Remote medical coders play a pivotal role in the healthcare industry by accurately translating medical diagnoses and procedures into a standardized coding system. These highly skilled professionals possess an in-depth understanding of medical terminology, anatomy, and coding guidelines, enabling them to assign the appropriate codes to patient records. By meticulously reviewing medical documentation, remote medical coders ensure that healthcare providers are properly reimbursed for their services while adhering to strict privacy and compliance regulations. Their expertise not only facilitates accurate billing and reimbursement processes but also contributes to improved patient care and streamlined healthcare operations.
What Does a Remote Medical Coder Do?
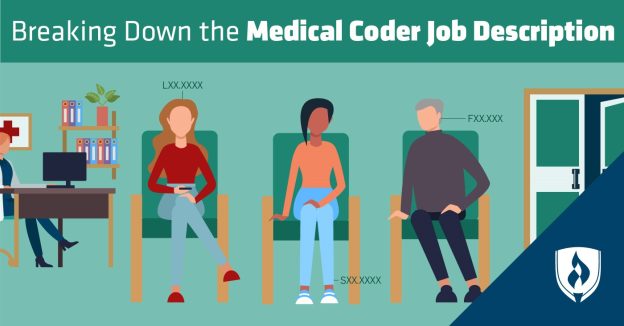
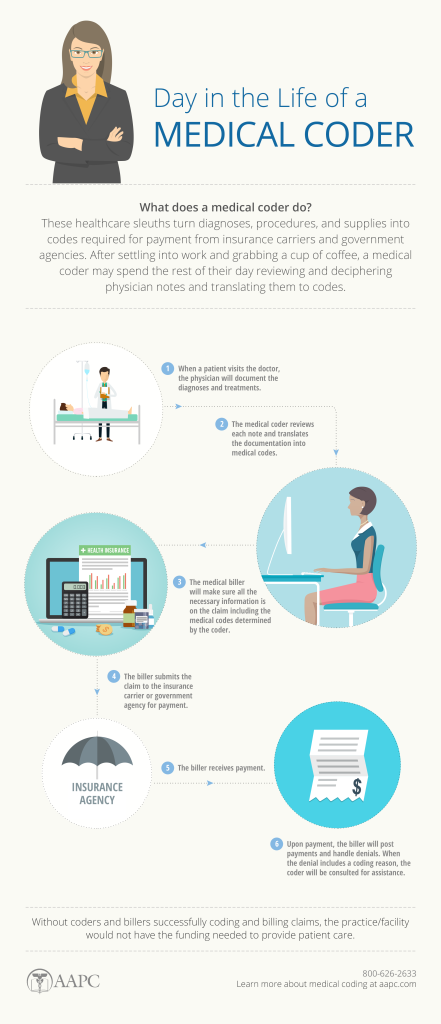
A remote medical coder is a professional responsible for reviewing and analyzing medical records to assign appropriate diagnosis and procedure codes. They play a crucial role in the healthcare industry by ensuring accurate documentation and compliance with coding guidelines. remote medical coders communicate with healthcare providers to clarify documentation and ensure that the coding accurately reflects the services provided to patients.
Responsibilities of a Remote Medical Coder
Remote medical coders have several responsibilities that contribute to the efficiency and accuracy of healthcare coding. These responsibilities include:
Reviewing and analyzing medical records:
Remote medical coders carefully review medical records, including physician notes, laboratory results, and radiology reports. This comprehensive review allows them to identify and extract relevant information necessary for accurate coding.
