Introduction
What is medical billing?
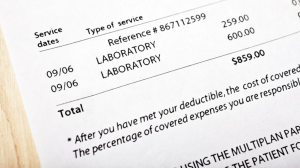
If you’ve ever visited a medical professional, you’ve likely seen a bill for their services. This is medical billing, the process of submitting and following up on insurance claims in order to receive reimbursement for healthcare services.
Why is medical billing important?
Medical billing serves as a crucial component of any healthcare facility. It not only ensures timely payment and cash flow for providers, but also helps patients navigate the complex healthcare system and understand their coverage, benefits, and financial responsibilities.
Who uses medical billing?
Medical billing is used by healthcare providers such as hospitals, clinics, and private practices, as well as insurance companies, government agencies, and patients.
How does medical billing work?
The medical billing process involves creating and submitting claims to insurance companies, verifying patient eligibility and coverage, following up on payment status, and dealing with any denials or rejections. It requires skilled workers who are familiar with the intricacies of medical coding and insurance regulations. Knowing the basics of medical billing can provide you with a better understanding of the cost of healthcare and how insurance works.
Medical Billing Basics
Medical billing is the process of submitting and following up on claims with health insurance companies. It is an essential part of healthcare administration and revenue cycle management. In this section, you will learn about medical coding, the claims and billing process, reimbursement methods, and patient and insurance information.
Medical Coding
Medical coding is the process of translating healthcare services into standardized codes that insurance companies can understand. Medical coders use a system called ICD-10 (International Classification of Diseases, 10th Revision) and CPT (Current Procedural Terminology) codes to bill insurance companies accurately.
Claims and Billing Process
The claims and billing process involves submitting claims to insurance companies for reimbursement. The process includes verifying patient insurance information, submitting claims, following up on claim denials, and appealing rejected claims.
Reimbursement Methods
Reimbursement methods include fee-for-service, capitation, and bundled payments. Fee-for-service is the most common method, where insurers pay providers for each service rendered. Capitation and bundled payments involve paying providers a set amount of money per patient or treatment.
Patient and Insurance Information
Patient and insurance information is crucial to the claims and billing process. It includes patient demographics, insurance coverage, copayments, deductibles, and pre-existing conditions. Accurate and up-to-date information is necessary for successful claims and billing.
Understanding medical billing basics is essential for healthcare providers and their staff. It helps to ensure accurate reimbursements and revenue collection while meeting regulatory compliance.
Medical Billing Software

Benefits of using medical billing software
If you want to streamline your medical billing process, you should consider using medical billing software. The benefits include increased accuracy, faster reimbursements, and improved organization. With medical billing software, you can easily track claims and payments, automate tasks, and reduce errors. Additionally, medical billing software can help you stay up-to-date with industry changes, such as new reimbursement rules, and help you avoid costly fines and penalties.
Top medical billing software providers
There are many medical billing software providers on the market, but some of the most popular include AdvancedMD, Kareo, and Athenahealth. These providers offer a range of features and pricing options to meet the needs of various medical practices.
Features to look for in medical billing software
When choosing a medical billing software provider, it’s important to consider features such as automated claim submission and tracking, detailed reporting, and HIPAA compliance. Additionally, you should ensure that the software integrates with other practice management tools, such as scheduling and EMR systems.
Costs associated with medical billing software
The cost of medical billing software varies depending on the provider and the features included. Some providers offer subscription-based pricing models while others charge per claim. It’s important to consider not only the upfront costs but also ongoing support and training fees. Ultimately, choosing a high-quality medical billing software provider can save you time, money and improve the overall efficiency of your practice.
Medical Billing Regulations
When it comes to medical billing, there are various regulations that you need to be aware of to ensure that you are in compliance. Here are some of the most important regulations to keep in mind:
HIPAA Regulations
HIPAA (Health Insurance Portability and Accountability Act) regulations protect the privacy and security of patients’ personal health information. As a medical biller, it’s crucial that you understand these regulations and take steps to ensure that you are handling patient information in a safe and secure manner.
Compliance Guidelines
In addition to HIPAA regulations, there are other compliance guidelines that you need to follow to avoid penalties and fines. This includes adhering to the False Claims Act, which prohibits submitting false claims to Medicare or Medicaid.
ICD-10 Codes
ICD-10 codes are used to classify and code diagnoses and procedures. Understanding these codes is essential for accurate billing and coding.
Current Procedural Terminology (CPT) Codes
CPT codes are used to describe medical procedures and services. As a medical biller, you need to be familiar with these codes so that you can accurately bill for the services provided.
Overall, understanding medical billing regulations is essential for accurate and ethical billing. Make sure you stay up-to-date on all the latest regulations to ensure that you are doing everything right.
