Clinical coding is a complex and intricate discipline that plays a crucial role in the healthcare industry. It involves the translation of medical diagnoses, procedures, and services into universally recognized codes for various purposes such as reimbursement, research, and data collection. While the accuracy of clinical coding is paramount, it is not uncommon for individuals to question whether it is a challenging field to enter. In this article, we will shed light on the level of difficulty associated with clinical coding, addressing common misconceptions and providing insights into the skills required to excel in this profession. Prepare to gain a clear understanding of the challenges and rewards that lie within the realm of clinical coding.
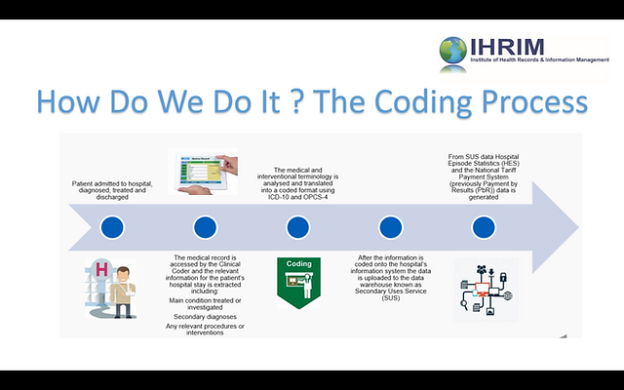
What is Clinical Coding?

This image is property of www.allenschool.edu.
Definition
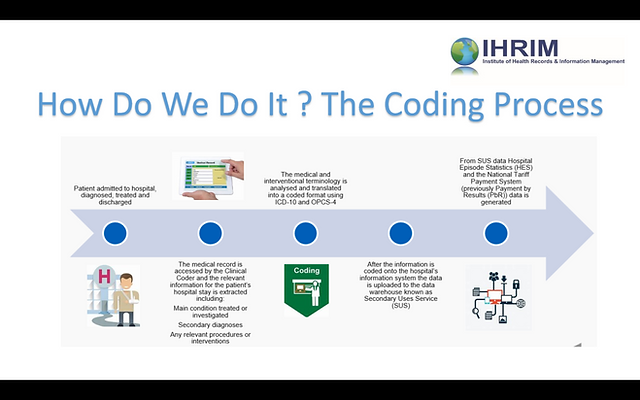
Clinical coding is the process of translating medical information into a standardized format. It involves assigning specific codes to diseases, treatments, procedures, and other medical data. These codes are used for documentation, billing, and research purposes. By using a common coding system, healthcare professionals can ensure consistency and accuracy in medical records and improve communication across different healthcare settings.
Purpose
The primary purpose of clinical coding is to accurately represent the patient’s healthcare encounters in a standardized format for reimbursement, research, and statistical analysis. Clinical coding plays a crucial role in streamlining healthcare processes, enabling efficient data exchange, and ensuring accurate billing and insurance claims. It also provides valuable information for public health surveillance and research studies.
Importance
Clinical coding is essential for the healthcare industry as it ensures the use of a common language to describe and classify medical conditions and procedures. Accurate coding helps healthcare providers maintain appropriate documentation, enables effective communication with insurance companies, and facilitates accurate reimbursement for services. Additionally, clinical coding impacts public health by contributing to reporting systems, research studies, and epidemiological analyses.
Skills Required for Clinical Coding

Medical Knowledge
To excel in clinical coding, a solid understanding of medical terminology, anatomy, physiology, and disease processes is crucial. Coders must be familiar with the diagnostic criteria for various diseases and have the ability to interpret medical reports, charts, and documentation accurately. They need to stay updated with advancements in medical practices and be able to translate complex medical information into standardized codes.
Analytical Skills
Clinical coding involves analyzing medical records, identifying relevant information, and determining the appropriate codes. Coders must possess strong analytical skills to interpret complex documentation, identify inconsistencies or missing information, and make decisions based on coding guidelines and principles. They need to have a meticulous approach to ensure accuracy and avoid potential errors.
