In the complex world of medical billing, it is crucial to understand the concept of a dirty claim. A dirty claim refers to a medical billing claim that is incorrect, incomplete, or contains errors, resulting in its rejection by insurance companies or delayed payments. These claims can have a significant impact on healthcare providers’ revenue and overall financial efficiency. This article will examine the common reasons behind dirty claims, explore their consequences, and provide valuable insights into how to avoid them in order to streamline the medical billing process.
Definition of a dirty claim
Basic description
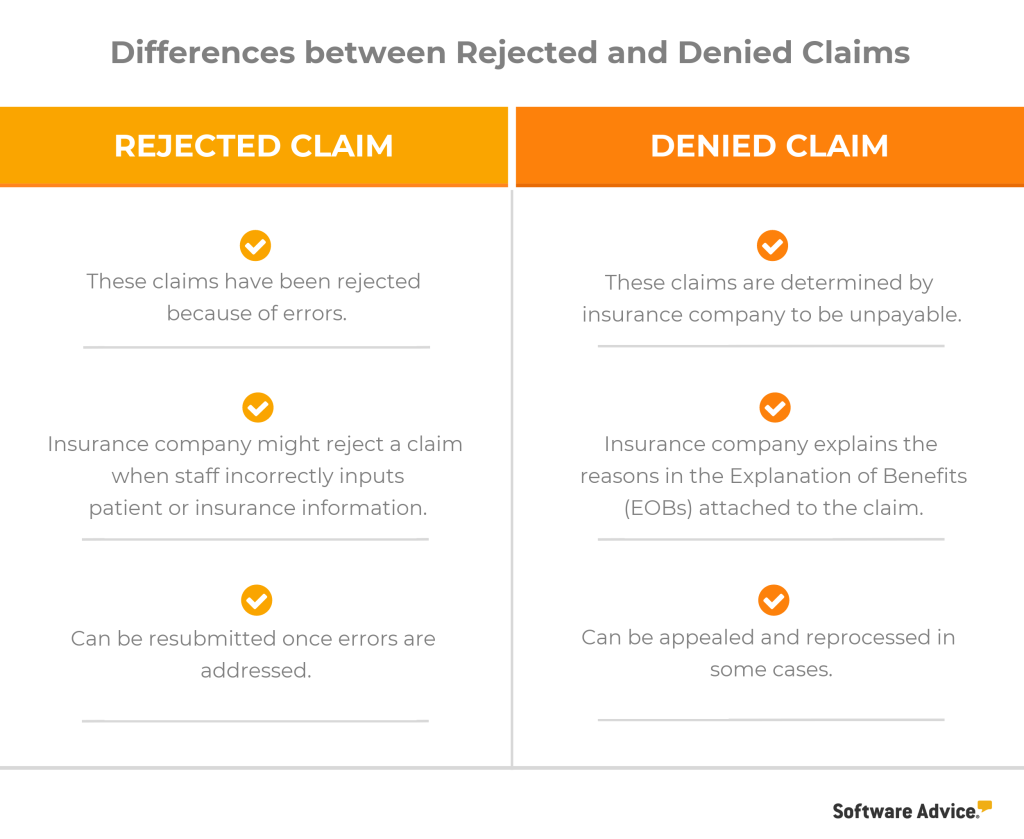
A dirty claim refers to a medical billing claim that is incomplete, inaccurate, or contains errors, making it difficult for healthcare providers or insurance companies to process and reimburse. These claims often fail to meet the submission requirements outlined by insurance companies, leading to delays, denials, and financial losses for healthcare providers.
Claim submission requirements
To submit a clean claim, certain requirements must be met. These requirements typically include accurate patient information, proper coding and billing procedures, correct documentation, compliance with medical necessity requirements, obtaining necessary authorizations, and timely filing. Failure to meet these requirements can result in a claim being classified as dirty.
Errors that classify a claim as dirty
Several errors can lead to a claim being classified as dirty. These errors include incomplete or inaccurate patient information, incorrect coding or billing, missing or invalid documentation, failure to meet medical necessity requirements, lack of proper authorization, duplicate claims, and untimely filing. These errors can cause significant issues in the billing process and hinder timely reimbursement.
Common causes of dirty claims

