In this article, you will be provided with a concise collection of real-life medical coding scenarios. These practical examples will demonstrate the vital role of accurate coding in the healthcare industry, showcasing how skilled medical coders translate complex diagnoses, procedures, and treatments into standardized codes. By exploring various scenarios, you will gain a deeper understanding of the challenges and intricacies involved in medical coding, as well as the importance of meticulous attention to detail in ensuring proper reimbursement and effective healthcare management.
Evaluation and Management Services

Hospital Visit
Hospital visits are an essential part of medical care, allowing healthcare professionals to assess and treat patients who require a higher level of care. Evaluation and management (E/M) services provided during hospital visits involve assessing the patient’s condition, reviewing their medical history, performing physical examinations, and formulating a treatment plan. These services are coded using E/M codes that reflect the complexity and intensity of the visit, taking into account factors such as the level of history obtained, the extent of the examination, and the complexity of medical decision-making.
Outpatient Visit
Outpatient visits refer to medical encounters where patients receive care without being admitted to a hospital. These visits can occur in various healthcare settings, such as clinics, physician offices, or specialized outpatient facilities. Evaluation and management (E/M) services provided during outpatient visits involve assessing the patient’s condition, addressing their concerns, examining relevant symptoms, and determining an appropriate treatment plan. The level of E/M service is determined by factors such as the complexity of the patient’s presenting problem, the extent of the examination performed, and the complexity of medical decision-making.
Nursing Facility Visit
Nursing facility visits involve providing medical care to patients residing in nursing homes or skilled nursing facilities. These visits are vital for managing the health of elderly or disabled individuals who may require specialized care and assistance. During nursing facility visits, healthcare professionals conduct comprehensive assessments, review medical records, communicate with facility staff, and address any concerns or acute medical issues. The coding of E/M services for nursing facility visits is based on the complexity of the patient’s condition, the level of medical decision-making required, and the extent of history and examination performed.
Emergency Department Visit
Emergency department visits deal with urgent and often life-threatening medical conditions requiring immediate medical attention. These visits are characterized by the need for quick assessment, rapid decision-making, and prompt intervention to stabilize the patient’s condition. Evaluation and management (E/M) services during emergency department visits involve thorough evaluations, diagnostic testing, treatment administration, and care coordination. The coding for emergency department visits is determined by the severity of the patient’s presenting problem, the level of medical decision-making, and the resources utilized during the encounter.
Surgical Procedures

Appendectomy
An appendectomy is a surgical procedure performed to remove an inflamed or infected appendix. It is commonly indicated in cases of appendicitis, which can cause severe abdominal pain and discomfort. During an appendectomy, the surgeon makes an incision in the abdomen, removes the appendix, and closes the incision. Coding for an appendectomy involves utilizing specific Current Procedural Terminology (CPT) codes that accurately describe the complexity and extent of the procedure.
Hernia Repair
Hernia repair surgery involves the correction of a hernia, which is a condition characterized by the protrusion of an organ or tissue through a weak spot in the surrounding muscles or connective tissue. The surgery typically involves returning the displaced organ or tissue to its proper place and strengthening the weakened area with sutures or mesh. Coding for hernia repair procedures involves identifying the specific type of hernia, the surgical approach used, and any additional procedures performed during the surgery.
Gallbladder Removal
Gallbladder removal, also known as cholecystectomy, is a surgical procedure performed to remove the gallbladder, usually due to the presence of gallstones or other gallbladder-related conditions. The procedure can be performed using traditional open surgery or minimally invasive laparoscopic techniques. Coding for gallbladder removal procedures involves selecting the appropriate CPT code based on the surgical approach used, any additional procedures performed, and the complexity of the case.
Knee Replacement
Knee replacement surgery, also called knee arthroplasty, is a surgical procedure performed to replace a damaged or diseased knee joint with an artificial joint, known as a prosthesis. This procedure is commonly indicated in cases of severe knee pain and limited mobility caused by conditions like osteoarthritis or rheumatoid arthritis. Coding for knee replacement procedures requires identifying the specific type of knee replacement performed, whether it is a partial or total replacement, and any additional procedures or implants used during the surgery.
Diagnostic Testing

