In this article, you will learn about the three main types of medical coding. We will discuss each type briefly, providing you with a clear understanding of their purpose and how they are used in the healthcare industry. By the end, you will have a solid grasp of the different coding systems and their importance in accurately documenting and classifying medical procedures, diagnoses, and services. So, read on to expand your knowledge of medical coding!
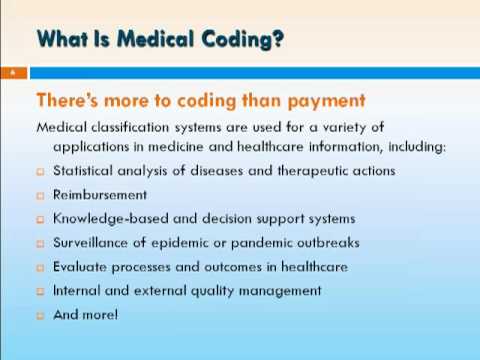
Introduction to Medical Coding
Medical coding is an essential aspect of the healthcare industry, as it involves the transformation of medical diagnoses, procedures, and services into numeric and alphanumeric codes. These codes are used for various purposes, such as insurance reimbursement, medical research, statistical analysis, and ensuring legal and ethical compliance. In this article, we will explore the three main types of medical coding: ICD-10 coding, CPT coding, and HCPCS coding. Understanding these coding systems is crucial for healthcare professionals involved in medical billing, coding, and documentation.
ICD-10 Coding
Introduction to ICD-10 Coding
ICD-10 coding, or the International Classification of Diseases, Tenth Revision, is a system used worldwide for classifying diseases, injuries, and other health conditions. This coding system is maintained by the World Health Organization (WHO) and is currently adopted by most countries, replacing the older ICD-9 coding system. ICD-10 codes are alphanumeric and provide a standardized way to categorize and record diagnoses.
Purpose of ICD-10 Coding
The primary purpose of ICD-10 coding is to provide a common language for describing health conditions across different healthcare settings and ensure accurate and consistent documentation. These codes capture important details about diseases and conditions, allowing healthcare providers to communicate effectively with insurers, researchers, and other healthcare professionals.
ICD-10 Code Structure
ICD-10 codes are composed of up to seven alphanumeric characters, which include a combination of letters and numbers. The first three characters represent the category of the disease or condition, while the subsequent characters provide more specific information, such as etiology, severity, and anatomical location. For example, the code I20.0 represents angina pectoris of unspecified type, while I42.0 represents dilated cardiomyopathy.
Benefits of ICD-10 Coding
The implementation of ICD-10 coding brings several benefits to the healthcare industry. Firstly, it allows for more detailed and precise classification of diseases and conditions, leading to improved accuracy in medical documentation and research. Additionally, ICD-10 codes provide a standardized language that enables better communication between healthcare providers, insurers, and other stakeholders. Furthermore, the increased specificity of ICD-10 codes enhances the ability to track and analyze various health conditions, contributing to improved public health initiatives and resource allocation.
Challenges of ICD-10 Coding
Although ICD-10 coding has numerous advantages, it also presents certain challenges. The transition from ICD-9 to ICD-10 required extensive training and education for healthcare professionals due to the increased complexity and number of codes. Moreover, the specificity of ICD-10 codes sometimes makes it difficult to select the most appropriate code, leading to potential errors in documentation. Furthermore, maintaining up-to-date knowledge of the constantly evolving guidelines and updates in the ICD-10 coding system can be a challenge for healthcare professionals.
CPT Coding
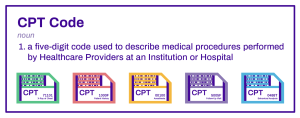
Introduction to CPT Coding
CPT coding, or Current Procedural Terminology coding, is a system developed and maintained by the American Medical Association (AMA). This coding system is primarily used in the United States to report medical procedures and services. CPT codes are numeric and provide a standardized way to document and bill for medical procedures performed by healthcare professionals.
Purpose of CPT Coding
The purpose of CPT coding is to communicate and identify specific medical procedures accurately, enabling consistent billing, reimbursement, and tracking of healthcare services. These codes provide a common language for healthcare providers, insurers, and policymakers to understand the services rendered, facilitating accurate reimbursement and resource allocation.
CPT Code Structure
CPT codes consist of five-digit numeric codes, with each code representing a unique medical procedure or service. The codes are divided into three categories: Category I, Category II, and Category III. Category I codes represent the most common and widely used procedures, while Category II codes are supplementary tracking codes used for performance measurement. Category III codes are temporary codes for emerging technologies, services, and procedures still undergoing evaluation.
