Have you ever wondered what a medical coder does on a daily basis? If so, you’re in the right place. In this article, we will explore the important role of a medical coder and provide you with a comprehensive understanding of their daily tasks and responsibilities.
Stay tuned to learn more about the essential functions of a medical coder, including how they review and analyze medical records, assign appropriate codes to procedures and diagnoses, and ensure accurate billing and reimbursement for healthcare services. Additionally, we will delve into the knowledge and skills required for this profession, as well as the potential career opportunities that await those interested in pursuing a career in medical coding. Whether you’re considering a career in this field or simply curious about what medical coders do, this article will provide you with valuable insights. So let’s get started! Medical coders play a crucial role in the healthcare system, ensuring accurate and efficient coding that is essential for proper billing and quality patient care. Their daily responsibilities include reviewing medical records, assigning appropriate codes, ensuring accuracy, collaborating with healthcare professionals, utilizing coding software and tools, dealing with confidential patient information, ensuring compliance and accuracy, constant learning and professional growth, playing a critical role in revenue cycle management, and maintaining attention to detail.
Responsibilities of a Medical Coder

Reviewing medical records
One of the primary responsibilities of a medical coder is to review medical records. This involves carefully examining the documentation provided by healthcare professionals, including physician’s notes, lab results, imaging reports, and other relevant information. By reviewing these records, medical coders gain a comprehensive understanding of the patient’s condition and the services that were provided.
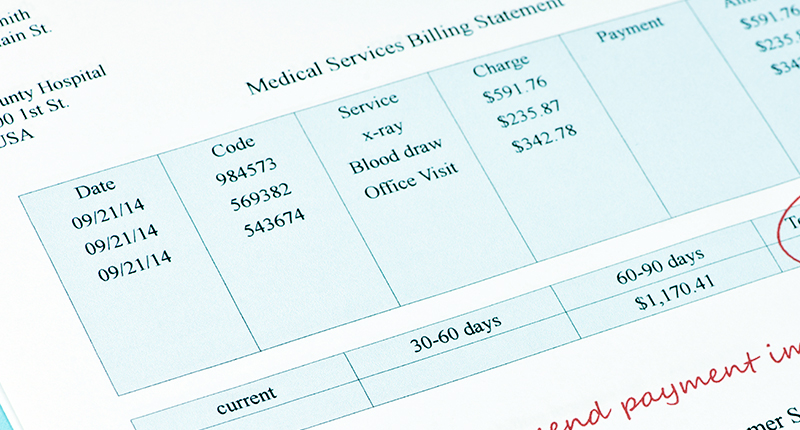
Assigning appropriate codes
After reviewing the medical records, medical coders assign appropriate codes to capture the specific diagnoses, procedures, and services performed during the patient’s treatment. They must have a thorough understanding of coding systems, such as the International Classification of Diseases, Tenth Revision (ICD-10) for diagnoses and Current Procedural Terminology (CPT) for procedures. Assigning the correct codes is crucial for accurate billing and reimbursement.
Ensuring accuracy of codes
Accuracy is of utmost importance in medical coding. Medical coders must ensure that the codes assigned reflect the services rendered and the diagnoses made accurately. They meticulously cross-reference the medical records, double-check the codes selected, and verify that they align with the appropriate guidelines and regulations. Any errors or discrepancies must be corrected promptly to maintain accuracy in the billing process.
Working with Healthcare Professionals

