To pursue a career as a clinical coder, you must possess a unique set of skills and qualifications. In this article, we will explore the essential requirements necessary to thrive in this profession. From a comprehensive understanding of medical terminology and coding systems to in-depth knowledge of anatomy and disease processes, being a clinical coder demands a meticulous eye for detail and a strong analytical mindset. Additionally, effective communication skills and the ability to work independently are crucial for success in this field. Join us as we delve into the key qualifications and qualities that make up a proficient clinical coder, and discover the rewarding opportunities that await those willing to embark on this path.
Education and Training

High School Diploma or Equivalent
To start a career as a clinical coder, a high school diploma or equivalent is typically the minimum educational requirement. This provides a strong foundation in basic skills such as reading, writing, and mathematics, which are essential for success in this field.
Associate’s Degree in Health Information Technology
While a high school diploma is the minimum requirement, earning an associate’s degree in health information technology can greatly enhance your chances of securing a clinical coding position. This degree program provides specialized education in medical coding, health information management, and other relevant subjects.
Certification in Medical Coding
In addition to formal education, obtaining certification in medical coding is highly recommended. There are several professional certifications available, such as the Certified Professional Coder (CPC) exam, Certified Coding Specialist (CCS) exam, Certified Coding Associate (CCA) exam, and Certified Professional Coder-Payer (CPC-P) exam. These certifications validate your knowledge and skills in coding and demonstrate your commitment to professionalism in the field.
Continuing Education
To stay current with the evolving field of clinical coding, it is essential to participate in continuing education. This can include attending conferences, workshops, or seminars, as well as pursuing additional certifications or advanced degrees. Continuing education ensures that you stay up to date with industry changes and advances in medical coding practices.
Knowledge and Skills

Medical Terminology
One of the fundamental skills required for a clinical coder is a strong understanding of medical terminology. This includes knowledge of anatomical terms, medical abbreviations, and common medical conditions. Being proficient in medical terminology enables accurate coding and allows for effective communication with medical professionals.
Anatomy and Physiology
An understanding of human anatomy and physiology is crucial in clinical coding. This knowledge helps coders correctly assign codes based on the location and nature of the medical condition or procedure. Familiarity with the various body systems and their functions allows for accurate coding and ensures proper documentation.
ICD Coding Systems
The International Classification of Diseases (ICD) coding system is used by clinical coders to assign codes to diagnoses and procedures. A comprehensive understanding of the ICD coding system is essential for accurate and consistent coding. This system is regularly updated, requiring coders to stay informed about the latest revisions and guidelines.
CPT Coding System
The Current Procedural Terminology (CPT) coding system is used to assign codes to medical procedures and services. Clinical coders must have a thorough understanding of the CPT coding system to accurately identify and code procedures performed on patients. This system is also subject to regular updates, making ongoing education necessary to maintain proficiency.
HIPAA Regulations
Clinical coders handle sensitive patient information on a daily basis, making an understanding of the Health Insurance Portability and Accountability Act (HIPAA) regulations crucial. Compliance with HIPAA regulations ensures patient privacy and confidentiality, protecting their personal health information from unauthorized access or disclosure.
Computer Skills
Clinical coders rely heavily on computer systems and software to perform their duties. Proficiency in computer skills, including data entry, electronic health record systems, and coding software, is essential. Strong computer skills allow for efficient and accurate coding, as well as effective communication with other healthcare professionals.
Analytical Skills
Clinical coders must possess strong analytical skills to interpret medical documentation, identify relevant information, and assign appropriate codes. Analytical skills enable coders to analyze complex medical records and make accurate coding decisions based on the available information.
Attention to Detail
Attention to detail is critical in clinical coding, as even a small error can have significant consequences. Coders must carefully review medical records, ensuring that all relevant details are considered and accurately coded. Meticulous attention to detail is necessary to maintain coding accuracy and ensure proper reimbursement for healthcare services.
Excellent Communication
Effective communication is essential for clinical coders, as they frequently collaborate with other healthcare professionals. Coders need to communicate coding information clearly and accurately to physicians, nurses, and other medical staff to Ensure proper documentation and coding practices. Additionally, coders must possess good written communication skills to complete coding reports and interact with insurance companies and auditors.
Ethics and Confidentiality
Clinical coders handle sensitive patient information and must adhere to strict ethical guidelines. Maintaining confidentiality and integrity in handling patient data is critical. Coders must prioritize patient privacy and handle information ethically, ensuring that only authorized individuals have access to patient records.
Experience

