Clinical coding plays a crucial role in the healthcare industry by translating medical diagnoses, procedures, and other healthcare services into a standardized language. Ensuring accuracy and consistency, clinical coding allows for effective communication and streamlined data management, facilitating proper patient care, billing, and research. By converting complex medical information into a structured code system, clinical coding contributes to a more efficient healthcare system and helps healthcare professionals make informed decisions based on accurate and comprehensive data.
Overview of Clinical Coding

Definition of Clinical Coding
Clinical coding is a crucial process in the healthcare industry that involves the translation of medical diagnoses, procedures, and resources into alphanumeric codes. These codes are used to classify and document patient encounters, facilitate efficient billing and reimbursement, support healthcare research and statistics, and ensure accurate medical documentation. By assigning specific codes to medical information, clinical coding plays a significant role in standardizing healthcare data.
Importance of Clinical Coding
Clinical coding is vital for several reasons. Firstly, it ensures that medical documentation is accurate and consistent, allowing healthcare professionals to communicate effectively and make informed decisions about patient care. Additionally, clinical coding facilitates efficient billing and reimbursement processes, enabling healthcare organizations to receive timely and appropriate payments for the services they provide. Moreover, it supports healthcare research and statistics, allowing for the analysis of trends, treatment outcomes, and the effectiveness of interventions.
Role of Clinical Coding in Healthcare

Ensure Accurate Medical Documentation
Clinical coding plays a pivotal role in ensuring accurate medical documentation. By assigning specific codes to diagnoses, procedures, and resources, clinical coders contribute to the standardization and consistency of health records. This standardized documentation not only aids in the effective communication of patient information among healthcare providers but also supports clinical decision-making and ensures continuity of care across different settings and providers.
Facilitate Efficient Billing and Reimbursement
Efficient billing and reimbursement are essential for the financial sustainability of healthcare organizations. Clinical coding enables accurate and timely billing by translating complex medical information into codes that represent the services provided. These codes are then used for claims submission to insurance companies or government reimbursement programs. By ensuring coding accuracy, clinical coders help healthcare organizations receive appropriate payments for their services and minimize the risk of claims rejection or denial.
Support Healthcare Research and Statistics
Clinical coding is a valuable tool for healthcare research and the generation of statistics. By coding medical information consistently and accurately, clinical coders create a standardized dataset that can be analyzed to identify patterns, trends, and outcomes. This data is essential for conducting epidemiological studies, monitoring population health, evaluating the effectiveness of interventions, and identifying areas for improvement in healthcare delivery. Accurate clinical coding contributes to the reliability and validity of research findings and helps inform evidence-based practice.
Clinical Coding Systems
International Classification of Diseases (ICD)
The International Classification of Diseases (ICD) is a globally recognized coding system used to classify and code diseases, injuries, and other health conditions. It provides a standardized framework for capturing and documenting medical information and supports the consistent reporting of diagnoses across healthcare settings. The latest version, ICD-10, is widely adopted and allows for greater specificity in coding. The upcoming transition to ICD-11 will bring further improvements in capturing healthcare data and enhancing clinical coding accuracy.
Current Procedural Terminology (CPT)
The Current Procedural Terminology (CPT) is a coding system developed by the American Medical Association to describe medical procedures and services provided by healthcare professionals. CPT codes are used for billing and reimbursement purposes in the United States. They provide a standardized language for describing medical procedures and services, allowing for the accurate and efficient communication of information between healthcare providers, payers, and regulatory bodies.
Healthcare Common Procedure Coding System (HCPCS)
The Healthcare Common Procedure Coding System (HCPCS) is another coding system used in the United States to describe and identify healthcare services, supplies, and equipment. HCPCS codes are used for billing and reimbursement purposes, particularly for services not covered by CPT codes. The system includes two levels of codes – Level I (which is the CPT codes) and Level II (which includes codes for items such as durable medical equipment, prosthetics, and supplies).
Clinical Coding Process