Incomplete or inaccurate patient information
One of the most common causes of dirty claims is incomplete or inaccurate patient information. This may include missing or incorrect demographic information, insurance details, or any other relevant information required for claim submission. Inaccurate information can lead to claim rejections or denials, delaying the reimbursement process.
Incorrect coding or billing
Incorrect coding or billing is another frequent cause of dirty claims. This involves using incorrect medical codes, modifiers, or billing information when submitting a claim. For example, using an incorrect procedure code or failing to include necessary diagnosis codes can result in a claim being flagged as dirty and subsequently denied or delayed.
Missing or invalid documentation
Dirty claims often occur when necessary documentation is missing or invalid. Proper documentation, such as medical records, test results, or referral letters, is essential for supporting the medical necessity of the services provided. Without complete and valid documentation, claims may be deemed dirty and rejected, leading to delays in reimbursement.
Failure to meet medical necessity requirements
Claims may also be classified as dirty if they fail to meet medical necessity requirements. Insurance companies require that services provided to patients are medically necessary and meet specific criteria. If healthcare providers fail to demonstrate medical necessity, the claim may be denied or classified as dirty.
Lack of proper authorization
Some healthcare services require prior authorization from insurance companies. If providers fail to obtain the necessary authorization before delivering services, claims may be labeled as dirty. This can lead to claim denials or delays in reimbursement.
Duplicate claims
Submitting duplicate claims is another common error that leads to dirty claims. Duplicate claims occur when the same service is billed multiple times for the same patient. Insurance companies closely monitor claims to identify duplicates, and if detected, these claims are classified as dirty and denied.
Untimely filing
Claims must be submitted within a specific timeframe specified by insurance companies. Failure to submit claims within the designated timeframe can result in claims being classified as dirty. Healthcare providers must adhere to timely filing guidelines to avoid delays or denials.
Impact of dirty claims on medical billing
Delayed reimbursement
One of the significant impacts of dirty claims is delayed reimbursement. When claims are labeled as dirty, they require additional processing and review, leading to delays in receiving payment for services provided. This can cause financial strain on healthcare providers and disrupt the cash flow of their practices.
Financial losses for healthcare providers
Dirty claims can result in significant financial losses for healthcare providers. Denied or delayed claims not only impact immediate revenue, but they can also lead to additional administrative costs associated with resubmissions, appeals, and follow-ups. These additional expenses can erode the profitability of healthcare organizations.
Increased claim denial rates
Dirty claims often have higher denial rates compared to clean claims. When claims do not meet the submission requirements or contain errors, they are more likely to be denied. Repeated denials can have a negative impact on the overall financial performance of healthcare providers.
Negative impact on patient satisfaction
Dirty claims can have a negative impact on patient satisfaction. When claims are denied or delayed, patients may be left with unexpected bills or disputes with insurance companies. This can cause frustration and dissatisfaction among patients, affecting the overall perception of the healthcare provider.
Administrative burden
Processing dirty claims requires additional administrative work for healthcare providers. From identifying errors to correcting them and resubmitting claims, the administrative burden involved in dealing with dirty claims can be time-consuming and resource-intensive. This can divert staff and resources away from other critical tasks, impacting overall productivity.
How to identify a dirty claim

Reviewing claim rejection and denial reports
One way to identify dirty claims is by reviewing claim rejection and denial reports. These reports provide valuable insights into the reasons for claim denials and rejections. By closely analyzing these reports, healthcare providers can identify patterns or recurring errors that classify claims as dirty.
Analyzing claim acceptance rate
Monitoring claim acceptance rate can also help identify dirty claims. A low acceptance rate indicates that a significant number of claims are being categorized as dirty. This may be an indication of errors or issues in the claim submission process.
Monitoring claim payment timelines
Monitoring claim payment timelines can help identify dirty claims that are leading to delayed reimbursement. If certain claims consistently take longer to process and receive payment, it could be an indication of issues that classify them as dirty.
Auditing claims for accuracy
Regularly auditing claims for accuracy is crucial in identifying dirty claims. By conducting internal audits, healthcare providers can identify errors, missing information, or any other factors that contribute to claims being classified as dirty. This allows for timely correction and resubmission of claims.
Tips to prevent dirty claims

Ensuring accurate patient information
Accurate patient information is key to preventing dirty claims. Healthcare providers should verify and update patient information at every visit, ensuring that demographics, insurance details, and contact information are accurate and up to date. Implementing electronic systems for data capture can help reduce errors in patient information.
Proper coding and billing procedures
Adhering to proper coding and billing procedures is crucial in preventing dirty claims. Healthcare providers should stay up to date with current coding guidelines and regulations to ensure accurate coding. Regular training sessions and quality control measures can help mitigate errors in the coding and billing process.
Thorough documentation and record keeping
Thorough documentation and record keeping are essential for preventing dirty claims. Healthcare providers should maintain complete and accurate medical records, including relevant test results, referrals, or any other documentation that supports the medical necessity of the services provided. This ensures that claims have proper documentation to substantiate the services billed.
Compliance with medical necessity requirements
Healthcare providers must ensure compliance with medical necessity requirements to prevent dirty claims. This involves understanding and documenting the medical necessity of services rendered, in alignment with insurance company guidelines. Clear documentation of the medical necessity reduces the risk of claims being denied or classified as dirty.
Obtaining necessary authorizations
To prevent dirty claims, healthcare providers should obtain necessary authorizations before delivering services. Prior authorization requirements should be thoroughly understood and implemented to ensure claims are not flagged as dirty due to a lack of proper authorization.
Implementing a claim scrubbing process
Implementing a claim scrubbing process can help prevent dirty claims. Claim scrubbing involves using specialized software or systems to review claims for errors, missing information, or inconsistencies before submission. This automated process helps catch issues and correct them before claims are sent to insurance companies.
Process of cleaning dirty claims

