In today’s ever-evolving healthcare landscape, medical billing denial management software has become an invaluable tool for healthcare providers and medical billing professionals. By streamlining the claims process and effectively managing denials, this software significantly improves revenue cycle management and helps maintain a steady cash flow. In this article, you will learn essential steps and best practices on how to effectively utilize medical billing denial management software, ensuring accurate claim submissions and maximizing reimbursement potential.
Setting Up the Software
Installation and Configuration
Before you can start using medical billing denial management software, you need to install and configure it on your system. Follow the vendor’s instructions for installation, which typically involve running an installer or downloading the software from a website. Once the software is installed, you will need to configure it by providing necessary information such as your practice details and billing preferences. This step is important as it will ensure that the software is tailored to your specific needs and requirements.
Adding Users and Permissions
To efficiently utilize medical billing denial management software, it is crucial to set up user accounts and assign appropriate permissions. This will allow different staff members in your practice to access and perform specific tasks within the software. For example, you may want to grant billing staff the ability to submit claims and manage denials, while limiting front desk staff to only accessing patient information. By carefully defining user roles and permissions, you can maintain data security and ensure that each individual has the necessary access to perform their job responsibilities.
Setting Up Insurance Companies
Configuring insurance companies within the software is essential for accurate billing and claims management. In this step, you will need to enter information about the insurance companies your practice works with, such as their names, contact details, and specific requirements for billing. This will enable the software to correctly process claims and communicate with the insurance companies when necessary, ensuring a smoother billing process.
Configuring Billing Rules
To streamline the billing process, it is important to configure billing rules within the software. These rules define how the software should handle specific billing scenarios, such as the allowed fees for different services, the maximum number of allowable units, and the modifiers applicable to certain procedures. By setting up these rules, you can ensure that claims are generated accurately and in accordance with industry standards and guidelines.
Navigating the User Interface
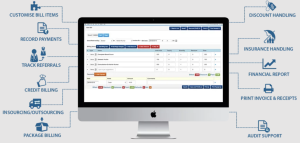
Dashboard Overview
The dashboard is the main screen you will see when you log in to the medical billing denial management software. It provides a high-level overview of key performance indicators, such as the number of claims in different stages of processing, the amount of outstanding payments, and any denials or rejections that require attention. The dashboard allows you to quickly assess the overall health of your billing cycle and identify areas that may need further investigation or action.
Menu and Navigation
To efficiently navigate the software, familiarize yourself with the menu and navigation options provided. The menu typically consists of different modules or sections, such as patient management, claim management, denial management, reporting, and settings. Each module will have its own set of submenus and options that allow you to perform specific tasks related to that area. Take the time to explore these menus and understand their functionality so that you can easily access the features you need.
Search and Filter Functions
The ability to search and filter data within the software is essential for efficient claim and denial management. The search function allows you to quickly find specific patients, claims, or denials by entering relevant keywords or criteria. Additionally, the filter function enables you to narrow down the data displayed based on specific attributes or parameters. By utilizing these search and filter functions effectively, you can save time and focus on the information that is most relevant to your tasks.
Customizing the User Interface
Medical billing denial management software often provides options to customize the user interface to suit your preferences and workflow. This may include rearranging menu items, adjusting the layout of screens, and choosing which data fields are displayed. By customizing the user interface, you can optimize your workflow and ensure that the most important information is readily available for efficient processing and decision-making.
Entering Patient Information
Creating and Updating Patient Profiles
Accurate and up-to-date patient profiles are essential for effective billing and claims management. Within the medical billing denial management software, you can create new patient profiles by entering relevant information such as the patient’s name, contact details, insurance information, and demographic data. It is also important to regularly update patient profiles with any changes in contact information or insurance coverage to ensure accurate billing and claim submission.
Entering Insurance Details
To accurately bill insurance companies, it is crucial to enter insurance details within the patient profiles. This includes information such as the insurance company’s name, policy number, group number, and any specific requirements or limitations associated with the insurance policy. By correctly inputting insurance details, you can streamline the claims submission process and minimize denials or rejections due to incorrect or incomplete information.