Entry-Level Positions
Entry-level positions are an excellent starting point for individuals interested in becoming clinical coders. These positions often provide on-the-job training, allowing individuals to gain practical experience in coding and familiarize themselves with various coding practices and healthcare settings.
Internships
Internships provide valuable hands-on experience in clinical coding. These opportunities allow individuals to apply their knowledge and skills in real-world scenarios, under the supervision of experienced professionals. Internships also provide networking opportunities and can lead to job offers or recommendations upon completion.
On-The-Job Training
Some healthcare facilities offer on-the-job training programs for aspiring clinical coders. These programs typically involve working closely with experienced coders and gradually increasing responsibilities as skills are developed. On-the-job training allows for practical, tailored learning experiences and the opportunity to gain coding proficiency in a specific healthcare setting.
Important Attributes

Attention to Detail
Attention to detail is critical in clinical coding to ensure accurate and precise coding. Coders must carefully review medical records, paying close attention to details such as physician notes, lab results, and medications. A meticulous approach is necessary to accurately assign codes and ensure proper documentation.
Accuracy
Accuracy is paramount in clinical coding. Coders must assign the correct codes for diagnoses and procedures, as errors can lead to incorrect billing, denied insurance claims, or compromised patient care. Maintaining a high level of accuracy is essential for effective healthcare management and patient safety.
Organizational Skills
Clinical coders must possess strong organizational skills to manage large volumes of medical records and coding documentation. Organizational skills help coders stay focused, prioritize tasks, and maintain efficient workflows. Proper organization ensures that nothing is missed, reducing the risk of coding errors.
Time Management
Effective time management is crucial for clinical coders, who often face tight deadlines and heavy workloads. Coders must be able to manage their time efficiently to ensure timely and accurate coding. Being able to prioritize tasks, minimize distractions, and work efficiently under pressure is essential for success in this fast-paced profession.
Problem-Solving
Clinical coders encounter diverse medical cases and complex documentation, requiring strong problem-solving skills. Coders must analyze medical records, interpret information, and determine the most appropriate codes for diagnoses and procedures. Effective problem-solving skills enable coders to navigate challenging situations and ensure accurate coding practices.
Ethical Conduct
Ethical conduct is essential in the field of clinical coding. Coders must adhere to professional and ethical standards, protecting patient confidentiality and privacy. Upholding ethical conduct ensures that patient information remains secure and that coding practices are conducted with integrity and professionalism.
Confidentiality
Maintaining patient confidentiality is a top priority for clinical coders. Coders handle sensitive medical information and must ensure its privacy and security. Respecting patient confidentiality builds trust and ensures compliance with legal and ethical guidelines.
Medical Coding Certification
This image is property of www.rasmussen.edu.
Certified Professional Coder (CPC) Exam
The Certified Professional Coder (CPC) exam is widely recognized in the field of clinical coding. This certification demonstrates proficiency in accurately assigning codes to diagnoses, procedures, and medical services. The CPC exam covers various healthcare settings, guidelines, and coding systems.
Certified Coding Specialist (CCS) Exam
The Certified Coding Specialist (CCS) exam is another recognized certification for clinical coders. This certification demonstrates expertise in reviewing medical records and assigning codes in hospital settings. The CCS exam covers inpatient and outpatient coding, as well as knowledge of coding systems specific to hospital procedures and diagnoses.
Certified Coding Associate (CCA) Exam
The Certified Coding Associate (CCA) exam is an entry-level certification for clinical coders. This certification validates foundational knowledge and skills in medical coding. The CCA exam covers basic coding principles, anatomy, and medical terminology.
Certified Professional Coder-Payer (CPC-P) Exam
The Certified Professional Coder-Payer (CPC-P) exam is an advanced certification specifically designed for coders working for insurance companies or payer organizations. This certification demonstrates expertise in processing claims, reviewing medical records, and ensuring accurate payment and reimbursement.
Work Environment