Attention to Detail
Attention to detail is a fundamental skill for clinical coding. Coders must have a keen eye for capturing and documenting all relevant medical information accurately. A single error in coding can lead to significant consequences, such as incorrect billing, denial of insurance claims, or misinterpretation of patient data. Attention to detail helps coders maintain data integrity and ensure the quality of healthcare records.
Organizational Skills
As clinical coding involves working with a large amount of patient data, strong organizational skills are essential. Coders must efficiently manage medical records, keep track of deadlines, prioritize tasks, and maintain a systematic approach to their work. Being organized enables coders to handle a high volume of coding assignments, reduce errors, and meet the demands of their role with efficiency.
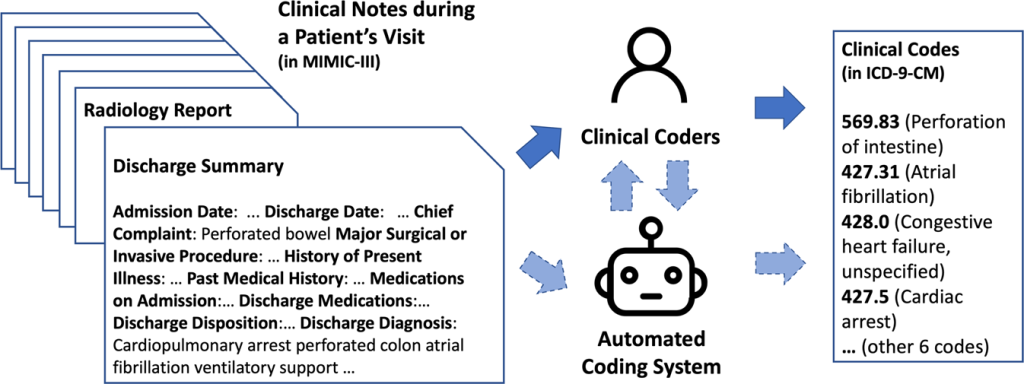
Coding and Classification Systems Knowledge
A comprehensive understanding of coding and classification systems, such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT), is vital for clinical coders. These systems provide the framework and guidelines necessary for assigning the appropriate codes to medical diagnoses, procedures, and services. Proficiency in using coding software and familiarity with coding guidelines help coders accurately translate medical information into the required codes.
Challenges in Clinical Coding
Complexity of Medical Terminology
Medical terminology can be intricate and highly specialized. Clinical coders must possess a deep understanding of medical language, abbreviations, and acronyms. They need to be able to decipher medical reports and understand the nuances of diagnoses, treatments, and procedures described in the documentation.
Evolving Coding Guidelines
Coding guidelines and regulations are constantly evolving. Clinical coders must stay updated with the latest changes in coding systems and guidelines to ensure accurate coding and compliance with industry standards. Continuous learning is necessary to adapt to new coding concepts, conventions, and updates in order to maintain coding accuracy and effectiveness.
Time Constraints
Clinical coding often involves strict deadlines due to billing and reimbursement requirements. Coders may face time constraints while analyzing medical records, assigning codes, and meeting established turnaround times. The pressure to work efficiently while maintaining accuracy can be challenging, especially when dealing with complex cases or high volumes of coding assignments.
Ongoing Learning and Updating
As medical practices and coding systems evolve, clinical coders need to engage in continuous learning and professional development. Staying current with medical advancements, coding changes, and industry trends is crucial for maintaining accuracy and compliance. This ongoing learning process requires dedication, persistence, and a commitment to keeping up with the ever-changing landscape of clinical coding.
Increased Responsibility
Clinical coders play a critical role in ensuring accurate coding, which directly affects patient care, reimbursement, and healthcare data analysis. The responsibility of accurately coding medical information falls on the clinical coder, and any errors or oversights can have significant consequences. Coders must exhibit high levels of accountability, professionalism, and ethical conduct to maintain the integrity and quality of healthcare data.
Training and Education in Clinical Coding

Formal Education Programs
Many clinical coders start their careers by pursuing formal education programs in medical coding, health information management, or related fields. These programs provide a foundation in medical terminology, anatomy, physiology, disease processes, coding principles, and coding systems. Graduates of these programs may earn associate or bachelor’s degrees, preparing them for entry-level positions in the field.