Radiology
Radiology diagnostic testing involves the use of various imaging techniques to visualize internal body structures and identify any abnormalities or conditions. Examples of radiology tests include X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), and ultrasound. Proper coding for radiology tests involves selecting the appropriate CPT codes that accurately describe the type of imaging study performed, the specific body part imaged, and any contrast material used.
Laboratory Testing
Laboratory testing plays a crucial role in diagnosing and monitoring a wide range of medical conditions. These tests involve analyzing blood, urine, tissue samples, and other bodily fluids to measure specific markers, detect infections, or assess organ function. Coding for laboratory tests relies on using specific Current Procedural Terminology (CPT) codes that accurately describe the type of test performed, the specific analytes measured, and the methodologies employed.
Electrocardiogram (ECG)
Electrocardiogram (ECG) testing is a non-invasive procedure that records the electrical activity of the heart. It helps diagnose various heart conditions, such as arrhythmias, myocardial infarction, or conduction abnormalities. Coding for ECG testing involves selecting the appropriate CPT code that reflects the complexity of the procedure performed, whether it is a routine single-lead ECG, a multi-lead ECG, or an extended monitoring service.
Endoscopy
Endoscopy procedures involve the use of a flexible tube with a camera and a light source to visualize and examine the internal organs or structures of the body. Endoscopy can be performed for diagnostic purposes, such as identifying gastrointestinal abnormalities or obtaining tissue samples for biopsy, or for therapeutic interventions like removing polyps or placing stents. Coding for endoscopy procedures requires identifying the specific type of endoscopy performed, the location of the procedure, and any additional interventions or biopsies conducted.
Medical Documentation

History and Physical Examination
The medical documentation of a patient encounter is an essential aspect of providing quality healthcare. This documentation includes a detailed history of the patient’s present illness, past medical history, family and social history, as well as a comprehensive physical examination. Accurate and thorough documentation enables healthcare professionals to assess the patient’s condition, make informed diagnoses, and develop appropriate treatment plans. Coding for history and physical examination documentation is typically not based on specific codes but rather on the levels of complexity and detail included in the documentation.
Progress Notes
Progress notes document the ongoing care and management of a patient over time. These notes include information such as the patient’s progress, response to treatments, any complications or side effects experienced, and any changes in the treatment plan. Proper coding of progress notes involves accurately reflecting the level of complexity and detail included in the notes, ensuring that the documentation supports the medical necessity of the services provided.
Operative Notes
Operative notes are comprehensive documents that detail the specifics of a surgical procedure. These notes provide a detailed account of the surgery, including the pre-operative diagnosis, the procedure performed, any complications encountered, and the post-operative condition of the patient. coding for operative notes involves selecting the appropriate CPT codes that accurately describe the surgical procedure performed, any additional procedures or interventions, and any relevant modifiers that indicate the complexity or unique circumstances of the surgery.
Discharge Summary
A discharge summary is a critical document that summarizes the patient’s hospital stay, including the reason for admission, the treatments received, any procedures performed, and the patient’s condition at the time of discharge. It also includes instructions for ongoing care, follow-up appointments, and medication management. Proper coding of discharge summaries involves accurately reflecting the comprehensive nature of the document and ensuring that all relevant information is included for effective continuity of care.
Chronic Disease Management