Healthcare Facilities
Clinical coders are employed in various healthcare facilities, including hospitals, clinics, and physician offices. These work environments provide opportunities for coders to collaborate with healthcare professionals, access medical records, and ensure accurate coding for patient care and billing purposes.
Hospitals
Many clinical coders find employment in hospitals, where they handle a wide range of medical records and coding assignments. Hospital coders often specialize in specific areas, such as emergency medicine, surgery, or oncology. Hospital settings offer diverse coding opportunities and exposure to complex medical cases.
Clinics
Clinics, particularly larger multi-specialty clinics, also employ clinical coders. These coders play a crucial role in coding outpatient procedures and diagnostic tests. Clinic settings offer coders the opportunity to work with various medical specialties and gain expertise in specific areas of healthcare.
Physician Offices
Clinical coders working in physician offices primarily focus on coding and billing for a specific medical practice or group. They work closely with physicians to ensure accurate coding and proper documentation, supporting efficient reimbursement and revenue cycles.
Government Agencies
Government agencies, such as the Centers for Medicare and Medicaid Services (CMS), also employ clinical coders. Coders working for government agencies play a vital role in ensuring compliance with coding regulations and guidelines. These positions often involve conducting audits and providing coding education and support to healthcare providers.
Insurance Companies
Insurance companies rely on clinical coders to review medical records and process insurance claims. Coders employed by insurance companies ensure that claims are accurately coded and compliant with coding guidelines, allowing for appropriate reimbursement to healthcare providers.
Remote Positions
With the advancement of technology, many clinical coders have the option to work remotely. Remote positions enable coders to work from home or other locations, using secure online connections to access medical records and coding software. Remote work offers flexibility and the ability to balance work and personal responsibilities.
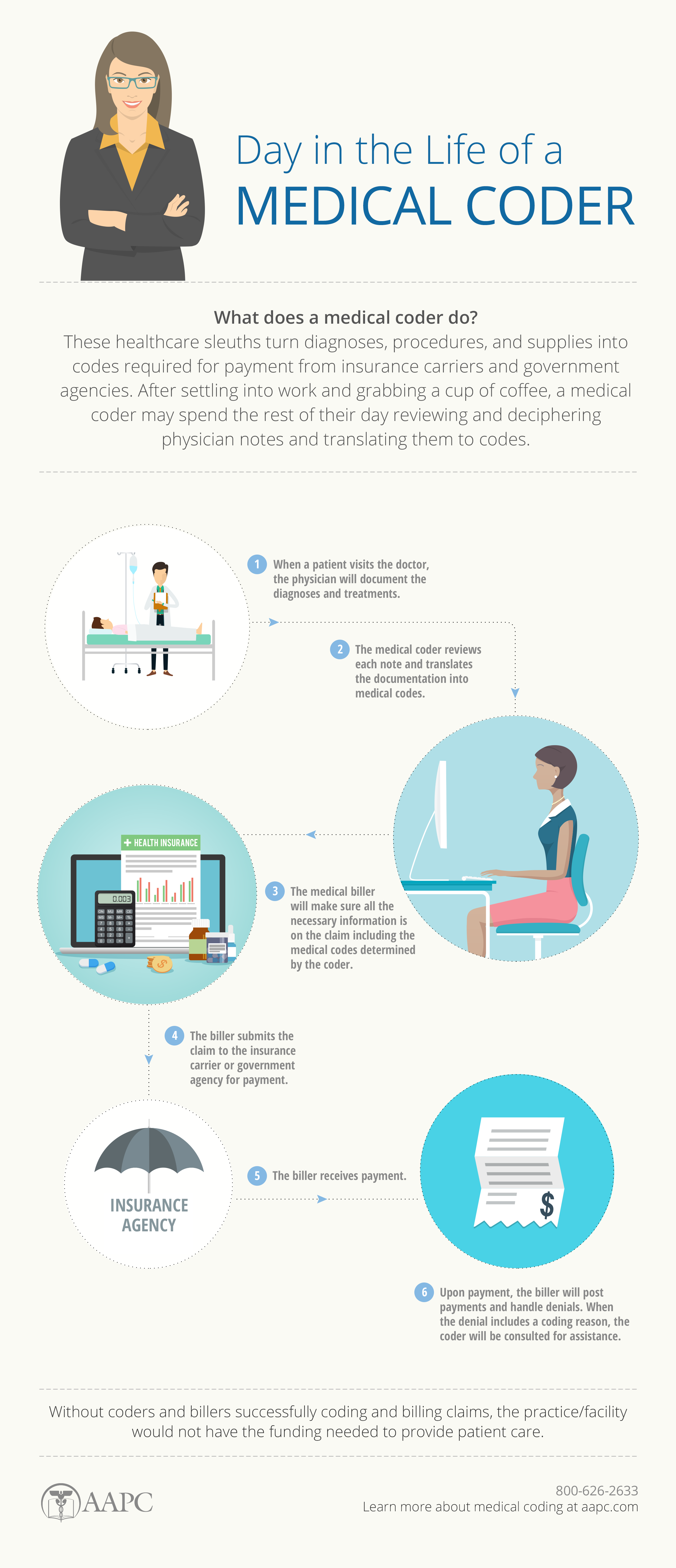
Job Responsibilities