Assigning appropriate diagnosis and procedure codes:
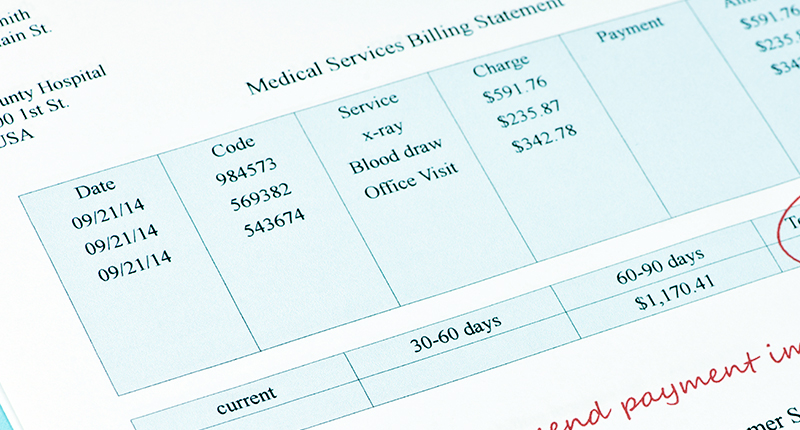
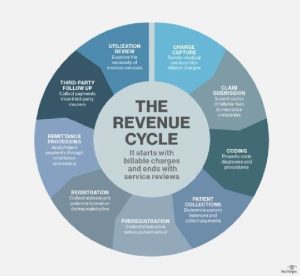
Based on the information extracted from medical records, remote medical coders assign appropriate diagnosis and procedure codes. These codes are a standardized way of categorizing medical services and are crucial for accurate billing and reimbursement.
Ensuring accuracy and compliance with coding guidelines:
Remote medical coders must ensure that the assigned codes accurately reflect the services provided, adhere to coding guidelines, and comply with regulatory requirements. Accuracy is vital to prevent fraudulent practices and ensure proper reimbursement.
Communicating with healthcare providers to clarify documentation:
Remote medical coders often need to communicate with healthcare providers to clarify documentation discrepancies or obtain additional information. Effective communication ensures that coding reflects the actual services provided and minimizes claim denials or delays.
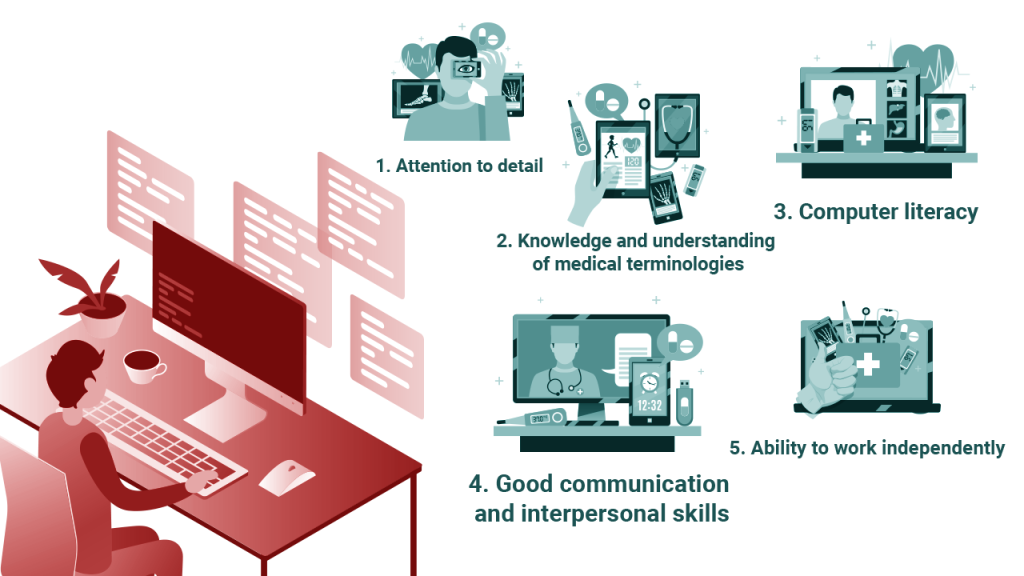
Skills Required for Remote Medical Coders
To excel as a remote medical coder, certain skills are essential. These skills include:
Knowledge of medical terminology, anatomy, and physiology:
Remote medical coders must possess a strong foundation in medical terminology, anatomy, and physiology. This knowledge allows them to understand and accurately code complex medical procedures and diagnoses.
Proficiency in medical coding systems:
Proficiency in medical coding systems, such as ICD-10, CPT, and HCPCS, is crucial for remote medical coders. They must be familiar with these coding systems to assign the appropriate codes that accurately represent the healthcare services provided.
Attention to detail and analytical skills:
Remote medical coders need a keen eye for detail to ensure accurate coding. They must be able to analyze medical records meticulously to identify relevant information for coding purposes.
