We are here to shed light on a pressing issue that plagues health offices everywhere – billing complications. In today’s article, we will identify and dissect the three primary problems that often arise in the realm of medical billing. By addressing these challenges head-on, we aim to equip health professionals with the knowledge and tools they need to streamline their billing processes and ensure financial stability for their practices.
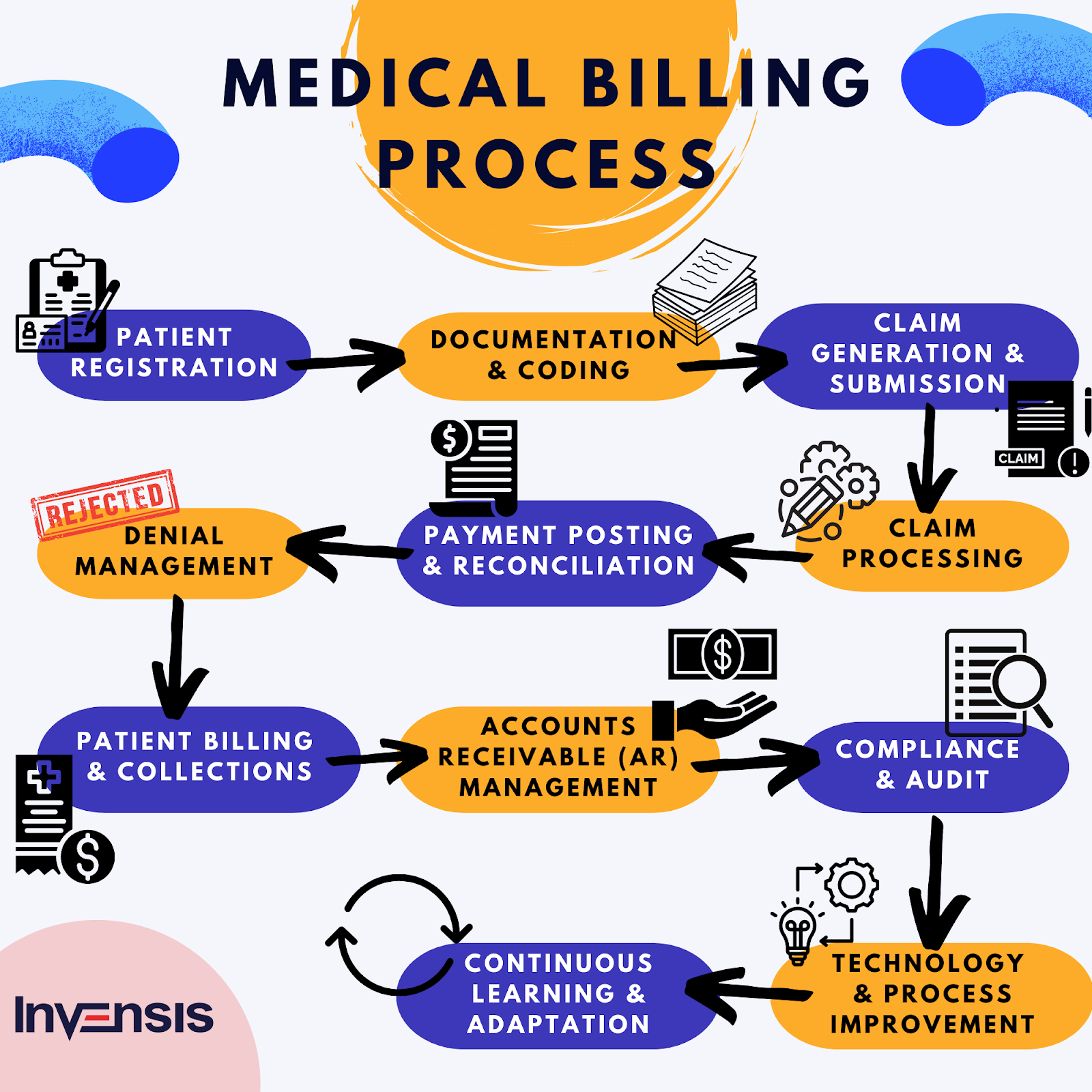
In the complex landscape of healthcare administration, billing is a critical aspect that demands precision and attention to detail. Unfortunately, it is all too common for health offices to encounter hurdles in this arena, resulting in delayed payments, dissatisfied patients, and financial strain. Through extensive research and analysis, we have identified the three primary issues that contribute to these problems. By the end of this article, you will not only have a comprehensive understanding of these challenges but also practical steps to overcome them, enabling you to provide better care for your patients while maintaining the financial health of your practice. So, let’s dive in and explore the intricacies of billing in a health office.
