In this article, we’ll explore whether a strong math background is necessary for a career in medical billing and coding. We’ll discuss the specific math skills that are required, as well as the level of proficiency needed to excel in this field. We’ll also provide some tips and resources for improving your math skills if you feel they are lacking. By the end, you’ll have a clear understanding of the role of math in medical billing and coding, and whether it’s a skill you need to prioritize in your training.

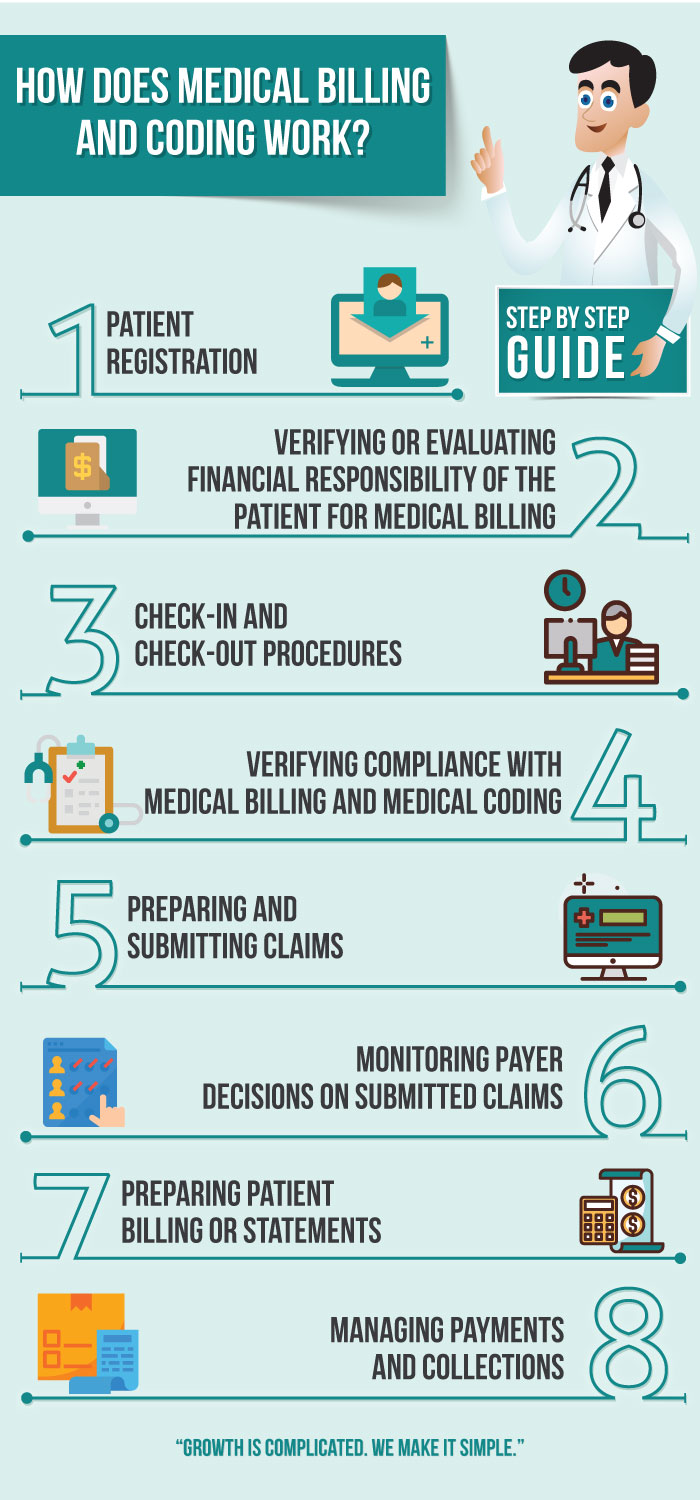
What is Medical Billing and Coding?