Ability to adhere to strict confidentiality and ethical standards:
Remote medical coders handle sensitive patient information, so they must maintain strict confidentiality and adhere to ethical standards. It is important to protect patients’ privacy and ensure compliance with regulations such as HIPAA.
Effective communication and teamwork:
Remote medical coders often work as part of a larger healthcare team. Effective communication skills are necessary for collaborating with physicians, nurses, and other healthcare professionals to clarify documentation or resolve coding-related issues.
Computer literacy and proficiency in coding software:
Remote medical coders need to be computer literate and possess proficiency in coding software. They utilize electronic health record (EHR) systems and coding software like EncoderPro and Flash Code to streamline their coding processes.
Benefits of Remote Medical Coding
Remote medical coding offers several benefits to professionals in the field. These benefits include:
Flexibility to work remotely:
One of the significant advantages of remote medical coding is the ability to work from anywhere. Remote coders have the freedom to choose their work environment, which can lead to increased job satisfaction and work-life balance.
Work-life balance:
Remote medical coding allows for greater work-life balance by eliminating the need for commuting and providing more control over work hours. This flexibility allows remote coders to manage personal responsibilities while still meeting professional obligations.
Reduced commuting time and costs:
Working remotely eliminates the need for long commutes, saving time and money on transportation expenses. Remote medical coders can use the time saved to focus on their work or engage in other activities that enhance their personal lives.
Expanded job opportunities and access to clients nationwide:
Remote medical coding opens up a broader range of job opportunities as coders can work with healthcare providers and institutions nationwide. This flexibility enables remote coders to work with diverse healthcare organizations and gain exposure to different coding practices.
Potential for higher earning potential:
Remote medical coders may have the potential for higher earning potential compared to their counterparts working in traditional healthcare settings. The flexibility of remote work allows for increased productivity, which can result in higher billing and coding accuracy rates.
Educational Requirements for Remote Medical Coders
To become a remote medical coder, certain educational requirements must be met. These requirements include:
High school diploma or equivalent:
A high school diploma or an equivalent qualification is the minimum educational requirement for aspiring remote medical coders. This provides a foundation for further training and education in medical coding.
Post-secondary training in medical coding:
While not mandatory, most remote medical coders pursue post-secondary training in medical coding through certificate programs or associate degree programs. These programs provide in-depth knowledge and hands-on training in medical coding principles, coding systems, and healthcare regulations.
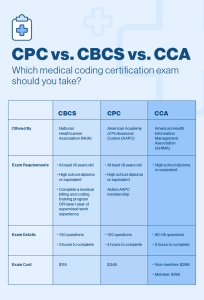
Certifications for Remote Medical Coders
Certifications play a vital role in demonstrating proficiency and knowledge in the field of remote medical coding. Some widely recognized certifications for remote medical coders include:
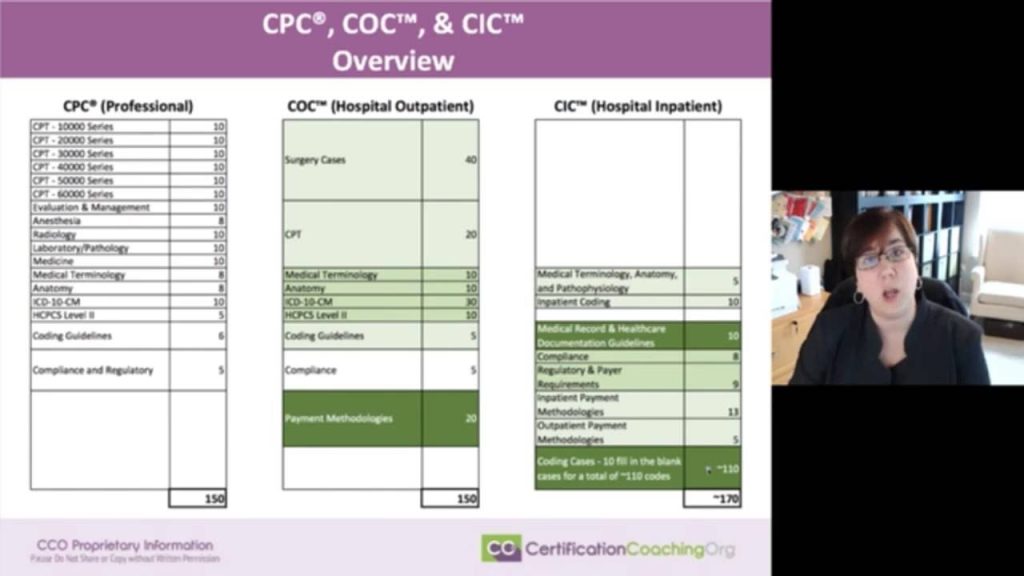
Certified Professional Coder (CPC):
Offered by the American Academy of Professional Coders (AAPC), The CPC certification validates the ability to assign accurate codes for diagnoses, procedures, and services. It demonstrates expertise in the correct application of CPT, ICD-10, and HCPCS Level II coding guidelines.