Reviewing Medical Records
Clinical coders are responsible for reviewing medical records, including physician notes, lab results, and diagnostic reports. They analyze the documentation to identify relevant diagnoses, procedures, and services for coding purposes. Thoroughly reviewing medical records ensures accurate coding and proper documentation.
Assigning Codes for Diagnoses and Procedures
One of the main responsibilities of clinical coders is to assign appropriate codes for diagnoses and procedures. They use coding systems such as ICD and CPT to accurately represent the medical services provided. Properly assigned codes are essential for billing, reimbursement, and data analysis.
Ensuring Code Accuracy
Clinical coders must ensure the accuracy of assigned codes to avoid errors or discrepancies in the coding process. They need to stay up to date with coding guidelines and regulations to ensure compliance. Regular auditing and quality checks help maintain high coding accuracy standards.
Keeping up with Industry Changes
The field of clinical coding is dynamic, with coding guidelines and regulations frequently updated. Coders must stay informed about industry changes, attend workshops or seminars, and participate in continuing education to keep their knowledge and skills up to date. Keeping up with industry changes ensures accurate and compliant coding.
Collaborating with Healthcare Professionals
Clinical coders often collaborate with other healthcare professionals, including physicians, nurses, and administrative staff. Effective communication and collaboration are essential for accurate coding, as coders may need clarification on diagnoses or procedures. Collaboration ensures proper documentation and accurate coding for optimal patient care and reimbursement.
Maintaining Confidentiality
Clinical coders handle sensitive patient information and must maintain patient confidentiality at all times. They strictly adhere to privacy regulations, ensuring that patient records and information are kept secure. Confidentiality is crucial in maintaining patient trust and safeguarding protected health information.
Meeting Productivity and Quality Standards
Clinical coders are often expected to meet productivity and quality standards set by their employers or industry guidelines. They need to balance efficiency with accuracy to ensure timely and accurate coding. Meeting productivity and quality standards supports efficient healthcare management and maximizes revenue cycle performance.
Following Legal and Ethical Guidelines
Clinical coders must follow legal and ethical guidelines when performing their duties. They should code accurately, ensuring compliance with coding regulations and guidelines. Upholding legal and ethical standards safeguards patient privacy and ensures appropriate billing practices.
Career Advancement

Specialization in Specific Healthcare Fields
Clinical coders often have the opportunity to specialize in specific healthcare fields. Specialization allows coders to develop expertise in a particular area, such as cardiology, orthopedics, or pediatrics. Specialized coders are in high demand and can advance their careers by focusing on specific healthcare disciplines.
Management Roles
Experienced clinical coders may advance to managerial or supervisory roles within healthcare organizations. These positions involve overseeing coding departments, managing coding teams, and ensuring coding compliance and accuracy across the organization. Management roles require strong leadership skills and a comprehensive understanding of coding practices.
Teaching or Training Positions
Clinical coders with significant experience and expertise may choose to pursue teaching or training roles. They can become instructors in educational institutions or provide training and education to other coders, healthcare professionals, or organizations. Teaching or training positions contribute to the professional growth of coders and allow them to share their knowledge and expertise.
Consulting
Experienced clinical coders may choose to work as consultants, providing coding expertise to healthcare organizations. Coders in consulting roles assist with coding audits, compliance assessments, and coding education. Consulting offers a diverse range of opportunities and allows coders to contribute their expertise to various healthcare settings.
Salary and Job Outlook

Median Annual Salary
The median annual salary for clinical coders varies depending on factors such as education, certification, experience, and geographical location. According to the U.S. Bureau of Labor Statistics, the median annual wage for medical records and health information technicians, which includes clinical coders, was $44,090 as of May 2020.
Job Growth
The job outlook for clinical coders is promising, with a projected growth rate of 8% from 2019 to 2029, according to the U.S. Bureau of Labor Statistics. This growth is driven by an increased demand for healthcare services and the need for accurate coding and documentation for insurance purposes. Clinical coders with certifications and specialized skills are expected to have favorable job prospects.
Conclusion
Demand for clinical coders continues to grow as healthcare organizations strive for accurate coding and proper reimbursement. While a high school diploma is the minimum educational requirement, obtaining an associate’s degree in health information technology and obtaining professional certifications greatly enhance career prospects. In addition to formal education, developing strong knowledge and skills in medical terminology, anatomy and physiology, coding systems, and computer skills is crucial. Clinical coders should also possess important attributes such as attention to detail, accuracy, organizational skills, time management, problem-solving ability, ethical conduct, and confidentiality. With experience and further education, clinical coders have opportunities for advancement, including specialization, management roles, teaching or training positions, and consulting. The salary for clinical coders varies based on factors such as education, experience, and location, with a median annual wage of $44,090. The job outlook for clinical coders is promising, with a projected growth rate of 8% from 2019 to 2029. Overall, the field of clinical coding offers a rewarding career path with opportunities for growth and professional development.