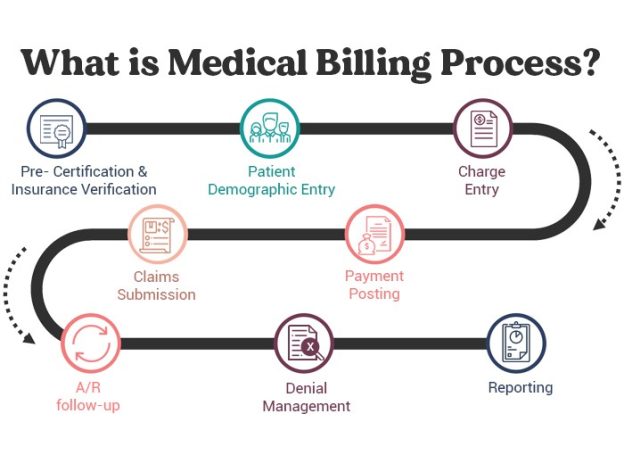
In the field of medical billing, ensuring accuracy and efficiency is of utmost importance. Quality checks play a vital role in safeguarding against errors and improving overall billing processes. From verifying patient information to reviewing coding accuracy, these checks encompass a wide range of measures that contribute to the successful management of medical billing. This article explores the key quality checks involved in medical billing, highlighting their significance in maintaining integrity and maximizing reimbursement potential.
Claim Verification
Patient Demographics
Claim verification begins with ensuring accurate patient demographics. This includes verifying the patient’s full name, date of birth, address, contact number, and insurance information. Accurate and up-to-date patient demographics are crucial for proper claim processing and to avoid claim denials or delays.
Insurance Information
Verifying insurance information is a critical step in medical billing. It involves confirming the patient’s insurance coverage, policy number, group number, and effective dates. This helps determine the patient’s eligibility for services and ensures that claims are submitted to the correct insurance provider. Inaccurate or outdated insurance information can result in claim denials and delayed payments.
Medical Necessity
Before submitting a claim, it is essential to ensure that the services provided are medically necessary. Medical necessity means that the services or procedures performed are appropriate and required for the patient’s diagnosis or condition. This can be verified by reviewing the medical documentation and ensuring that it supports the services billed. Failure to establish medical necessity may result in claim denials or audits.
Coding Accuracy
Current Procedural Terminology (CPT) Codes
Accurate coding is crucial for proper claim submission. CPT codes are used to describe the services or procedures performed by healthcare providers. These codes are standardized and must be selected appropriately based on the services rendered. It is essential to review the medical documentation thoroughly to determine the correct CPT codes. Incorrect or mismatched CPT codes can lead to claim denials or underpayments.
International Classification of Diseases (ICD) Codes
ICD codes are used to classify and describe the patient’s diagnosis or condition. These codes are essential for proper claim submission and reimbursement. It is crucial to select the most accurate and specific ICD codes based on the documentation provided by the healthcare provider. Using incorrect or outdated ICD codes may lead to claim denials or delays in reimbursement.
Healthcare Common Procedure Coding System (HCPCS) Codes
HCPCS codes are used for additional procedures, services, supplies, and equipment not covered by CPT codes. These codes are used primarily for Medicare and Medicaid billing. Like CPT and ICD codes, accuracy in selecting the appropriate HCPCS codes is crucial. Errors in HCPCS coding can result in claim denials or incorrect reimbursement.
Charge Entry
Service Description and Dates
When entering charges into the billing system, it is essential to provide a detailed description of the services or procedures performed. This includes specifying the date of service, the location, and any additional relevant details. Accurate service descriptions and dates help ensure that claims are processed correctly and facilitate easy claim tracking.
Correct Codes and Units
In charge entry, it is crucial to enter the correct CPT, ICD, and HCPCS codes associated with the services provided. The codes must match the procedures performed and the diagnosis documented in the medical records. Additionally, entering the correct number of units is important for accurate reimbursement. Mistakes in code selection or unit entry can lead to claim denials or reduced payment.