Identifying the cause of the dirty claim
The first step in cleaning dirty claims is identifying the cause of the classification. This involves reviewing the rejection or denial reasons provided by insurance companies or analyzing internal audit findings. Identifying the specific error or issue allows healthcare providers to take appropriate corrective measures.
Correcting errors and missing information
Once the cause of the dirty claim is identified, healthcare providers must correct the errors and missing information. This may involve updating patient information, revising coding or billing information, obtaining proper authorization, or providing missing documentation. It is crucial to ensure that all necessary information is accurate and complete.
Resubmitting the claim
After correcting errors and updating missing information, healthcare providers can resubmit the cleaned claim. It is important to follow the correct submission process and meet any deadlines or requirements specified by insurance companies. Resubmitting the claim promptly increases the chances of timely reimbursement.
Following up on the claim status
Following up on the claim status is essential to ensure the cleaned claim is processed and reimbursed. Healthcare providers should regularly monitor the progress of the claim and address any further issues or inquiries from insurance companies promptly. Following up helps avoid potential delays or denials and ensures a smoother resolution of the claim.
The role of technology in reducing dirty claims

Automated claim scrubbing software
Automated claim scrubbing software plays a significant role in reducing dirty claims. This technology reviews claims before submission, identifying errors, missing information, or any inconsistencies. By automatically flagging potential issues, claim scrubbing software helps healthcare providers correct errors and submit clean claims.
Artificial Intelligence in claims processing
Artificial Intelligence (AI) is increasingly being utilized in claims processing to reduce dirty claims. AI algorithms can analyze claim data, identify potential errors or patterns, and suggest corrections. This technology can streamline the process and minimize errors, leading to a reduction in dirty claims.
Electronic Health Records (EHR) systems
Electronic Health Records (EHR) systems contribute to reducing dirty claims by improving documentation and record-keeping processes. EHR systems allow healthcare providers to capture and store patient information electronically, reducing the risk of errors or missing information. Improved documentation accuracy leads to cleaner claims.
Real-time eligibility verification
Real-time eligibility verification is another technological advancement that helps reduce dirty claims. With real-time verification, healthcare providers can confirm patient insurance coverage, verify authorization requirements, and determine medical necessity before delivering services. This reduces the chances of claims being classified as dirty due to issues with eligibility or authorization.
Dirty claim statistics

Percentage of dirty claims in the healthcare industry
While specific statistics on the percentage of dirty claims vary, studies indicate that a significant portion of claims submitted in the healthcare industry are classified as dirty. According to industry estimates, dirty claims can account for anywhere from 14% to 30% of all claims submitted.
Most common types of errors leading to dirty claims
Some of the most common types of errors leading to dirty claims include incomplete or inaccurate patient information, incorrect coding or billing, missing or invalid documentation, and failure to meet medical necessity requirements. These errors often contribute to claim denials or delays.
Financial impact of dirty claims on healthcare organizations
The financial impact of dirty claims on healthcare organizations can be substantial. The costs associated with resubmissions, appeals, and administrative work required to clean dirty claims can result in significant financial losses. Furthermore, delayed or denied reimbursement can disrupt cash flow, impacting the overall financial stability of healthcare providers.
Conclusion
In conclusion, a dirty claim in medical billing refers to a claim that is incomplete, inaccurate, or contains errors that hinder the processing and reimbursement process. Dirty claims result from various errors, such as incomplete patient information, coding mistakes, missing documentation, and failure to comply with medical necessity requirements. These claims have detrimental effects on medical billing, leading to delayed reimbursement, financial losses for healthcare providers, increased claim denial rates, negative impact on patient satisfaction, and administrative burden.
To identify and prevent dirty claims, healthcare providers can review claim rejection and denial reports, analyze claim acceptance rates, monitor claim payment timelines, and conduct audits for accuracy. Implementing practices such as ensuring accurate patient information, proper coding and billing procedures, thorough documentation, compliance with medical necessity requirements, obtaining authorizations, and utilizing claim scrubbing processes can help prevent dirty claims.
The process of cleaning dirty claims involves identifying the cause of the claim’s classification, correcting errors and missing information, resubmitting the claim, and actively following up on its status. Technology plays a crucial role in reducing dirty claims, with automated claim scrubbing software, AI in claims processing, EHR systems, and real-time eligibility verification being effective tools.
Dirty claim statistics show that a substantial percentage of claims submitted in the healthcare industry are classified as dirty, and errors such as incomplete patient information and incorrect coding are common culprits. The financial impact on healthcare organizations can be significant, with additional costs and disruptions to cash flow.
In conclusion, prioritizing clean claims in medical billing is crucial for efficient reimbursement, patient satisfaction, and financial stability. Continuously improving claim submission processes and embracing technology advancements are essential to reducing the occurrence of dirty claims and optimizing the revenue cycle in healthcare organizations.