Benefits of CPT Coding
CPT coding offers several advantages in the healthcare industry. Firstly, it provides a uniform system for reporting medical procedures and services, ensuring consistent and accurate billing across healthcare settings. Secondly, CPT codes allow for efficient tracking and analysis of healthcare utilization and trends, facilitating evidence-based decision-making and policy development. Moreover, CPT coding enhances communication between healthcare providers and insurers, reducing the potential for misunderstandings or disputes regarding billed services.
Challenges of CPT Coding
While CPT coding streamlines the process of documenting and billing medical procedures, it also poses certain challenges. One of the main challenges is the constant updates and revisions of CPT codes, requiring healthcare professionals to stay updated with the latest coding guidelines. Additionally, the complexity of certain procedures may make it challenging to accurately assign the most appropriate code. Furthermore, errors in CPT coding can result in claim denials, delayed payments, and potential legal implications, underscoring the importance of training and accuracy in coding practices.
HCPCS Coding

Introduction to HCPCS Coding
HCPCS coding, or Healthcare Common Procedure Coding System coding, is a system used in the United States for reporting healthcare services and supplies to Medicare and other insurance programs. HCPCS codes are used primarily for procedures, services, and supplies that are not covered by CPT codes, such as durable medical equipment, ambulance services, and supplies for specific patient populations.
Purpose of HCPCS Coding
The purpose of HCPCS coding is to provide a standardized system for documenting and reporting healthcare services, supplies, and equipment. These codes allow for accurate and consistent billing, reimbursement, and utilization tracking for services not covered under CPT coding.
HCPCS Code Structure
HCPCS codes are alphanumeric and consist of a single letter followed by four numeric digits. The letter at the beginning of the code indicates the specific category of the service or supply, while the subsequent digits provide further specificity and description. For example, the code E0601 represents a continuous positive airway pressure (CPAP) device, while A0427 represents ground mileage of an ambulance.
Benefits of HCPCS Coding
HCPCS coding offers several benefits to the healthcare industry. Firstly, it provides a standardized language for reporting and billing non-CPT services and supplies, ensuring accurate reimbursement and resource tracking. Secondly, HCPCS codes allow for efficient utilization analysis and identification of specific patient populations or services that require additional attention or monitoring. Moreover, HCPCS coding enhances transparency and consistency in reporting, enabling effective communication between healthcare providers, insurers, and regulatory bodies.
Challenges of HCPCS Coding
Like any coding system, HCPCS coding presents certain challenges. The complexity and specificity of HCPCS codes may require extensive training and knowledge to accurately assign the appropriate code to a given service or supply. Additionally, as with other coding systems, HCPCS codes undergo regular updates and revisions, necessitating ongoing education and understanding of the latest coding guidelines. Furthermore, errors in HCPCS coding can result in claim denials and delays in reimbursement, highlighting the importance of accuracy and attention to detail.
Comparison of the Three Types of Medical Coding
Now that we have discussed the main types of medical coding individually, let’s compare them based on various factors.
Differences in Code Structures
ICD-10 codes are alphanumeric and provide a high level of specificity, capturing detailed information about diagnoses. CPT codes, on the other hand, are numeric and focus on reporting medical procedures and services. HCPCS codes are also alphanumeric and primarily used for reporting non-CPT services and supplies.
Specific Uses and Applications
ICD-10 coding is used for documenting and tracking diagnoses and allows for efficient data analysis and research. CPT coding is essential for billing and reimbursement purposes, providing a standardized method for reporting medical procedures. HCPCS coding is specifically used for reporting non-CPT services and supplies and is primarily utilized in programs like Medicare.
Complexity and Training Requirements
ICD-10 coding is considered more complex than the other two coding systems due to its extensive code structure and specificity. Healthcare professionals need comprehensive training to accurately assign ICD-10 codes. CPT coding requires in-depth knowledge of medical procedures, while HCPCS coding focuses on specific services and supplies not covered by CPT codes.
Reimbursement and Insurance Billing
All three coding systems play a vital role in reimbursement and insurance billing. Proper coding ensures accurate and timely reimbursement for healthcare services rendered. Insurers and payers use these codes to determine the appropriate reimbursement rates and coverage.
Integration with Electronic Health Records
Medical coding is an integral component of electronic health records (EHRs). Proper coding allows for efficient documentation, retrieval, and analysis of patient data within an EHR system. Integration of coding systems with EHRs provides a comprehensive and accurate picture of a patient’s healthcare history.