Certified Coding Specialist (CCS):
The CCS certification, offered by the American Health Information Management Association (AHIMA), is a credential for experienced coders. It showcases proficiency in inpatient and outpatient coding, as well as a thorough understanding of coding guidelines and regulations.
Certified Professional Biller (CPB):
The CPB certification, also offered by the AAPC, focuses on the billing aspect of medical coding. It demonstrates expertise in medical billing, including filing claims, resolving claim denials, and optimizing reimbursement strategies.
Certified Outpatient Coder (COC):
The COC certification, offered by the AAPC, specifically validates the ability to accurately code outpatient records, including ambulatory surgical centers and hospital outpatient services.
Certified Inpatient Coder (CIC):
The CIC certification, also offered by the AAPC, focuses on inpatient coding. It demonstrates proficiency in coding complex inpatient records, including diagnoses, procedures, and complications.
Certified Risk Adjustment Coder (CRC):
The CRC certification, offered by the AAPC, focuses on risk adjustment coding. It validates expertise in coding for payment models such as hierarchical condition categories (HCC), where accurate coding affects reimbursement rates.
Tools and Software Used by Remote Medical Coders
Remote medical coders utilize various tools and software to optimize their coding processes. These tools include:
Electronic Health Record (EHR) systems:
Remote medical coders rely on EHR systems to access and review patient medical records. These systems provide a centralized platform for healthcare professionals to document and track patient information, making it accessible to remote coders.
Medical coding software:
Medical coding software such as EncoderPro and Flash Code are essential for remote coders. These software programs feature coding databases, coding guidelines, and advanced search functions that streamline the coding process and enhance accuracy.
Code books:
Remote medical coders often refer to code books such as ICD-10, CPT, and HCPCS for accurate coding. These code books contain a comprehensive list of codes and guidelines used in medical coding, ensuring adherence to standardized coding practices.
Work Environment for Remote Medical Coders
The work environment for remote medical coders differs from traditional healthcare settings. Some key aspects of the work environment include:

Home-based or remote work setup:
Remote medical coders typically work from home or another location of their choice. This setup offers flexibility and eliminates the need for commuting to a physical office.
Virtual collaboration tools:
To facilitate communication and collaboration, remote medical coders utilize virtual collaboration tools such as email and video conferencing. These tools enable effective communication with healthcare providers, colleagues, and supervisors.
Secure internet connection and computer equipment:
To protect patient information and ensure the security of healthcare data, remote medical coders must have a secure internet connection and access to necessary computer equipment. This includes firewalls, antivirus software, and encryption to safeguard sensitive data.
Flexible working hours and autonomy:
Remote medical coders often have the flexibility to determine their working hours within certain constraints. This autonomy allows them to customize their schedule to suit personal preferences and balance professional and personal commitments.
Challenges Faced by Remote Medical Coders
While remote medical coding offers many advantages, it also presents some unique challenges. Some of the challenges faced by remote medical coders include:

Maintaining focus and productivity in a home-based environment:
Working from home can present distractions and challenges in maintaining focus and productivity. Remote medical coders must have the discipline to create a conducive work environment and establish effective routines to maximize productivity.
Adapting to changes in coding guidelines and regulations:
The healthcare industry is constantly evolving, with frequent changes to coding guidelines and regulations. Remote medical coders must stay updated with these changes and adapt their coding practices accordingly to ensure compliance and accuracy.
