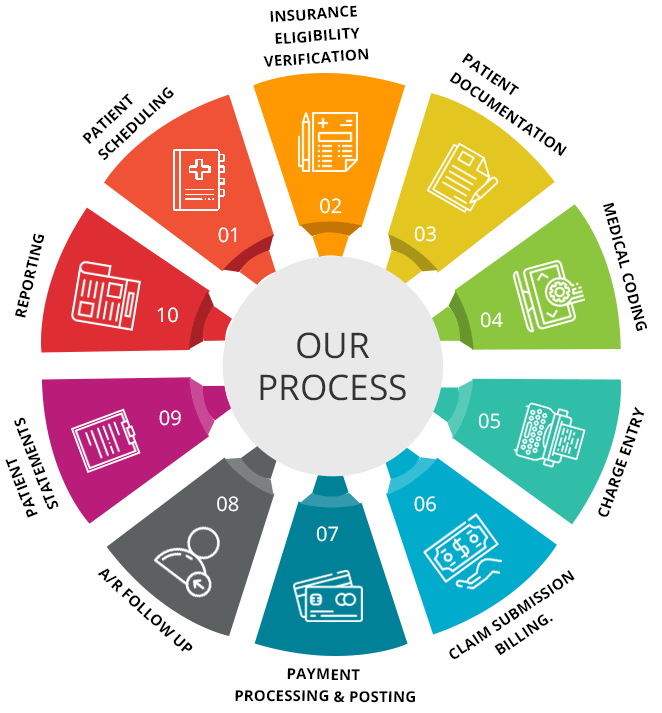
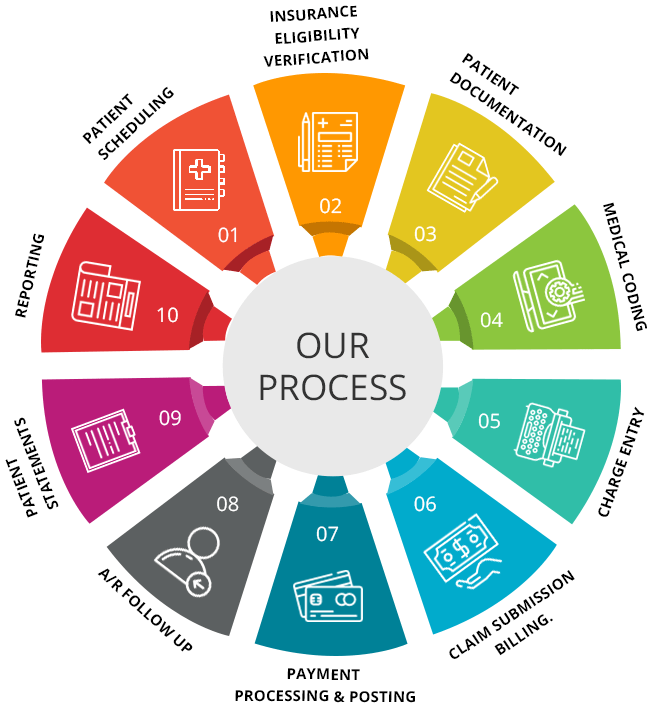
In this article, you will learn about the various steps involved in the medical billing process. This information will help you understand the complex and critical process of billing for medical services and ensure accurate and timely payment.
The first step in the medical billing process is to gather all necessary patient information and verify insurance coverage. This involves obtaining personal and insurance details from the patient, such as their name, address, date of birth, and insurance policy number. Once this information is collected, it is crucial to verify the patient’s insurance coverage to ensure the services provided are eligible for reimbursement.
The next step is to accurately code the medical services provided. This requires assigning specific codes to each procedure, diagnosis, and service rendered. These codes are standardized and used to communicate with insurance companies, ensuring that they understand the nature and extent of the healthcare services provided. Accurate coding is essential for the claims to be processed correctly and for accurate reimbursement.
Following coding, the third step is to submit the claim to the insurance company. This can be done electronically or via paper submission, depending on the insurer’s requirements. It is essential to ensure that all necessary documentation and supporting documents are included with the claim to avoid any delays or denials. The claim is reviewed by the insurance company, and a determination is made regarding its eligibility for reimbursement.
Finally, the last step in the medical billing process is to receive payment and initiate any necessary follow-up. Once the claim is approved, the insurance company will issue payment to the healthcare provider. It is crucial to keep track of all payments received and reconcile them with the claims submitted. If there are any discrepancies or unpaid claims, follow-up with the insurance company is necessary to rectify any issues and ensure timely payment.
Registration