Patient Encounter and Documentation
The clinical coding process begins with the patient encounter and documentation of medical information. Healthcare professionals document the patient’s medical history, symptoms, diagnoses, procedures performed, and other relevant details. Accurate and comprehensive documentation is essential to ensure that all relevant information is captured and that clinical coders can assign the appropriate codes based on the medical record.
Code Assignment and Selection
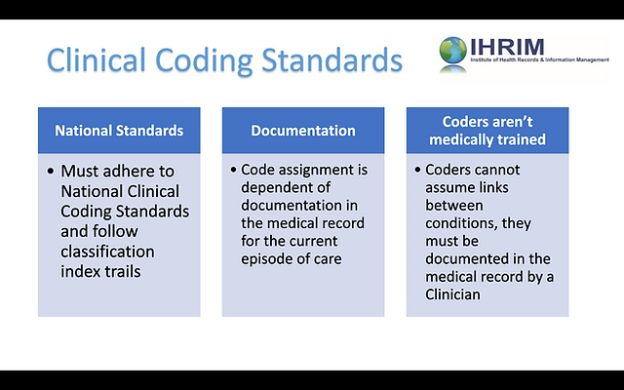
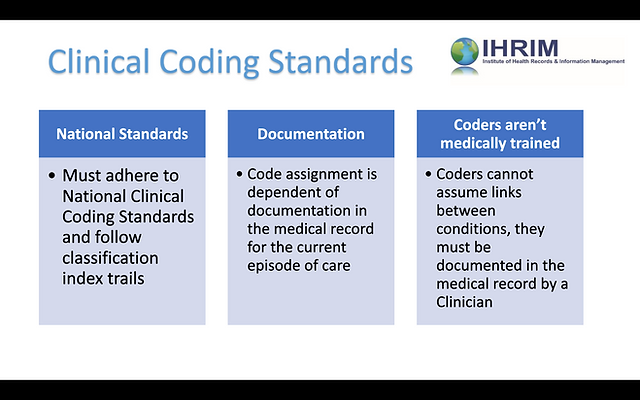
Once the patient’s information is documented, clinical coders analyze the medical record and assign the appropriate codes based on established coding guidelines. They identify and code the patient’s diagnoses, procedures, and resources used during the encounter. This process involves a deep understanding of coding systems, medical terminology, and coding guidelines to ensure accuracy and compliance with industry standards.
Quality Assurance and Compliance
To ensure coding accuracy, healthcare organizations implement quality assurance measures through regular audits and reviews. This includes assessing the accuracy and completeness of coded data, ensuring compliance with coding guidelines and regulations, and identifying areas for improvement and training. Internal and external coding audits help maintain the integrity of clinical coding and support accurate medical documentation, efficient billing, and reimbursement processes, and reliable healthcare statistics.
Roles and Responsibilities of Clinical Coders
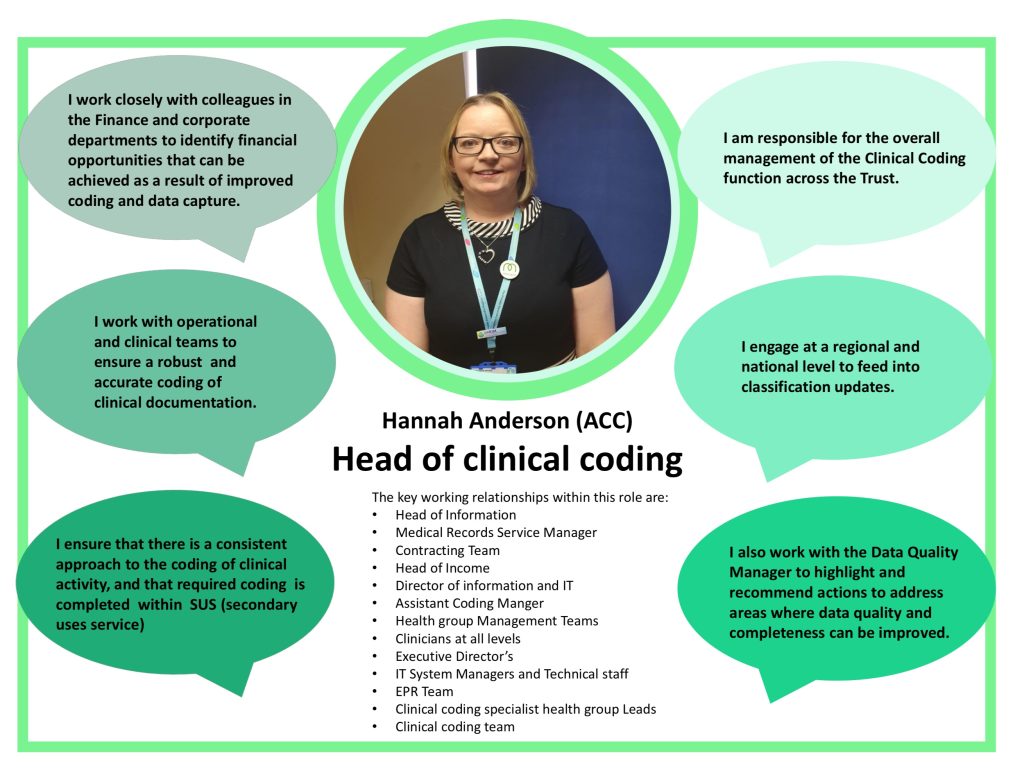
This image is property of fabnhsstuff.net.
Certification and Education Requirements
Clinical coders are highly skilled professionals who undergo specialized training and certification. They typically hold certifications such as Certified Coding Specialist (CCS) or Certified Professional Coder (CPC) that validate their competence in clinical coding. These certifications require a comprehensive understanding of coding systems, medical terminology, anatomy, physiology, and disease processes. Continuous education is crucial for clinical coders to stay updated with evolving coding guidelines, regulations, and technological advancements.
Coding Accuracy and Efficiency
Clinical coders are responsible for accurately translating medical information into codes. They must possess strong analytical skills and attention to detail to ensure coding accuracy and compliance with coding guidelines. Alongside accuracy, clinical coders must also maintain efficiency in their coding processes to meet the demands of healthcare settings. Timely and accurate coding plays a crucial role in revenue cycle management by facilitating timely billing and reimbursement and reducing the risk of claims rejection or denial.
Collaboration with Healthcare Providers
Clinical coders collaborate closely with healthcare providers, including physicians, nurses, and other allied health professionals. They work together to ensure accurate and complete documentation of patient encounters, clarify clinical details, and address any coding-related queries. Effective communication and collaboration enhance coding accuracy and enable healthcare providers to receive appropriate reimbursement for the services they provide.
Clinical Coding and Revenue Cycle Management