Modifiers and Pricing
Modifiers are used to provide additional information about the service or procedure performed. They can indicate changes in the procedure, multiple procedures, or specific circumstances. Accuracy in assigning modifiers is crucial, as incorrect or missing modifiers may result in claim denials or underpayment. Additionally, ensuring correct pricing for each service or procedure is essential to receive accurate reimbursement.
Insurance Eligibility
Verification of Insurance Coverage
Before services are rendered, it is important to verify the patient’s insurance coverage. This involves contacting the insurance provider to confirm the patient’s eligibility, benefits, and any specific requirements or limitations. Verifying insurance coverage helps avoid claim denials and ensures that the patient’s services are appropriately covered.
Effective Coverage Dates
Insurance coverage may have specific effective dates, which must be verified and considered when providing services. It is important to ensure that the services are rendered within the coverage period to avoid claim denials or patient responsibility for the charges. Accurate identification of the effective coverage dates is crucial for successful claim submission and reimbursement.
Pre-authorization Requirements
Certain procedures or services may require pre-authorization from the insurance provider. It is necessary to verify if pre-authorization is needed and obtain it before performing the service. Failure to obtain pre-authorization may result in claim denials or the patient being held responsible for the charges. Proper management of pre-authorization requirements helps ensure timely payment and reduces the risk of claim denials.
Medical Documentation
Provider’s Notes and Documentation
Accurate and detailed medical documentation is the backbone of successful claim submission. It is important to review the healthcare provider’s notes and documentation to ensure they support the services or procedures billed. The documentation should clearly establish the medical necessity, describe the services provided, and demonstrate the patient’s condition or diagnosis. Incomplete or inadequate documentation can lead to claim denials or audits.
Procedure and Diagnosis Documentation
Medical documentation should include clear and detailed descriptions of the procedures performed and the patient’s diagnosis. The procedure documentation should outline any necessary information, such as the anatomical location and the extent of the service provided. Similarly, diagnosis documentation should be specific and detailed to support the medical necessity of the services rendered. Accurate procedure and diagnosis documentation are crucial for successful claim submission and reimbursement.
Supporting Medical Reports and Records
In addition to the provider’s notes, supporting medical reports and records should also be reviewed for accuracy and completeness. These reports may include laboratory results, imaging studies, or consultation reports. These supporting documents help establish the medical necessity and provide additional evidence to support the services billed. Thoroughly reviewing the supporting medical reports helps ensure accurate claim submission and reduces the risk of claim denials.
Claims Submission
Submission of Clean Claims
Submitting a clean claim means providing all the necessary information accurately and completely to the insurance provider. This includes ensuring that all required fields are filled, proper codes are assigned, and documentation is attached as needed. Submitting clean claims increases the chances of timely and accurate reimbursement and reduces the likelihood of claim denials or rework.
Timeliness of Claim Filing
Claims should be submitted within the specified time frame defined by the insurance provider. It is crucial to understand and adhere to these timelines to avoid claim denials due to late filing. Timely claim filing helps ensure prompt payment and reduces the risk of lost revenue or delayed reimbursement.
Correct Billing Address and Contact Information
When submitting claims, it is vital to double-check and verify the correct billing address and contact information for the insurance provider. Inaccurate or outdated information may result in claim rejections or delays in processing. Providing the correct billing address and contact information ensures that the claims reach the intended recipient and facilitates timely communication regarding any inquiries or issues.
Claims Adjudication
Verification of Claim Processing
Once claims are submitted, it is important to verify that they are being processed by the insurance provider. This can be done by regularly monitoring the status of the claims through electronic portals or by following up with the insurance company. Verifying claim processing helps identify any potential issues or delays and allows for prompt action or follow-up.
Approval or Denial Determination
After processing, claims are either approved or denied by the insurance provider. It is crucial to carefully review the determination and understand the reasons for denial, if applicable. Approved claims should move forward for reimbursement, while denied claims require further action such as appeals or resubmission. Accurate determination of approval or denial allows for appropriate action to be taken, ensuring maximum reimbursement.