Collecting patient information
The first step in the medical billing process begins with registration. When a patient arrives at a healthcare facility, they are asked to provide their personal and insurance information. This includes their full name, date of birth, address, contact details, and insurance policy number. Collecting accurate patient information is crucial for ensuring efficient billing and reimbursement.
Verifying insurance coverage
Once the patient’s information is collected, it is important to verify their insurance coverage. This involves contacting the insurance company to confirm the patient’s eligibility and coverage details. This step ensures that the services provided to the patient will be covered by their insurance plan. Verifying insurance coverage helps prevent unnecessary denials and delays in reimbursement.
Updating patient records
After verifying insurance coverage, the next step is to update the patient’s records. This includes entering all the relevant information into the healthcare facility’s electronic or paper-based system. It is important to ensure that the patient’s records are accurate and up to date, as this information will be used throughout the billing process. Updating patient records helps facilitate smooth communication with insurance companies and supports accurate billing and coding.
Documentation

Recording patient diagnoses and procedures
Once the patient’s information is updated, healthcare professionals need to document the diagnoses and procedures performed during the patient’s visit. This documentation is essential for accurate coding and billing. Properly recording the diagnoses and procedures ensures that the medical claims submitted reflect the services provided to the patient.
Submitting medical reports and test results
In addition to documenting diagnoses and procedures, medical reports and test results need to be submitted as supporting documentation for the claims. This ensures that the insurance company has all the necessary information to review and process the claim. Submitting medical reports and test results helps provide a comprehensive view of the patient’s condition and assists in justifying the services billed.
Coding

Assigning appropriate medical codes
Coding is a critical step in the medical billing process. It involves assigning specific codes to patient diagnoses, procedures, and services. These codes are used to identify and classify medical services and conditions for billing purposes. Proper coding ensures accurate reimbursement and compliance with coding guidelines.
Ensuring accuracy and compliance with coding guidelines
While assigning medical codes, it is important to ensure accuracy and compliance with coding guidelines. Inaccurate coding can lead to claim denials or delays in reimbursement. Healthcare providers should stay updated with the latest coding conventions and guidelines to ensure proper coding practices. Accuracy and compliance with coding guidelines are crucial for smooth claim processing and reimbursement.
Claim Submission

Preparing and reviewing claims
Once the coding is completed, claims need to be prepared and reviewed before submission to the insurance companies. This involves compiling all the necessary information, including patient demographics, diagnoses, procedures, and supporting documentation. Claims should be thoroughly reviewed to check for accuracy and completeness before submission.
Submitting claims to insurance companies
After preparing and reviewing the claims, they can be submitted to the respective insurance companies. Insurance companies have specific procedures and platforms for claim submission, which can be electronic or paper-based. It is important to follow the insurance company’s guidelines and requirements to ensure successful claim submission. This step initiates the process of reimbursement from the insurance company.
Claims Processing

Adjudicating claims
Once the claims are submitted, insurance companies review and process them. This involves verifying the information provided, checking for policy coverage, and evaluating the claims based on coding and billing guidelines. Claims are adjudicated to determine if they meet the criteria for reimbursement. Adjudication can result in approval, denial, or request for additional information or clarification.
Reviewing for errors or missing information
During the claims processing stage, insurance companies review the claims for errors or missing information. If there are any discrepancies or missing details, the insurance company may request additional documentation or clarification from the healthcare provider. It is important to address these issues promptly to prevent claim denials or delays in reimbursement.
Determining payment amount
After reviewing the claims, insurance companies determine the payment amount based on the policy coverage, negotiated rates, and reimbursement rules. The payment amount may be the full billed amount, a partial payment, or in some cases, no payment at all. It is important to review the payment amount carefully and reconcile it with the original claim to ensure accurate reimbursement.
Invoice Generation