Support for Medical Billing
Clinical coding is a fundamental part of the revenue cycle management process in healthcare organizations. Accurate clinical coding enables the generation of claims for medical services provided to patients. These claims are then submitted to insurance companies or government reimbursement programs for payment. Without proper clinical coding, healthcare organizations would struggle to receive timely and appropriate payment for the care they deliver.
Documentation Improvement
Clinical coding plays a crucial role in documentation improvement initiatives within healthcare organizations. By ensuring accurate and detailed coding, clinical coders contribute to the completeness and specificity of medical records. This improves the accuracy of clinical documentation, supports effective communication among healthcare providers, and reduces the risk of coding-related errors. Enhanced documentation also facilitates better coordination of care, improves patient safety, and ensures the continuity of care across different healthcare settings.
Financial Impact on Healthcare Organizations
Accurate clinical coding has a direct financial impact on healthcare organizations. Coding errors or omissions can lead to claims rejection or denial, resulting in delayed or lost revenue for healthcare providers. Moreover, inaccurate coding can result in overpayment or underpayment for services rendered, affecting the financial viability of the organization. By ensuring coding accuracy and compliance, clinical coders contribute to the financial health and sustainability of healthcare organizations.
Importance of Coding Accuracy

Claims Rejection and Denials
Coding accuracy is crucial to prevent claims rejection or denial by insurance companies or government reimbursement programs. Inaccurate or incomplete coding can result in rejected or delayed claims, leading to delayed payments for healthcare services and potential financial difficulties for healthcare organizations. By ensuring coding accuracy and compliance with coding guidelines, clinical coders minimize the risk of claims rejection or denial, resulting in a smoother and more efficient revenue cycle.
Clinical Decision Making
Accurate coding has a direct impact on clinical decision-making. When evaluating patient records, healthcare providers rely on coded data to understand the patient’s medical history, diagnoses, and procedures performed. Inaccurate or incomplete coding can lead to wrong interpretations and incorrect clinical decisions, potentially compromising patient care and outcomes. By maintaining coding accuracy, clinical coders contribute to the reliability and quality of clinical decision-making, allowing for informed and evidence-based patient care.
Patient Safety and Quality of Care
Coding accuracy also plays a significant role in patient safety and the overall quality of care provided. Accurate coding ensures that healthcare providers have a complete and precise understanding of a patient’s conditions, treatments, and interventions. This information is crucial for effective care coordination, medication management, and the prevention of medical errors. By accurately coding medical information, clinical coders contribute to patient safety, improved outcomes, and the overall quality of healthcare delivery.
Challenges in Clinical Coding