Incorrect coding
Lack of properly trained coding staff
One of the main problems with billing in a health office is the lack of properly trained coding staff. Coding is a critical aspect of the billing process as it involves translating medical procedures, diagnoses, and services into corresponding codes for billing purposes. Without a well-trained coding team, there is a significant risk of inaccuracies and coding errors, which can lead to claim denials, delays in payment, and even legal issues. It is essential for health offices to invest in the training and development of their coding staff to ensure accuracy and compliance with coding guidelines.
Failure to regularly update coding practices
Another problem that arises in many health offices is the failure to regularly update coding practices. The healthcare industry is constantly evolving, with new procedures, services, and diagnoses being introduced regularly. It is crucial for health offices to keep up with these changes and ensure that their coding practices are up to date. Failure to do so can result in outdated codes being used, leading to claim denials or underpayment. Regularly reviewing and updating coding practices is essential to stay compliant with industry standards and maximize revenue for the health office.
Errors in assigning medical codes
Assigning medical codes is a complex task that requires careful attention to detail. However, errors in assigning codes are a common problem in many health offices. These errors can result from misinterpretation of medical records, lack of familiarity with coding guidelines, or simple oversight. Incorrect coding can lead to claim denials, delays in payment, and even legal consequences. Health offices should implement quality control measures, such as double-checking codes and conducting regular audits, to minimize coding errors and ensure accurate billing.
Inaccurate patient information
Incomplete or outdated patient records
Inaccurate patient information is another significant problem that affects billing in health offices. Incomplete or outdated patient records can lead to errors in billing and claims processing. For example, if a patient’s insurance information is not up to date or if their medical history is incomplete, it can result in claim denials or delays in payment. Health offices need to establish efficient systems for collecting and maintaining accurate patient records. Regularly verifying and updating patient information is crucial to ensure smooth billing processes and minimize the risk of errors.
Failure to verify insurance coverage
Verifying insurance coverage is an essential step in the billing process. However, many health offices neglect this crucial task, leading to problems with billing. Failure to verify insurance coverage can result in claims being submitted to the wrong insurance provider, claims being denied due to lack of coverage, or inaccurate billing. Health offices should implement robust insurance verification processes to ensure that the patient’s coverage is confirmed before proceeding with billing. Verifying insurance coverage upfront can prevent claim rejections, reduce payment delays, and improve overall revenue cycle management.
Failure to collect accurate demographic data
Collecting accurate demographic data is vital for proper billing and claims processing. However, health offices often face challenges in this area. Failure to collect accurate demographic data, such as the patient’s address, contact information, or insurance details, can lead to claim denials or incorrect billing. Health offices should implement efficient and standardized data collection processes, such as using electronic forms or online registration portals, to gather accurate demographic information from patients. Regularly reviewing and updating demographic data is crucial to ensure accurate billing and minimize administrative errors.
Improper billing procedures
Lack of standardized billing processes
A lack of standardized billing processes is a common problem in many health offices. Without standardized procedures in place, each staff member may follow their own approach to billing, leading to inconsistencies, errors, and inefficiencies. Standardizing billing processes is crucial for ensuring accuracy, reducing the risk of errors, and enhancing overall efficiency. Health offices should implement clear billing guidelines, provide comprehensive training to staff members, and regularly review and update their billing procedures to maintain consistency and compliance.
Inefficient use of technology
Technology plays a vital role in modern healthcare billing, but inefficiency in its use can create problems in health offices. Inefficient use of billing software or other technology tools can result in errors, delays, and increased administrative burden. Health offices should invest in robust billing software and ensure that staff members receive proper training on its effective use. Regularly evaluating and optimizing the use of technology tools can help streamline billing processes, reduce errors, and improve overall efficiency in the health office.
Failure to adhere to billing regulations
Adhering to billing regulations is critical to avoid legal issues, financial penalties, and reputational damage. However, many health offices face challenges in staying compliant with the complex and ever-changing billing regulations. Failure to comply with billing regulations can result in claim denials, audits, or even fraud investigations. It is essential for health offices to stay updated on relevant regulations, invest in staff training on compliance, and establish internal auditing and monitoring processes. By adhering to billing regulations, health offices can mitigate risk, maintain financial integrity, and build trust with patients and insurance providers.
In conclusion, billing in a health office faces several main problems, including incorrect coding, inaccurate patient information, and improper billing procedures. Addressing these issues requires investment in training and developing coding staff, regularly updating coding practices, ensuring accurate patient information, verifying insurance coverage, collecting accurate demographic data, standardizing billing processes, optimizing technology use, and adhering to billing regulations. By addressing these challenges, health offices can improve billing accuracy, accelerate payment processing, and enhance overall revenue cycle management.