Linking Patient Records to Service Codes
To streamline the billing process, it is important to link patient records to the appropriate service codes within the software. Service codes, such as Current Procedural Terminology (CPT) codes, represent the specific services or procedures performed by healthcare providers and are used for billing purposes. By linking patient records to the appropriate service codes, you can generate claims accurately and ensure that the services provided are properly represented in the billing process.
Managing Patient Contact Information
Keeping patient contact information up to date is crucial for effective communication and billing. Within the medical billing denial management software, you can easily manage and update patient contact information, including phone numbers, email addresses, and mailing addresses. This ensures that any necessary communication regarding claims, denials, or payment inquiries can be sent to the correct recipient and minimizes the risk of delayed or missed notifications.
Submitting Claims
Generating and Reviewing Claims
Generating claims is a fundamental function of medical billing denial management software. The software allows you to generate claims based on the services provided to patients and the associated service codes. Before submitting the claims, it is important to review them to ensure accuracy and completeness. This includes verifying that the correct service codes and modifiers are assigned, the charges align with the agreed-upon fees, and all necessary supporting documentation is attached.
Verifying Claim Accuracy
To minimize denials and rejections, it is crucial to verify the accuracy of each claim before submission. This involves checking that the patient and insurance information is correct, all required fields are completed, and any necessary authorizations or referrals are included. Additionally, it is important to review the supporting documentation, such as medical records or test results, to ensure that the services billed align with the documentation provided.
Submitting Claims Electronically
Medical billing denial management software typically offers the ability to submit claims electronically. This method of submission is fast, efficient, and reduces the risk of errors or delays associated with manual processing. To submit claims electronically, ensure that the software is configured to communicate with the necessary clearinghouses or electronic data interchange (EDI) systems. The software will generate electronic claim files in the appropriate format, which can then be securely transmitted to the designated recipients for processing.
Printing and Mailing Paper Claims
In some cases, it may be necessary to print and mail paper claims. This could be due to specific insurance requirements or limitations, or the inability to submit claims electronically for certain payers. Within the medical billing denial management software, you can easily generate paper claim forms that include all the necessary information. Once printed, ensure that the claims are securely packaged and sent to the appropriate recipients for processing.
Managing Denials and Rejections
Identifying Denials and Rejections
Managing denials and rejections is a critical component of medical billing denial management software. The software will typically provide a dedicated module or section for tracking and managing these issues. Denials occur when an insurance company refuses to pay for a claimed service, while rejections refer to claims that are returned due to errors or missing information. The software will flag and categorize denials and rejections, allowing you to easily identify and address them.
Reviewing Rejection Reasons
Understanding the reasons for claim rejections is essential for preventing future occurrences and improving billing accuracy. Medical billing denial management software provides detailed information regarding rejection reasons, which may include missing or incorrect patient information, invalid service codes, or insufficient supporting documentation. By reviewing these rejection reasons, you can identify patterns or common errors and take appropriate measures to address them in future claim submissions.
Appealing Denied Claims
When a claim is denied by an insurance company, it is often possible to appeal the decision. The medical billing denial management software will typically include a function for initiating and managing appeals. This involves gathering any necessary additional documentation or supporting evidence, crafting a well-documented appeal letter, and tracking the progress of the appeal. By utilizing the appeal functionality within the software, you can increase the likelihood of successfully overturning denied claims and maximizing reimbursement.
Tracking Denial Trends
To continuously improve billing processes and minimize denials, it is important to track denial trends within the medical billing denial management software. The software will typically provide reporting or analytics capabilities that allow you to monitor and analyze denial data. This includes identifying the most common denial reasons, tracking denial rates over time, and pinpointing any patterns or trends that may be indicative of underlying issues. By tracking denial trends, you can proactively address recurring issues and implement appropriate measures to prevent future denials.
Resubmitting and Correcting Claims
Accessing Rejected Claim Information
When a claim is rejected, it is necessary to access the rejected claim information within the medical billing denial management software. This information will typically include the reasons for rejection, any error codes associated with the rejection, and details regarding what needs to be corrected or amended. By accessing this information, you can pinpoint the specific issues that caused the rejection and take appropriate action to correct the claim.