Diabetes
Chronic disease management is a crucial component of healthcare, as it involves the ongoing care and treatment of patients with conditions that require consistent monitoring and intervention. Managing chronic diseases like diabetes involves regular follow-up visits, routine laboratory testing, medication management, and lifestyle modifications. Coding for chronic disease management services in diabetes focuses on accurately reflecting the level of complexity, the frequency and duration of the encounters, and any additional interventions performed.
Hypertension
Hypertension, or high blood pressure, is a common chronic condition that requires long-term management to prevent complications such as heart disease, stroke, or kidney disease. Managing hypertension involves regular monitoring of blood pressure, lifestyle modifications, and medication management. Coding for chronic disease management services in hypertension considers the frequency of visits, the complexity of medical decision-making, and the duration of encounter.
Asthma
Asthma is a chronic respiratory condition that requires ongoing monitoring and management to control symptoms and prevent exacerbations. The management of asthma involves regular follow-up visits, assessment of symptoms, pulmonary function testing, medication adjustments, and patient education. Coding for chronic disease management services in asthma entails accurately reflecting the level of control, the frequency and duration of visits, and any additional interventions provided.
Chronic Kidney Disease
Chronic kidney disease (CKD) necessitates ongoing monitoring and management to slow disease progression and prevent complications. Managing CKD involves regular follow-up visits, laboratory testing, medication adjustments, and lifestyle modifications. Coding for chronic kidney disease management services focuses on accurately reflecting the stage of CKD, the frequency and duration of encounters, and any additional services or interventions provided.
Medical Billing
Medical cost concept with stethoscope and medical bill
Insurance Claims
Medical billing plays a crucial role in the financial sustainability of healthcare practices as it involves submitting claims to insurance companies for reimbursement of provided services. Proper coding and documentation are vital to ensure accurate claim submission, including selecting the appropriate diagnosis and procedure codes, verifying insurance coverage, and adhering to the rules and guidelines set by insurance payers.
Payment Posting
Payment posting refers to the process of recording and reconciling payments received from insurance payers, patients, or other sources. Accurate payment posting ensures that the appropriate credits and adjustments are applied, allowing for accurate accounts receivable management and financial reporting.
Denial Management
Denial management is an integral part of medical billing, involving the identification, analysis, and resolution of claim denials or rejections from insurance payers. This process requires detailed review and investigation of denial reasons, appeals preparation, and resubmission of denied claims to maximize reimbursement.
Appeals and Rejections
Appeals and rejections are common challenges encountered in the medical billing process. Effective appeals management entails understanding the denial reason, gathering supporting documentation, and effectively communicating with insurance payers to overturn denied claims. Proper coding, accurate documentation, and timely submission of appeals are crucial to successfully resolving claim denials and optimizing reimbursement.
Coding for Specialties
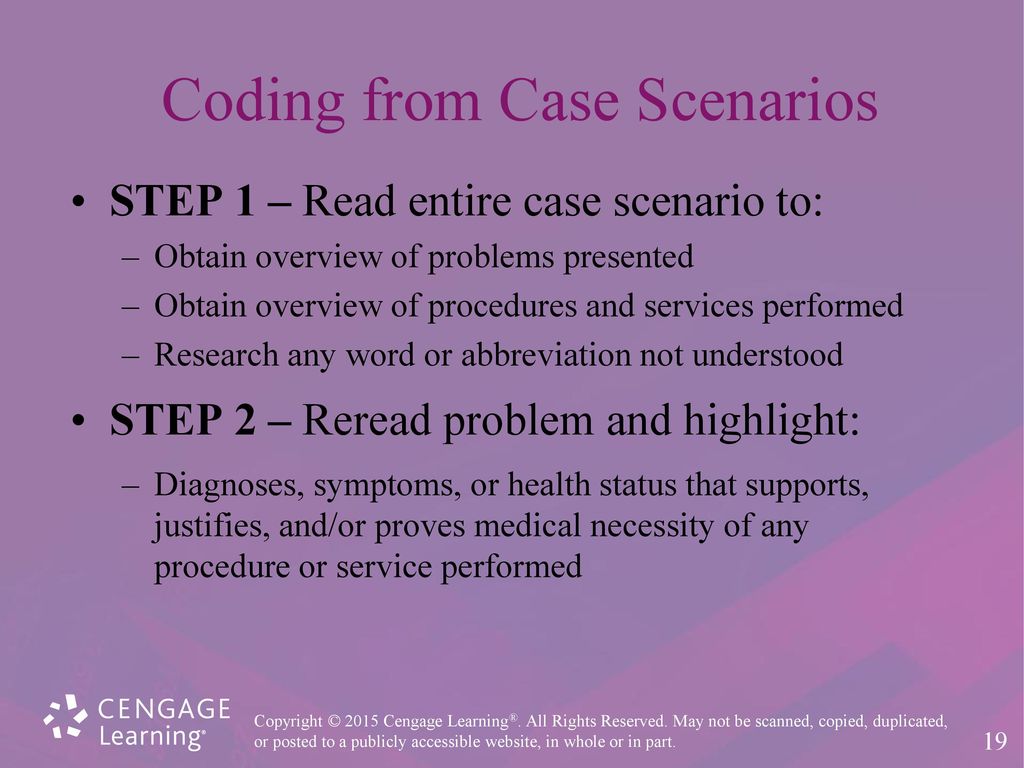
This image is property of slideplayer.com.
Anesthesia
Anesthesia coding requires a specialized understanding of the unique services provided in the perioperative setting. Proper coding for anesthesia services involves selecting the appropriate anesthesia codes based on factors such as the type and complexity of the procedure, the patient’s age, and any underlying medical conditions that may impact anesthesia management.
Cardiology
Cardiology coding involves a wide range of services, including diagnostic testing, interventional procedures, and ongoing management of cardiovascular conditions. Accurate coding for cardiology services requires familiarity with specific CPT codes for procedures like cardiac catheterization, echocardiography, and electrophysiology studies, as well as the appropriate use of modifiers for multiple procedures, professional component billing, or critical care services.
Orthopedics
Orthopedic coding encompasses a variety of procedures related to the musculoskeletal system, such as joint replacements, fracture repairs, and arthroscopic surgeries. Proper coding for orthopedic procedures involves understanding the specific details of the procedure performed, including the type of operation, the anatomical site involved, and any additional procedures or implants used.
Dermatology
Dermatology coding encompasses a wide range of services related to the assessment, diagnosis, and treatment of skin conditions. This includes procedures such as skin biopsies, excisions of lesions, and removal of benign or malignant skin tumors. Accurate coding for dermatology procedures requires knowledge of specific CPT codes, understanding of anatomical site documentation, and familiarity with modifiers for lesion size, layered closure, or biopsy techniques.
Telemedicine