Certifications and Credentials
Certifications and credentials play a vital role in the professional development of clinical coders. Organizations such as the American Health Information Management Association (AHIMA) and the American Academy of Professional Coders (AAPC) offer certification programs, including the Certified Coding Associate (CCA) and Certified Professional Coder (CPC) credentials. These certifications demonstrate expertise in medical coding and can enhance career opportunities and earning potential.
Continuing Education
Continuing education is essential for clinical coders to stay updated with evolving coding systems, guidelines, and industry practices. Various organizations and professional associations provide continuing education programs, workshops, and seminars to support ongoing learning. Continuing education helps coders maintain their skills, expand their knowledge base, and stay current with regulatory changes and industry advancements.
Career Opportunities in Clinical Coding

This image is property of www.northwestcareercollege.edu.
Hospitals and Healthcare Facilities
Hospitals and healthcare facilities employ clinical coders to ensure accurate and timely coding of patients’ medical records. Coders in these settings work closely with healthcare professionals to document diagnoses, procedures, and treatments, enabling proper billing, reimbursement, and data analysis. They play a crucial role in maintaining accurate medical records and optimizing healthcare processes.
Insurance Companies
Insurance companies rely on clinical coders to interpret and assign codes that accurately reflect the services provided and the diagnoses made. Coders in insurance companies review medical claims, assess their accuracy, and ensure that they comply with coding guidelines and standards. They play a critical role in determining the appropriateness of reimbursement and ensuring that claims are processed correctly.
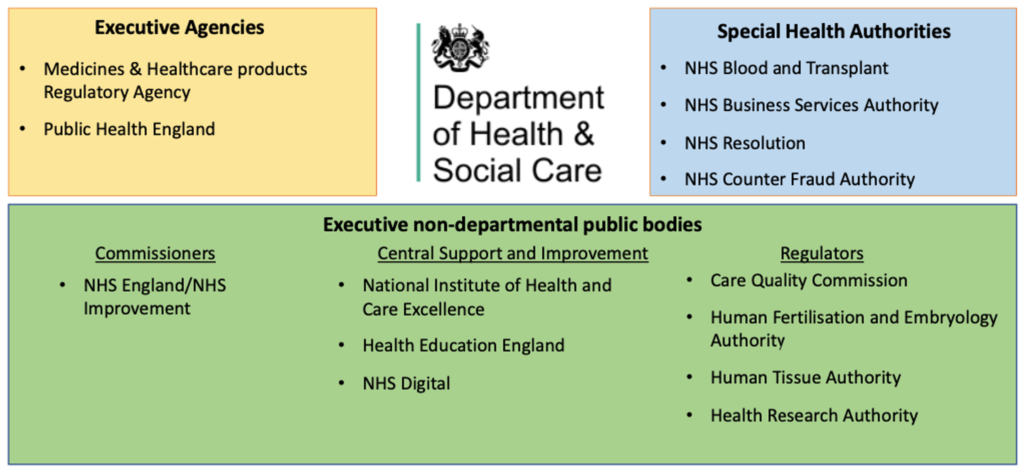
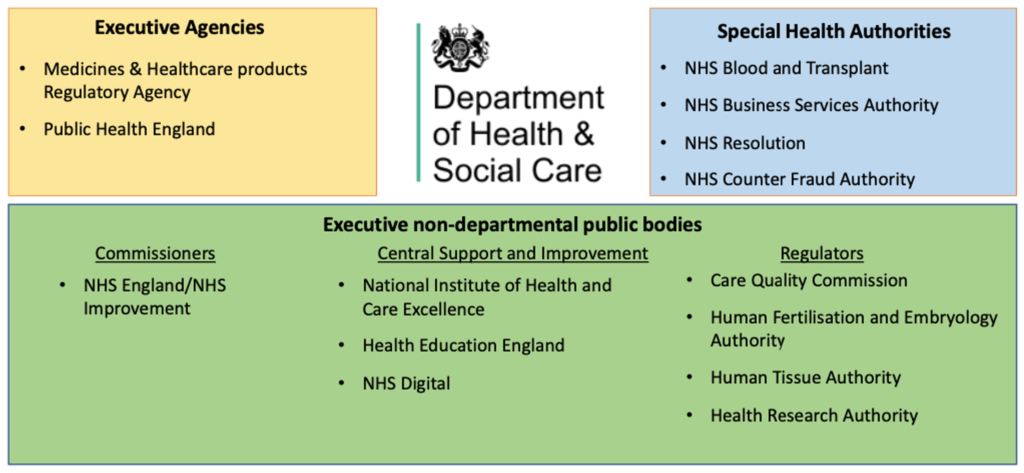
Government Agencies
Government agencies, such as the Centers for Medicare and Medicaid Services (CMS), hire clinical coders to support healthcare programs, policy development, and data analysis. Clinical coders working in government agencies contribute to public health initiatives, research studies, and quality improvement projects. They play a vital role in translating medical data into meaningful information for health surveillance, epidemiological analysis, and policymaking.