Collaborating with physicians
Medical coders work closely with physicians to ensure accurate coding. They may consult with physicians to clarify certain aspects of the medical record or to obtain additional information necessary for proper code assignment. By collaborating with physicians, medical coders contribute to the accuracy of the codes assigned and promote effective communication within the healthcare team.
Consulting with nurses and other staff
In addition to collaborating with physicians, medical coders also consult with nurses and other healthcare staff to gather supplementary information. This may include details on the medications administered, treatments performed, and any other relevant procedures. By consulting with the entire healthcare team, medical coders ensure that all aspects of the patient’s care are accurately captured in the coding process.
Coordinating with billing department
Medical coders work closely with the billing department to ensure that codes assigned align with the billing requirements. They coordinate with the billing team to ensure that the codes submitted for reimbursement accurately reflect the services provided. This collaboration ensures smooth revenue cycle management and reduces the chances of claim denials or rejections.
Knowledge and Skills Required
Understanding of medical terminology
To be effective in their role, medical coders must have a solid understanding of medical terminology. This knowledge allows them to accurately interpret and assign codes based on the specific diagnoses and treatments documented in the medical record. Medical coders must be able to decipher complex medical terms and abbreviations to ensure accurate coding.
Familiarity with coding systems (e.g. ICD-10, CPT)
Proficiency in coding systems, such as ICD-10 and CPT, is essential for medical coders. They must be familiar with the guidelines and conventions associated with these coding systems to assign accurate codes. Medical coders must stay updated with the latest coding changes, including new codes and revisions, to ensure compliance and accurate coding.
Analytical and problem-solving abilities
Medical coding requires strong analytical and problem-solving skills. Medical coders must be able to analyze complex medical records and identify the appropriate codes based on the information provided. They may encounter situations where the documentation is incomplete or ambiguous, and they must use their problem-solving abilities to determine the most accurate code assignment.
Utilizing Coding Software and Tools

Using electronic health record (EHR) systems
Medical coders utilize electronic health record (EHR) systems to access and review patient records. These systems provide a streamlined and efficient way to navigate through medical charts, annotate coding decisions, and facilitate collaboration with other healthcare professionals. Proficiency in EHR systems is crucial for medical coders to perform their job effectively.
Proficiency in coding software
Medical coders use specialized coding software to assist in the accurate assignment of codes. This software often includes coding aides and tools that help validate the codes selected and ensure compliance with coding guidelines. Medical coders must be proficient in using such software to enhance their productivity and accuracy.
Staying updated with industry changes
The healthcare industry is constantly evolving, and medical coders must stay updated with the latest changes in coding guidelines, regulations, and industry best practices. They must actively engage in continuous learning and professional development by attending seminars, workshops, and conferences. Staying updated enables medical coders to maintain their competency and adapt to industry changes effectively.
Dealing with Confidential Patient Information
Maintaining patient privacy and confidentiality
As healthcare professionals, medical coders have a legal and ethical obligation to maintain patient privacy and confidentiality. They handle sensitive and confidential information on a daily basis, and it is their responsibility to ensure that this information is protected. Medical coders must adhere to strict confidentiality protocols and maintain the utmost professionalism when handling patient data.
Adhering to HIPAA regulations
Medical coders must comply with the Health Insurance Portability and Accountability Act (HIPAA) regulations. HIPAA governs the privacy and security of patient information and sets standards for its protection. Medical coders must be well-versed in HIPAA regulations and ensure that they handle patient information in accordance with the law.
Secure storage and transmission of data
Medical coders must ensure that patient information is securely stored and transmitted. They must follow secure data transmission protocols and use encrypted communication channels to transfer patient data. By implementing appropriate security measures, medical coders contribute to the protection of patient privacy and safeguard healthcare information.
Ensuring Compliance and Accuracy

Reviewing codes for compliance
Medical coders play a critical role in ensuring compliance with coding guidelines and regulations. They review the codes assigned and verify that they align with the applicable guidelines, including those established by the Centers for Medicare and Medicaid Services (CMS) and other regulatory bodies. Compliance with these guidelines is essential for accurate billing and reimbursement.
Auditing medical documentation
Medical coders may conduct audits of medical documentation to ensure its accuracy and completeness. These audits help identify any patterns of errors or discrepancies and provide feedback to healthcare professionals for improvement. By conducting regular audits, medical coders contribute to the overall accuracy and quality of the medical coding process.
Correcting errors and discrepancies
If any errors or discrepancies are identified in the coding process, medical coders take appropriate actions to correct them. They may communicate with the healthcare professionals involved to obtain additional information or clarification and make the necessary adjustments to the codes assigned. Correcting errors and discrepancies ensures the accuracy of the billing process and prevents potential issues with reimbursement.
Constant Learning and Professional Growth