Creating and sending invoices to patients
Once the insurance company has processed the claims and provided reimbursement, healthcare providers need to generate and send invoices to patients for any remaining balance. This typically includes deductibles, co-pays, and non-covered services. Invoices should clearly outline the services provided, the payment amount, and any insurance adjustments. Creating and sending invoices promptly helps ensure timely payment from patients.
Providing itemized billing information
In addition to the invoice, healthcare providers should also provide itemized billing information to patients upon request. This includes a breakdown of the charges for each service or procedure performed. Itemized billing helps patients understand the charges and encourages transparency in the billing process. Providing itemized billing information demonstrates a commitment to clear communication and enhances patient satisfaction.
Payment Collection

Following up on unpaid invoices
After sending the invoices, healthcare providers need to follow up on unpaid invoices. This may involve sending reminders or making phone calls to remind patients about outstanding balances. Following up on unpaid invoices is crucial for timely payment collection and helps prevent accounts from becoming delinquent.
Accepting various payment methods
To facilitate payment collection, healthcare providers should offer various payment methods to patients. This includes accepting cash, checks, credit cards, and online payments. Offering multiple payment options ensures convenience for the patients and increases the likelihood of prompt payment. Accepting various payment methods streamlines the payment collection process and boosts overall revenue management.
Resolving payment disputes
In some cases, patients may dispute the payment amount or have questions regarding the charges. It is important to address these concerns promptly and resolve payment disputes amicably. Open and effective communication with patients can help prevent misunderstandings and maintain a positive relationship. Resolving payment disputes in a timely manner ensures smooth payment collection and patient satisfaction.
Insurance Reimbursement
Reviewing and reconciling reimbursement amounts
Once insurance reimbursements are received, it is important to review and reconcile the payment amounts with the original claims. This helps ensure accurate reimbursement and identify any discrepancies or underpayments. Reviewing and reconciling reimbursement amounts allows healthcare providers to address any issues with the insurance company promptly and seek appropriate reimbursement.
Dealing with denied or underpaid claims
In some cases, insurance companies may deny or underpay claims. When this happens, healthcare providers need to take appropriate action to appeal denials or request reevaluation for underpayments. This may involve providing additional documentation, clarifications, or appeals. Dealing with denied or underpaid claims requires persistence and proactive communication with the insurance company to ensure fair reimbursement.
Patient Billing and Follow-Up

Providing billing statements to patients
In addition to invoices, healthcare providers should also provide detailed billing statements to patients upon request. Billing statements include a summary of all charges, payments, and adjustments. Providing billing statements allows patients to review and verify the accuracy of their bills. This level of transparency promotes trust and facilitates clear communication between healthcare providers and patients.
Responding to patient inquiries and concerns
During the billing process, patients may have inquiries or concerns regarding their bills. It is important to respond to these inquiries promptly and address any concerns or questions raised by the patients. Open and clear communication fosters patient satisfaction and trust. Responding to patient inquiries and concerns helps build strong patient-provider relationships and supports a positive billing experience.
Conclusion
Efficiently managing the medical billing process is crucial for healthcare providers to receive timely and accurate reimbursement. By following these steps, healthcare organizations can streamline their billing operations and improve overall revenue cycle management. Collecting patient information, verifying insurance coverage, updating patient records, documenting diagnoses and procedures, submitting claims, processing claims, generating invoices, collecting payments, and following up on patient billing are all integral parts of the medical billing process. Adhering to these steps and maintaining compliance with coding and billing guidelines ensures smooth claim processing and reimbursement, ultimately supporting the financial stability of healthcare providers.