Career Opportunities in Medical Coding
Professionals with expertise in medical coding are in high demand in the healthcare industry. Here are some career opportunities in medical coding:
Medical Coding Specialist
Medical coding specialists are responsible for assigning appropriate codes to diagnoses, procedures, and services. They ensure accurate documentation and compliance with coding guidelines, as well as resolve coding-related issues and discrepancies.
Coding Auditor
Coding auditors review medical records and coding practices to ensure compliance with coding guidelines and accuracy in coding assignments. They identify coding errors or discrepancies and provide feedback and recommendations for improvement.
Coding Supervisor
Coding supervisors oversee and manage a team of medical coders. They ensure the accurate and timely coding of medical records, provide training and guidance to coding staff, and monitor coding performance and productivity.
Coding Educator
Coding educators develop and deliver training programs and educational materials to healthcare professionals, ensuring they are knowledgeable and up to date with coding guidelines and best practices.
Medical Billing Specialist
Medical billing specialists are responsible for submitting claims to insurance companies, verifying insurance coverage, and ensuring accurate and timely reimbursement for healthcare services rendered. They are proficient in medical coding and billing software.
Importance of Accurate Medical Coding
Accurate medical coding is crucial for several reasons:
Ensuring Reimbursement
Accurate coding ensures that healthcare providers are properly reimbursed for the services and procedures they provide. Proper coding prevents claim denials, reduces payment delays, and facilitates the financial stability of healthcare organizations.
Facilitating Proper Patient Care
Accurate coding leads to comprehensive and detailed medical documentation, which is essential for proper patient care. Medical codes allow healthcare professionals to access relevant patient information quickly, make informed decisions, and provide appropriate treatment.
Conforming to Legal and Ethical Standards
Medical coding must comply with legal and ethical standards, ensuring proper billing and documentation practices. Accurate coding helps prevent fraudulent activities, such as upcoding or unbundling services, and promotes transparency and accountability in healthcare.
Supporting Medical Research and Statistics
Medical coding plays a crucial role in medical research and the generation of healthcare statistics. Researchers rely on coded data to analyze disease patterns, treatment outcomes, and overall population health. Accurate coding ensures the integrity and reliability of research findings.
Preventing Fraud and Abuse
Accurate coding helps prevent fraudulent activities by providing a clear and traceable record of services rendered. Proper coding practices help detect and prevent instances of unnecessary or fraudulent billing, protecting both patients and healthcare organizations.
Challenges and Future Trends in Medical Coding
Medical coding faces several challenges and is subject to ongoing trends and developments. Here are some key challenges and future trends in medical coding:
Constantly Evolving Guidelines and Standards
Medical coding guidelines and standards are subject to frequent updates and revisions. Healthcare professionals must stay updated with the latest coding changes and guidelines to ensure accurate coding practices.
Increasing Demand for Coding Professionals
As healthcare systems evolve and expand, the demand for qualified medical coding professionals continues to grow. Medical coders with in-depth knowledge and expertise in specific coding systems are highly sought after.
Integration of Artificial Intelligence
Artificial intelligence (AI) technologies are being increasingly integrated into medical coding processes. AI algorithms are used to assist in assigning codes, detecting errors, and improving coding efficiency and accuracy.
Emphasis on Data Analytics
The abundance of coded data in healthcare systems provides opportunities for in-depth data analysis and analytics. Data-driven insights derived from coded data can assist in identifying patterns, improving patient outcomes, and optimizing healthcare resource allocation.
Automation and Coding Software
Advancements in technology have led to the development of coding software and automated coding systems. These tools streamline coding processes, reduce errors, and improve productivity. However, the role of human coders remains crucial in ensuring the accuracy and integrity of coded data.
Conclusion
In conclusion, medical coding is an integral part of the healthcare industry, enabling accurate documentation, billing, and reimbursement of healthcare services. The three main types of medical coding – ICD-10 coding, CPT coding, and HCPCS coding – serve different purposes and are essential for various aspects of healthcare delivery. Understanding these coding systems is crucial for healthcare professionals involved in medical billing, coding, and documentation. Accurate coding is vital for facilitating proper patient care, ensuring reimbursement, and conforming to legal and ethical standards. Although medical coding faces challenges, such as evolving guidelines and increasing demands, ongoing developments in technology and data analytics offer promising opportunities for the future of medical coding.