Clinical Coding Consultancy
Clinical coding consultancies provide specialized coding services and expertise to healthcare organizations. These consultancies often work with multiple clients, assisting them in accurate coding, compliance, and revenue cycle management. Clinical coders in consultancies may engage in coding audits, coding education, and providing guidance on coding-related issues. This career path offers the opportunity to work on diverse coding projects and collaborate with different healthcare entities.
Demand and Job Outlook for Clinical Coders

Growing Demand
The demand for skilled clinical coders is expected to grow in the coming years. As healthcare systems expand, the need for accurate and efficient coding to support billing, reimbursement, and data analysis will increase. Additionally, changing coding regulations, advancements in medical technology, and the focus on electronic health records contribute to the growing demand for coding expertise.
Job Stability
Clinical coding offers job stability due to its integral role in healthcare operations. As long as healthcare services are provided, clinical coders will be required to translate medical information into standardized codes. The ongoing need for accurate coding ensures a stable job market and potential for long-term career growth.
Salary Potential
Clinical coders can enjoy competitive salaries based on their experience, credentials, and skill set. According to the U.S. Bureau of Labor Statistics, the median annual wage for medical records and health information technicians, which includes clinical coders, was $44,090 in May 2020. With additional experience and specialized knowledge, clinical coders may have the opportunity to earn higher salaries and advance their careers.
Tips for Success in Clinical Coding

Continuous Learning
Continuous learning is key to success in clinical coding. Stay updated with coding guidelines, regulatory changes, and industry trends by attending conferences, workshops, and continuing education programs. Engage in self-study, online resources, and networking to expand your knowledge and enhance your coding skills.
Attention to Detail
Develop a keen eye for detail to ensure accurate coding. Pay close attention to medical documentation, cross-reference codes, and review coding guidelines to minimize errors. Double-check your work and aim for precision in assigning codes, as even a small mistake can have significant ramifications.
Effective Communication
Effective communication is essential in clinical coding. Collaborate with healthcare professionals, billing staff, and insurance representatives to address any coding-related issues or queries. Clear and concise communication ensures accurate coding and helps resolve any discrepancies or concerns promptly.
Time Management
Efficient time management is crucial in clinical coding. Prioritize tasks, set realistic goals, and manage your time effectively to meet deadlines. Plan your work and allocate sufficient time for complex cases, while also maintaining productivity for high-volume coding assignments.
Networking
Build a professional network within the coding community to stay informed and connected. Engage with fellow coders, attend industry events, and join professional organizations to learn from others, share experiences, and gain insights into best practices. Networking can help you stay up-to-date with the latest developments and open doors to new career opportunities.
Conclusion
Clinical coding is a critical process that ensures accurate representation of medical information through standardized codes. It requires a combination of medical knowledge, analytical skills, attention to detail, organizational skills, and coding system expertise. Despite the challenges, clinical coding offers a rewarding career path with job stability, competitive salaries, and opportunities for professional growth. By continuously learning, paying attention to detail, effectively communicating, managing time, and networking, you can achieve success and contribute to the efficiency and accuracy of healthcare documentation and data analysis.
This image is property of d33wubrfki0l68.cloudfront.net.