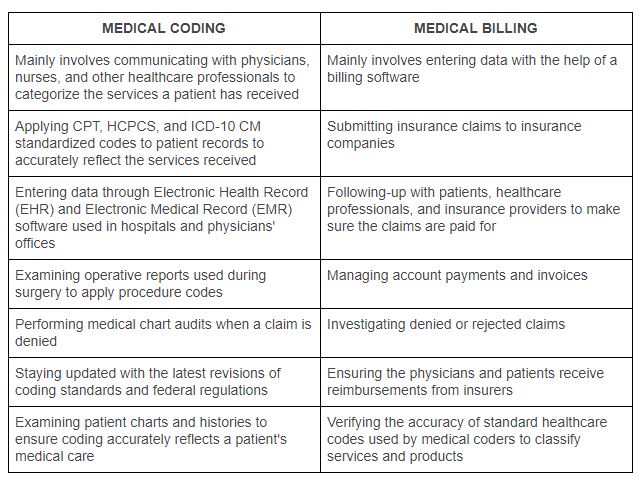
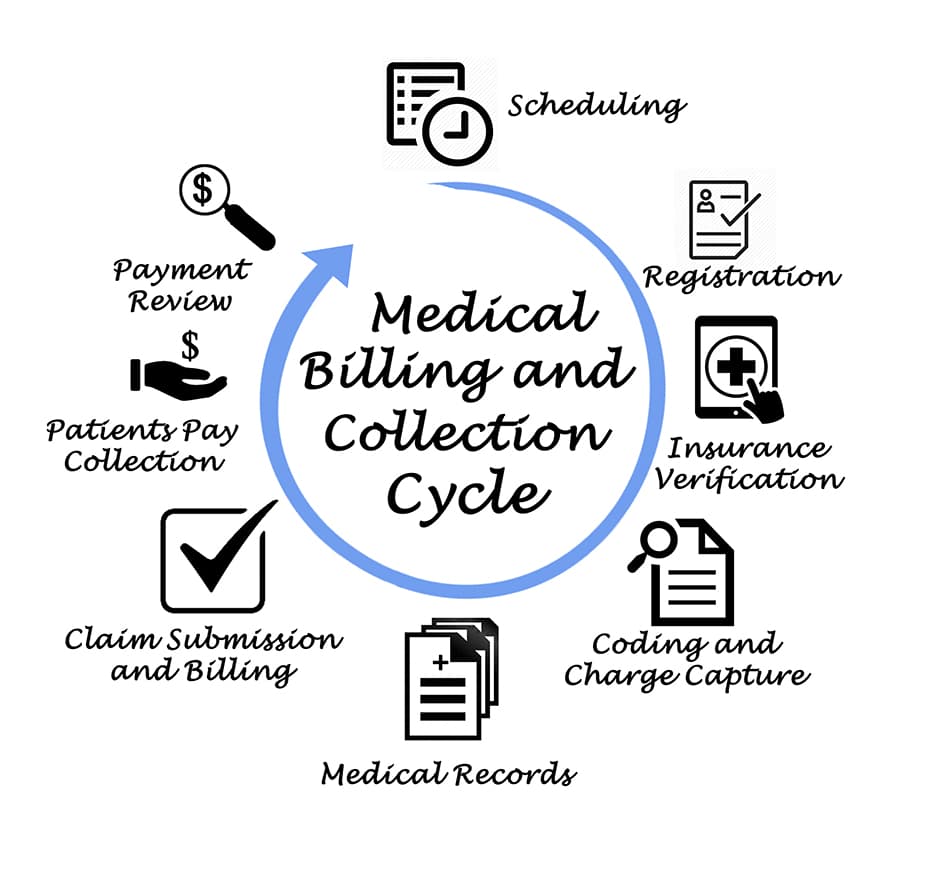