Troubleshooting technical issues:
Being solely responsible for their technical setup, remote medical coders may encounter technical issues that can affect their work. Troubleshooting these issues can prove to be challenging, requiring technical knowledge or seeking assistance.
Lack of direct interaction with healthcare providers:
Remote medical coders may have limited direct interaction with healthcare providers, which can sometimes pose challenges in obtaining clarifications or additional information necessary for accurate coding. Effective communication becomes crucial to bridge this gap.
Career Growth Opportunities for Remote Medical Coders
Remote medical coders have various career growth opportunities within the field. These opportunities include:
Advancement in coding specialties:
Remote medical coders can specialize in specific areas of medical coding, such as inpatient coding, outpatient coding, or risk adjustment coding. Specializing in a particular coding area allows for career advancement and increased job opportunities.
Supervisory or management roles:
As remote medical coders gain experience and expertise, they may progress into supervisory or management roles. These positions involve overseeing coding teams, ensuring quality control, and implementing best practices.
Consulting or auditing:
Experienced remote medical coders may transition into consulting or auditing roles, where they provide expertise and guidance to healthcare organizations. They may review coding practices, identify areas for improvement, and assist in compliance with coding guidelines and regulations.
Continuing education and professional development:
Remote medical coders can pursue continuous education and professional development opportunities to enhance their skills and knowledge. This may include attending workshops, webinars, or conferences to stay updated with industry changes and improve coding proficiency.
Tips for Becoming a Remote Medical Coder
For those aspiring to become remote medical coders, there are several valuable tips to consider. These tips include:
Acquire relevant education and training:
Pursue post-secondary education or training programs focused on medical coding to gain the necessary knowledge and skills. These programs provide a comprehensive understanding of medical coding principles, coding systems, and healthcare regulations.
Obtain a recognized coding certification:
Certifications such as CPC, CCS, CPB, COC, CIC, or CRC add credibility and validate proficiency in medical coding. Obtaining a recognized coding certification enhances job prospects and demonstrates expertise to potential employers.
Build a strong foundation in medical terminology and coding systems:
Develop a solid understanding of medical terminology, anatomy, and physiology. Familiarize yourself with coding systems like ICD-10, CPT, and HCPCS to accurately assign codes and ensure compliance with coding guidelines.
Gain experience through internships or entry-level positions:
Seek opportunities to gain practical experience through internships or entry-level positions. This hands-on experience allows aspiring remote medical coders to apply their skills in real-world scenarios, build a professional network, and enhance their resumes.
Develop strong analytical and problem-solving skills:
Develop analytical thinking and problem-solving skills to excel as a remote medical coder. Analyzing medical records, identifying coding discrepancies, and resolving coding-related issues require critical thinking and attention to detail.
Stay updated with industry changes and coding updates:
The healthcare industry is dynamic, with constant changes in coding guidelines and regulations. Stay updated with industry news, subscribe to coding newsletters, and participate in continuing education opportunities to remain current and adaptable.
Network with professionals in the field:
Network with other medical coders, healthcare professionals, and industry experts to learn from their experiences and gain insights. Professional associations, online forums, and social media platforms can facilitate networking opportunities.
Adopt efficient time management and organizational skills:
Working remotely requires discipline and effective time management. Develop organizational skills, plan your tasks, and set priorities to ensure productivity and meet deadlines.
Consider joining professional associations and attending conferences:
Join professional associations relevant to medical coding, such as the AAPC or AHIMA. These associations offer resources, networking events, and conferences that provide valuable knowledge, industry updates, and networking opportunities.
Continuously improve coding accuracy and productivity:
Strive for continuous improvement in coding accuracy and productivity. Regularly review your coding practices, seek feedback, and implement strategies to enhance coding efficiency and accuracy.
In conclusion, remote medical coders play a crucial role in accurately coding and classifying medical services. Their responsibilities, skills, and knowledge enable healthcare providers to streamline billing, ensure compliance, and facilitate efficient healthcare processes. With the right education, training, certifications, and dedication to continuous improvement, aspiring remote medical coders can embark on a rewarding career in this field.