Proper Reimbursement Calculation
When claims are approved, the insurance provider calculates the reimbursement amount based on the contracted rates. It is essential to review the reimbursement calculations to ensure accuracy. Any discrepancies or underpayments should be identified and addressed promptly. Proper reimbursement calculation helps optimize revenue and ensures that providers are appropriately compensated for their services.
Accounts Receivable
Follow-up on Unpaid Claims
Accounts receivable management involves diligent follow-up on unpaid or unresolved claims. Regularly monitoring the status of unpaid claims helps identify any delays or issues in reimbursement. Following up with insurance providers allows for the identification and resolution of claim denials, underpayments, or any other billing discrepancies. Timely follow-up on unpaid claims is crucial for optimum revenue management.
Identifying Claim Rejections
Claim rejections occur when a claim cannot be processed due to errors or missing information. It is important to identify and resolve claim rejections promptly to avoid delayed reimbursement. Analyzing claim rejections helps identify any patterns or common errors, allowing for corrective action and process improvement.
Resolving Billing Discrepancies
Billing discrepancies may arise due to various reasons, such as incorrect coding, missing information, or billing errors. Promptly addressing billing discrepancies helps minimize delays in reimbursement and ensures accurate financial records. Resolving billing discrepancies requires close collaboration with the insurance provider and thorough investigation of the root causes of the discrepancies.
Payment Posting
Verification of Payments
After claims are approved, payments are received from the insurance provider. It is essential to verify the accuracy of the payments received. This involves cross-referencing the payment amount with the expected reimbursement amount and ensuring that any contractual adjustments or patient responsibilities are appropriately applied. Verifying payments helps identify any underpayments or overpayments that may require further action.
Correct Allocation of Payments
Once payments are verified, they need to be allocated correctly to the respective accounts or invoices. It is essential to accurately allocate payments to ensure proper financial records and to prevent any confusion or discrepancies. Correct allocation of payments contributes to efficient revenue management and maintains accurate account balances.
Identification of Underpayments or Overpayments
During payment posting, it is important to identify any underpayments or overpayments that may have occurred. Underpayments can be addressed through timely appeals or follow-up with the insurance provider to ensure proper reimbursement. Overpayments should be promptly refunded to the insurance provider to maintain compliance and financial integrity. Proper identification and management of underpayments or overpayments help maintain a balanced revenue cycle.
Denial Management
Identification and Analysis of Denials
Denial management involves identifying and analyzing claim denials to understand the underlying reasons. This includes reviewing denial codes, claims data, and documentation to identify patterns or trends. Proper analysis of denials helps identify areas of improvement, such as coding errors, documentation deficiencies, or pre-authorization issues. By addressing the root causes of denials, the overall denial rate can be reduced, resulting in improved revenue and claims processing.
Appealing Denied Claims
Denied claims that are deemed to be eligible for reimbursement should be appealed within the specified time frame. The appeals process involves providing additional documentation or clarification to support the medical necessity of the services rendered. Accurate and persuasive appeals can overturn claim denials and result in proper reimbursement. Timely and effective appeals management is crucial for revenue optimization.
Implementing Corrective Actions
Analyzing denials and appeals data helps identify areas for process improvement and corrective actions. These actions may involve updating coding guidelines, enhancing documentation practices, or improving communication with insurance providers. Implementing corrective actions helps prevent future denials and enhances the overall efficiency and effectiveness of the medical billing process.
In conclusion, quality checks in medical billing encompass various aspects, including claim verification, coding accuracy, charge entry, insurance eligibility, medical documentation, claims submission, claims adjudication, accounts receivable, payment posting, denial management, and implementing corrective actions. Following these quality checks diligently and ensuring accuracy at each step helps optimize revenue, reduce claim denials or rework, and maintain compliance in the complex world of medical billing.