Dealing with Denials and Appeals
Medical billing can be a complex and frustrating process. Even after you submit your claims, there is no guarantee that they will be accepted. You may receive claim denials for many reasons, including billing errors or lack of medical necessity. But don’t worry – there are ways to appeal denied claims and reduce denials in the future.
Reasons for claim denials
It’s important to understand the common reasons for claim denials so that you can avoid them in the future. Some common reasons include incomplete or inaccurate information, missing documentation, and incorrect coding. It’s also important to make sure that you are submitting claims for services that are deemed medically necessary.
Appealing denied claims
If you receive a claim denial, don’t give up! You have the right to appeal the decision. This process involves gathering additional documentation and evidence to show why the claim should be paid. It’s important to follow the appeals process carefully and provide all necessary information to increase your chances of success.
Best practices for reducing denials
To reduce the number of claim denials, make sure that you are submitting accurate and complete information. Double-check your coding and ensure that you have all necessary documentation. It’s also important to regularly review your billing processes and make adjustments as necessary.
Handling delinquent accounts
When patients don’t pay their bills on time, it can be challenging to collect the debt. It’s important to have policies and procedures in place for handling delinquent accounts, including sending reminder notices and working with collection agencies as necessary.
By understanding how to handle claim denials and delinquent accounts, you can navigate the world of medical billing with confidence.
Medical Billing Careers
If you are interested in pursuing a career in medical billing, there are several things you should know. Medical billing requires a knowledge of medical coding and insurance regulations, as well as attention to detail and strong communication skills.
Education Requirements for Medical Billing Positions
Most medical billing positions require at least a high school diploma or equivalent, but many employers prefer candidates with an associate’s or bachelor’s degree in healthcare administration or a related field. Additionally, certification as a Certified Professional Biller or Certified Professional Coder may be required or preferred by some employers.
Types of Medical Billing Jobs
Medical billing professionals can work in a variety of settings, including hospitals, clinics, physician offices, insurance companies, and billing and coding firms. Some common job titles in this field include Medical Biller, Medical Coder, Billing Specialist, Revenue Cycle Manager, and Claims Processor.
Average Salary for Medical Billing Professionals
The average salary for medical billing professionals varies depending on experience, education, and location. According to the Bureau of Labor Statistics, the median annual wage for medical records and health information technicians, which includes medical billers and coders, was $42,630 as of May 2020.
Future Outlook for Medical Billing Careers
The demand for medical billing professionals is expected to remain strong in the coming years, with an estimated 8% job growth from 2019 to 2029. With the aging population and increasing need for healthcare services, the medical billing field offers promising career opportunities.
Choosing a Medical Billing Company
When it comes to medical billing, choosing the right company to handle your billing needs is crucial to ensuring smooth operations and timely payments. Here are some factors to consider when choosing a medical billing company:
Factors to consider when choosing a medical billing company
- Experience: Look for a company with a solid track record in medical billing, and preferably experience in your specific field.
- Technology: Ideally, the medical billing company should be using the latest billing software and have a system for keeping track of claims and payments.
- Services offered: Make sure the company offers the services you need, whether that be coding, claim submission, or payment posting.
- Pricing: Look for a company that provides transparent pricing, and consider whether the cost is worth the benefits they offer.
Questions to ask a potential medical billing provider
- How long have you been in business?
- What percentage of claims are usually paid within 30 days?
- What is your process for handling denied claims?
- Do you have experience working with my specific type of practice or specialty?
Signs of a reputable medical billing company
- Clear communication channels
- Regular reporting on claims and payments
- Certifications or accreditations
- Positive reviews from other healthcare providers
How much does outsourcing medical billing cost?
The cost of outsourcing medical billing varies depending on the company and the specific services you need. However, many medical billing companies charge a percentage of the revenue collected, typically ranging from 4% to 10%. Keep in mind that while outsourcing medical billing may seem expensive at first, it can actually save you money in the long run by ensuring timely payments and minimizing billing errors.
Resources
When it comes to medical billing, it’s important to have access to reliable resources. Here are a few organizations that can provide helpful information and guidance:
American Medical Billing Association
The AMBA is a professional association dedicated to medical billing and coding professionals. They offer education, certification, and resources to help you stay up-to-date with the latest changes in the industry.
Healthcare Information and Management Systems Society (HIMSS)
HIMSS is a global organization focused on improving healthcare delivery through the use of technology. They offer resources and networking opportunities to help you stay current with the latest innovations in healthcare IT.
Medical Group Management Association
The MGMA is a professional organization focused on helping medical practice managers and administrators. They offer education, certification, and resources to help you navigate the complex world of medical billing and healthcare management.
Centers for Medicare and Medicaid Services
CMS is a federal agency that administers Medicare, Medicaid, and other healthcare programs. They offer a wide range of resources and information on billing and coding for healthcare providers.
By utilizing these resources and staying informed about the latest developments in medical billing, you can ensure that you are providing the best possible service to your patients.