Correcting Billing Errors
Correcting billing errors is a crucial step in resubmitting rejected claims. The medical billing denial management software will typically allow you to edit and update claim information, such as patient and insurance details, service codes, charges, and supporting documentation. By diligently reviewing the rejection reasons and making the necessary corrections, you can ensure that the resubmitted claim is accurate and compliant with the payer’s requirements.
Updating Claim Information
In some cases, it may be necessary to update claim information that is not directly related to rejection reasons. For example, if a patient’s insurance coverage changes after a claim has been submitted, it may be necessary to update the claim with the new insurance details. Within the medical billing denial management software, you can easily access and update claim information as needed, ensuring that the claim is accurate and up to date with the most recent patient or insurance details.
Resubmitting Corrected Claims
After correcting and updating the necessary information, it is time to resubmit the corrected claims. Medical billing denial management software typically includes a function to resubmit claims electronically or generate new paper claim forms. Depending on the software’s capabilities, you may also have the option to include any additional documentation or supporting evidence to strengthen the claim. By promptly resubmitting corrected claims, you can minimize delays in reimbursement and improve overall revenue cycle management.
Tracking and Following Up on Claims
Monitoring Claim Status
Efficiently tracking the status of claims is crucial to ensure timely reimbursement and minimize delays in the revenue cycle. Within the medical billing denial management software, you can easily monitor the status of each claim, from submission to payment or resolution. The software will typically provide information regarding the claim’s current stage, any pending actions required, and the estimated time for resolution. By regularly monitoring claim status, you can proactively follow up on delayed or stalled claims and take appropriate action to expedite payment.
Creating Follow-up Reminders
To effectively manage and follow up on claims, it is important to create follow-up reminders within the medical billing denial management software. Reminders can be set to alert you when specific actions are required, such as following up with the insurance company, submitting additional documentation, or appealing denied claims. By utilizing the software’s reminder function, you can ensure that critical tasks are not overlooked and that necessary actions are taken in a timely manner.
Tracking Payment History
Accurately tracking payment history is essential for monitoring revenue and identifying any discrepancies or delayed payments. The medical billing denial management software typically includes a feature that allows you to record and track payment information related to each claim. This includes details such as the date of payment, the amount received, any adjustments or write-offs, and the payment method used. By regularly reviewing payment history, you can identify any payment issues, reconcile accounts, and ensure accurate financial reporting.
Analyzing Aging Reports
Aging reports provide valuable insights into the status of outstanding claims and the overall health of your revenue cycle. Medical billing denial management software typically includes predefined aging reports that categorize claims based on the length of time since submission or denial. By analyzing these reports, you can identify any patterns or trends in delayed payments, identify problematic payers, and take proactive measures to address any outstanding or aging claims. This allows you to improve claim follow-up strategies and optimize your revenue cycle management processes.
Generating Reports and Analytics
Running Standard Reports
Medical billing denial management software typically offers a variety of standard reports that provide key performance indicators and analytical insights. These reports may include metrics such as the total number of claims filed, the average reimbursement rate, the denial rate, and the average time to payment. By regularly running and reviewing these standard reports, you can gain a comprehensive understanding of your billing performance, identify areas for improvement, and make informed decisions regarding revenue cycle management.
Customizing Reports and Dashboards
To further tailor the reporting capabilities of the medical billing denial management software to your specific needs, many software packages allow for customization of reports and dashboards. This includes the ability to select specific data fields to be included in reports, create custom metrics or calculations, and design personalized dashboards that provide a visual snapshot of key performance indicators. By customizing reports and dashboards, you can focus on the information that is most relevant to your practice and gain actionable insights from your data.
Analyzing Key Performance Indicators
Analyzing key performance indicators (KPIs) is crucial for evaluating the effectiveness of your billing operations and identifying areas for improvement. Medical billing denial management software provides the necessary data and tools to calculate and analyze KPIs such as denial rates, first-pass resolution rates, and average reimbursement rates. By regularly analyzing these KPIs, you can benchmark your performance against industry standards, track progress over time, and implement targeted strategies to improve revenue cycle management.
