Agency bill types
Reimbursement for home health services is typically based on various factors, including the patient’s health condition, the services provided, and the payment methodology set by insurance companies or Medicare. Accurate coding and documentation of services, adherence to specific guidelines, and regular communication with the involved insurance companies are crucial for maximizing reimbursement for home health services.
Other Bill Types
Each bill type corresponds to a specific category of healthcare services, allowing for efficient and precise billing processes.
Definition of other bill types
Besides the specific bill types discussed above, there are various other bill types that cater to specific healthcare services or settings. These bill types may include mental health services, radiology services, emergency department services, and more.
Examples of other bill types
Examples of other bill types include:
- Bill Type 421: Mental health services.
- Bill Type 721: Radiology services.
- Bill Type 851: Emergency department services.
Reimbursement considerations for other bill types
Reimbursement considerations for these other bill types vary depending on the specific services provided and the payment methodologies set by insurance companies or Medicare. Healthcare providers must accurately code and document these services, ensuring compliance with specific guidelines, and understanding the reimbursement rules associated with each specific bill type to maximize reimbursement. Regular communication and collaboration with insurance companies and payers can help healthcare providers navigate the complexities of reimbursement for these services.
In conclusion, understanding the different bill types in medical billing is critical for accurate coding, billing, and reimbursement processes. From inpatient and outpatient bill types to professional services and specialized bill types for various settings, each category comes with its own unique considerations. Healthcare providers must stay informed about the specific requirements, guidelines, and payment methodologies associated with each bill type to optimize reimbursement and maintain financial stability in the ever-evolving landscape of medical billing.