Remote Consultation
Telemedicine has become increasingly popular as a means of providing medical care remotely, particularly in situations where in-person visits may be challenging or impossible. Remote consultations involve virtual interactions between healthcare providers and patients using audio and video communication technologies. Proper coding for remote consultations involves using specific telemedicine codes or appropriate evaluation and management (E/M) codes for new or established patients, depending on the complexity and nature of the consultation.
Virtual Visits
Virtual visits are similar to remote consultations, enabling patients to receive healthcare services from the comfort of their own homes. These visits may include discussions of symptoms, medication management, follow-up care, and counseling. Coding for virtual visits involves selecting the appropriate telehealth or E/M codes that accurately reflect the level of complexity and duration of the encounter.
Telemonitoring
Telemonitoring is a remote monitoring service that allows healthcare providers to track patients’ health data, such as vital signs, glucose levels, or cardiac rhythms, through wearable devices or home monitoring equipment. Coding for telemonitoring services involves specific CPT codes that reflect the type of monitoring performed and the duration of the service provided.
Mobile Health Applications
Mobile health applications, or apps, have revolutionized healthcare by providing patients with access to educational resources, health tracking tools, and interactive platforms to communicate with healthcare providers. Coding for mobile health applications focuses on the specific functionalities offered by the app, such as patient education, symptom tracking, or remote communication, and can involve a combination of telehealth or E/M codes that align with the services provided.
Procedural Coding

CPT Codes
Current Procedural Terminology (CPT) codes are the standard codes used to describe medical, surgical, and diagnostic procedures performed by healthcare providers. These codes are essential for accurate reimbursement and tracking of services provided. Proper coding with CPT codes requires knowledge of the specific codes for each procedure, accurate documentation of the details of the procedure, and adherence to the guidelines and modifiers associated with each code.
Modifiers
Modifiers are additional codes appended to a main CPT code to provide further information about the specific circumstances or complexity of a procedure. Modifiers can influence reimbursement levels, indicate services performed in conjunction with the main procedure, or highlight unique circumstances that impact the coding or payment. Proper use of modifiers requires an understanding of each modifier’s purpose and the documentation requirements associated with its use.
Global Surgery Package
The global surgery package represents a comprehensive bundle of services provided during the pre-operative, intra-operative, and post-operative periods for a specific surgical procedure. It includes pre-operative evaluation, the procedure itself, and post-operative care typically rendered by the surgeon. Accurate coding for the global surgery package involves selecting the appropriate CPT codes that reflect the specific elements included in the global package.
Unbundling
Unbundling refers to the practice of coding and billing individual components of a bundled procedure separately, instead of utilizing the appropriate bundled code. Unbundling is considered fraudulent and can result in denial of claims or even legal consequences. Proper coding practices involve accurately identifying and applying the correct bundled code to ensure proper reimbursement and compliance with coding regulations.
ICD-10 Coding
Infectious Diseases
ICD-10 coding involves the use of specific codes to document and classify infectious diseases accurately. These codes are essential for outbreak monitoring, infection control, and epidemiological studies. Proper coding for infectious diseases requires knowledge of the specific disease processes, the causative agents, and the anatomical sites involved to select the appropriate ICD-10 codes.
Neoplasms
Neoplasm coding in the ICD-10 system allows for accurate documentation and classification of tumors and cancerous growths. The codes account for tumor location, behavior (benign or malignant), histology, and other important factors. Proper coding for neoplasms requires familiarity with the specific ICD-10 codes for different types of tumors, an understanding of the staging and grading of cancers, and accurate documentation of relevant tumor characteristics.
Mental Health Disorders
ICD-10 includes a comprehensive classification system for mental health disorders, providing codes for various conditions such as depression, anxiety disorders, schizophrenia, and substance use disorders. Accurate coding for mental health disorders involves understanding the specific diagnostic criteria outlined by the ICD-10, documenting the patient’s symptoms and behaviors, and selecting the appropriate codes that reflect the specific condition diagnosed.
Obstetrics and Gynecology
ICD-10 coding is crucial in the field of obstetrics and gynecology to accurately document and classify conditions related to pregnancy, childbirth, and the female reproductive system. Proper coding for obstetric and gynecological conditions involves selecting the appropriate ICD-10 codes that reflect the specific diagnoses, complications, procedures, or outcomes of interest.
In conclusion, medical coding encompasses a vast array of specialties and services, each requiring a deep understanding of specific coding guidelines and principles. Accurate and comprehensive coding is essential for proper reimbursement, effective communication, and reliable healthcare data. Healthcare professionals involved in the coding process must stay updated with the latest coding changes, guidelines, and documentation requirements to ensure accurate coding and billing practices.