Complexity of Coding Guidelines
Clinical coding is a highly complex task that requires a deep understanding of coding systems and guidelines. The coding guidelines, such as those provided by the American Hospital Association (AHA) and the Centers for Medicare and Medicaid Services (CMS), are extensive and regularly updated to reflect changes in medical practice and technology. Clinical coders must continuously keep up with these evolving guidelines to ensure accurate coding and comply with regulatory requirements, presenting a constant challenge in the field.
Evolving Healthcare Regulations
Healthcare regulations and reimbursement policies undergo frequent changes, adding another layer of complexity to clinical coding. Clinical coders must stay updated on the latest regulatory changes, such as those introduced by the CMS or private insurance companies, to ensure compliance and accurate coding. These regulatory changes often aim to improve transparency, standardization, and fraud prevention in healthcare, but they can pose challenges for clinical coders as they navigate the ever-changing landscape.
Technological Advancements
While technology brings numerous advancements to the healthcare industry, it also poses challenges in clinical coding. The implementation of electronic health records (EHRs) has transformed the way medical information is captured and stored. Clinical coders must adapt to new technologies and software systems, ensuring they are proficient in using EHRs and other coding tools. Additionally, the increasing use of artificial intelligence and machine learning in coding processes requires clinical coders to develop new skills and embrace the capabilities of technology to enhance coding accuracy and efficiency.
Emerging Trends in Clinical Coding
This image is property of static.wixstatic.com.
Implementation of Electronic Health Records (EHR)
The implementation of electronic health records (EHRs) has revolutionized the way healthcare organizations capture, store, and share patient information. EHRs provide clinical coders with immediate access to patient records, streamlining the coding process and enhancing accuracy. The integration of coding tools within EHR systems facilitates real-time coding, reduces administrative burden, and improves coding efficiency. The ongoing advancement in EHR technology presents exciting opportunities to further automate and optimize clinical coding processes.
Artificial Intelligence and Machine Learning
The field of clinical coding is experiencing transformative advancements with the integration of artificial intelligence (AI) and machine learning (ML) algorithms. AI-powered coding tools are being developed to automate code assignment and increase coding accuracy. ML algorithms analyze vast amounts of data, identify patterns, and suggest appropriate codes based on historical coding decisions. These technological advancements have the potential to revolutionize clinical coding, improving coding accuracy, efficiency, and productivity.
Remote and Virtual Coding
Another emerging trend in clinical coding is the adoption of remote and virtual coding. Remote coding allows clinical coders to work from home or off-site locations, offering flexibility and cost savings for healthcare organizations. Virtual coding involves the use of secure software and communication tools to assign codes remotely, facilitating collaboration and minimizing the need for physical infrastructure. Remote and virtual coding options are particularly valuable during times of crisis, such as the COVID-19 pandemic, when remote work has become more prevalent.
Future of Clinical Coding

Automation and Integration
The future of clinical coding lies in automation and integration. As technology continues to advance, clinical coding processes will become increasingly automated. AI-powered coding algorithms will assist clinical coders in assigning codes accurately and efficiently, reducing the risk of human error. Integration of coding tools within EHR systems will streamline coding processes, enabling real-time coding and seamless sharing of information between healthcare providers, coders, and billing departments.
Interoperability with Healthcare Systems
Interoperability is a critical aspect of the future of clinical coding. As healthcare systems become more integrated, the exchange of coded information will become seamless across different settings and platforms. Shared electronic health records and interoperable coding systems will improve care coordination, enhance data accuracy, and reduce administrative burden. The ability to exchange coded information across healthcare providers and organizations will contribute to a comprehensive and holistic understanding of patient health.
Continued Education and Professional Development
Continuous education and professional development will be essential for clinical coders in the future. As coding guidelines, regulations, and technology evolve, clinical coders must stay updated and enhance their skills and knowledge. Ongoing education and training programs will ensure that clinical coders remain proficient in coding systems, medical terminology, and emerging technologies. By investing in the professional development of clinical coders, healthcare organizations can ensure the accuracy and reliability of clinical coding processes.
In conclusion, clinical coding plays a vital role in the healthcare industry, ensuring accurate medical documentation, facilitating efficient billing and reimbursement, and supporting healthcare research and statistics. Clinical coders have the responsibility of assigning codes accurately, complying with coding guidelines, and collaborating with healthcare providers. Challenges in clinical coding, such as the complexity of coding guidelines, evolving healthcare regulations, and technological advancements, need to be addressed through continuous education and staying updated with emerging trends. The future of clinical coding lies in automation, interoperability, and the continued professional development of clinical coders.