Continuing education and training
Medical coding is a dynamic field that requires ongoing learning and professional development. Medical coders must engage in continuous education and training to stay updated with the latest coding guidelines, regulations, and industry trends. This may involve taking courses, attending webinars, or pursuing certifications to enhance their knowledge and skills.
Attending seminars and workshops
Seminars and workshops provide valuable opportunities for medical coders to gain in-depth knowledge and practical insights from experts in the field. These events cover a wide range of topics, such as coding updates, regulatory changes, and best practices. By attending seminars and workshops, medical coders can expand their professional network and stay current with industry advancements.
Staying updated with coding guidelines
Medical coders must stay updated with coding guidelines to ensure accurate code assignment. They must familiarize themselves with the latest updates and revisions to avoid coding errors and potential compliance issues. By staying informed, medical coders can contribute to the quality and accuracy of the coding process.
Critical Role in Revenue Cycle Management
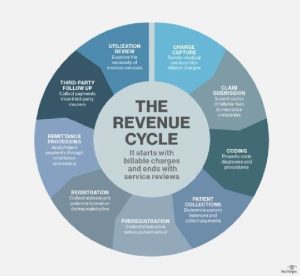
Contributing to accurate billing and claims
Medical coders play a critical role in revenue cycle management by ensuring accurate billing and claims processing. They assign the appropriate codes that capture the services rendered and diagnoses made during the patient’s treatment. Accurate coding is vital for generating claims that reflect the true scope of services provided, leading to appropriate reimbursement for healthcare providers.
Maximizing reimbursement potential
By accurately coding the medical services provided, medical coders contribute to maximizing reimbursement potential. They ensure the inclusion of all billable services and procedures, allowing healthcare providers to receive fair and appropriate reimbursement for their services. Maximizing reimbursement potential helps healthcare organizations maintain their financial stability and provide quality patient care.
Reducing denials and rejections
Medical coders play a crucial role in reducing claim denials and rejections. By accurately assigning codes, medical coders minimize the risk of coding errors and discrepancies that can lead to claim denials or delays in reimbursement. Their expertise in coding guidelines and regulations helps ensure the submission of clean claims, thereby reducing the administrative burden on healthcare organizations.
Importance of Attention to Detail

Thoroughly reviewing medical charts
Attention to detail is essential for medical coders to accurately interpret and assign codes. They must carefully review medical charts, paying close attention to the documentation provided by healthcare professionals. By thoroughly reviewing medical charts, medical coders can capture all relevant information and assign the appropriate codes with precision.
Applying appropriate codes with precision
Medical coders must apply the appropriate codes with precision. They must ensure that the codes assigned accurately reflect the specific diagnoses, procedures, and services performed during the patient’s treatment. By applying the codes with precision, medical coders contribute to accurate billing and reimbursement, as well as the continuity of care for the patient.
Avoiding coding errors
Coding errors can have significant consequences, ranging from claim denials to potential legal and compliance issues. Therefore, medical coders must avoid coding errors by paying meticulous attention to detail. By exercising precision in code assignment and adhering to coding guidelines, medical coders help minimize coding errors and promote accuracy in the billing process.
Conclusion
In conclusion, medical coders play a vital role in the healthcare system by ensuring accurate and efficient coding that is essential for proper billing and quality patient care. Their daily responsibilities include reviewing medical records, assigning appropriate codes, ensuring accuracy, collaborating with healthcare professionals, utilizing coding software and tools, dealing with confidential patient information, ensuring compliance and accuracy, constant learning and professional growth, playing a critical role in revenue cycle management, and maintaining attention to detail. Medical coders’ expertise ensures efficient billing, maximizes reimbursement potential, reduces denials and rejections, and contributes to overall quality patient care. With their dedication and attention to detail, medical coders make a significant impact on the healthcare industry.