Utilizing Analytics for Revenue Cycle Management
The availability of advanced analytics within medical billing denial management software allows for a deeper understanding of billing patterns, trends, and opportunities for improvement. By utilizing these analytics, you can identify areas of inefficiency or potential revenue leakage, develop strategies for boosting reimbursement rates, and optimize coding and billing processes. The insights gained from analytics can guide decision-making and ultimately improve revenue cycle management, resulting in increased profitability and financial stability for your practice.
Integration with Practice Management Systems
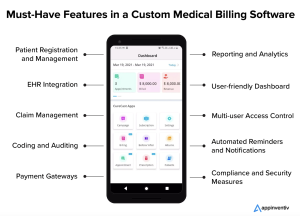
Importing Patient and Billing Data
Integration with practice management systems is a valuable feature of medical billing denial management software that streamlines data management and eliminates the need for duplicate data entry. The software can be configured to import patient and billing data from your practice management system, ensuring that patient profiles, service records, and claims information are automatically synchronized across the two systems. This integration minimizes data entry errors, improves efficiency, and allows for a more seamless workflow between different aspects of your practice.
Synchronizing Claim Status Updates
To prevent discrepancies and ensure accurate claim tracking, medical billing denial management software can synchronize claim status updates with your practice management system. This means that any changes in claim status, such as payment received or denial issued, will be reflected automatically in both systems. By synchronizing claim status updates, you can save time and avoid the need for manual updates, ensuring that you always have the most up-to-date information regarding the status of each claim.
Automatic Payment Posting
Automatic payment posting is another valuable integration feature of medical billing denial management software. With this functionality, payments received from insurance companies can be automatically posted to patient accounts within your practice management system. This eliminates the need for manual posting of payments, reduces the risk of errors, and streamlines the reconciliation process. By automating payment posting, you can improve accuracy and efficiency in managing your accounts receivable and ensure that revenue is accurately captured and allocated.
Sharing Data with EMR or EHR Systems
Integration between medical billing denial management software and electronic medical record (EMR) or electronic health record (EHR) systems allows for seamless sharing of patient and visit information. This ensures that accurate and up-to-date patient data is available for both clinical and billing purposes. Sharing data between these systems eliminates the need for duplicate data entry, reduces the risk of errors, and improves the quality and accuracy of billing information. By synchronizing data between the billing software and EMR or EHR systems, you can promote efficiency and ensure that the billing process is closely aligned with the clinical workflow.
Training and Support
User Training and Onboarding
When implementing medical billing denial management software, it is important to provide comprehensive user training and onboarding to ensure smooth adoption and optimal utilization of the software. Training sessions should cover all essential features and functionalities of the software, as well as best practices for efficient workflow management. By investing in user training and onboarding, you can equip your staff with the necessary skills and knowledge to navigate the software confidently, improve productivity, and maximize the benefits of the software.
Accessing Help Documentation and Resources
Medical billing denial management software typically provides extensive help documentation and resources to assist users in understanding and utilizing the software effectively. Help documentation often includes user guides, video tutorials, and FAQ sections that address common inquiries or issues. Familiarize yourself and your staff with these resources so that you can quickly access valuable information and troubleshoot any challenges that may arise during software usage.
Contacting Technical Support
In the event of technical issues or software-related questions, it is important to know how to contact the vendor’s technical support team. Medical billing denial management software vendors typically provide various support channels, such as email, phone, or live chat, to ensure that users can promptly and effectively address any issues that may arise. Keep the vendor’s contact information readily available and communicate any technical concerns to the support team for timely resolution.
Getting Software Updates and Upgrades
To ensure your medical billing denial management software remains up to date with the latest features, bug fixes, and regulatory changes, it is important to regularly check for software updates and upgrades. Software vendors often release updates periodically to address any issues or enhance software functionality. Stay informed about software updates and upgrades by subscribing to the vendor’s newsletters or notifications, and follow the provided instructions to install and implement the updates effectively. By keeping your software up to date, you can take advantage of new features, improve system performance, and ensure compliance with evolving industry standards.