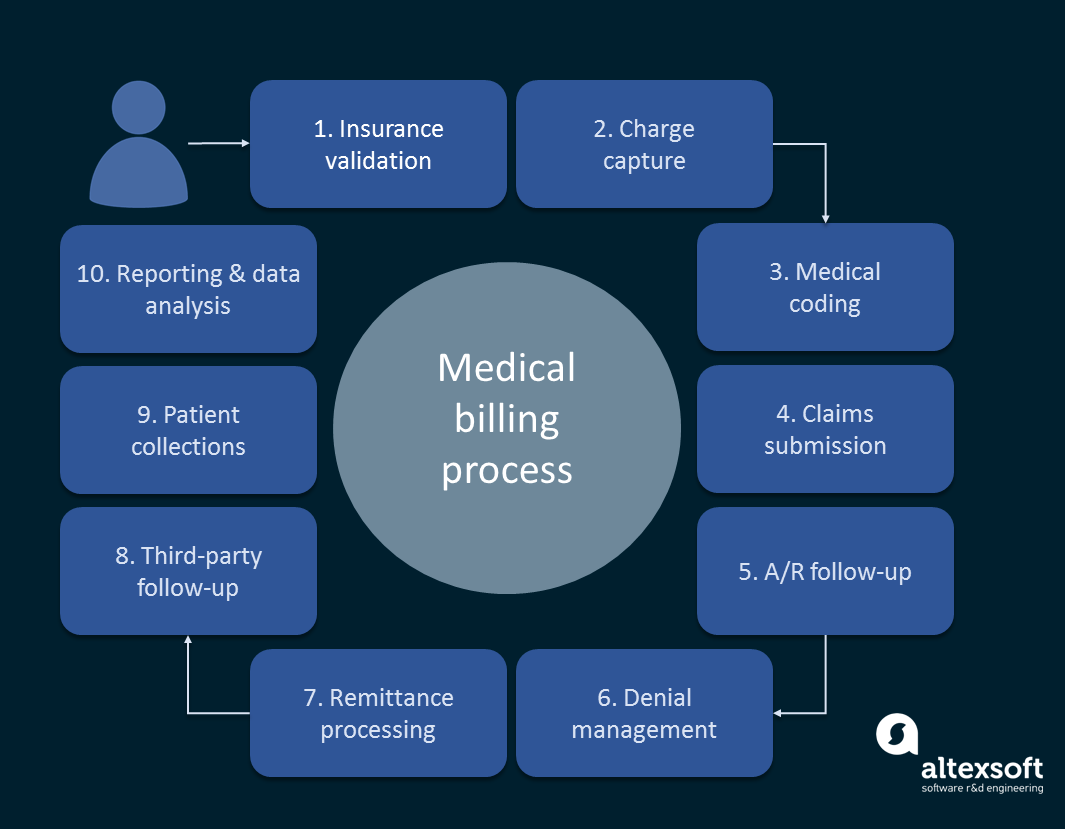
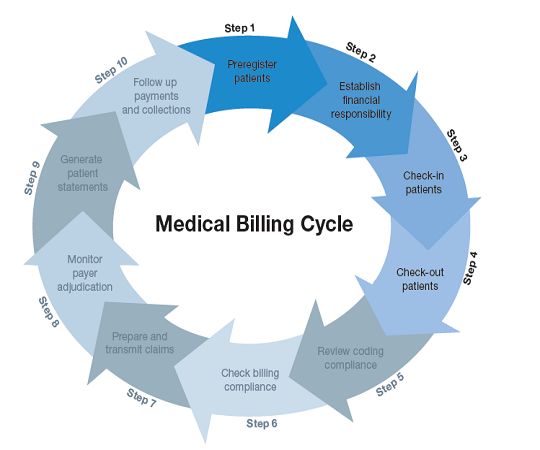
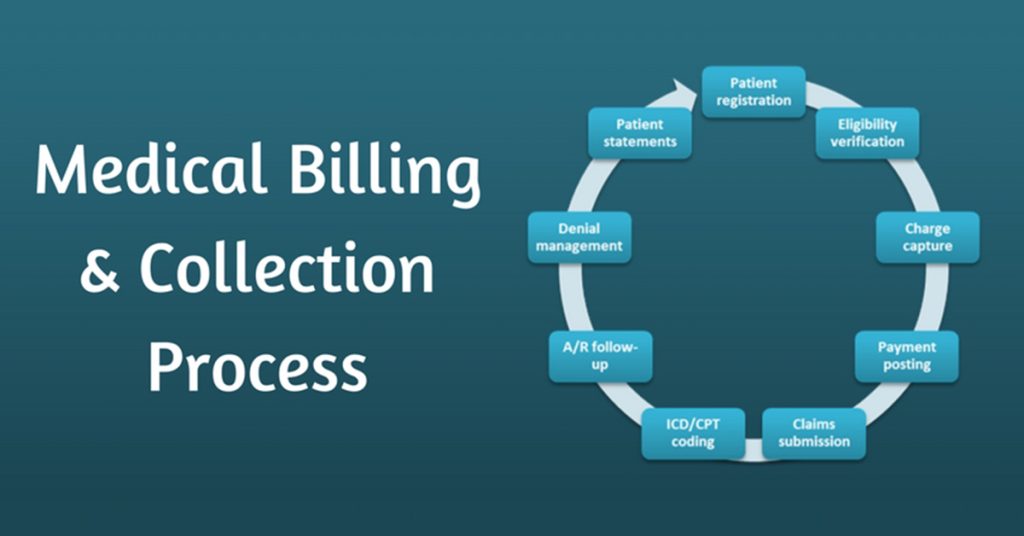
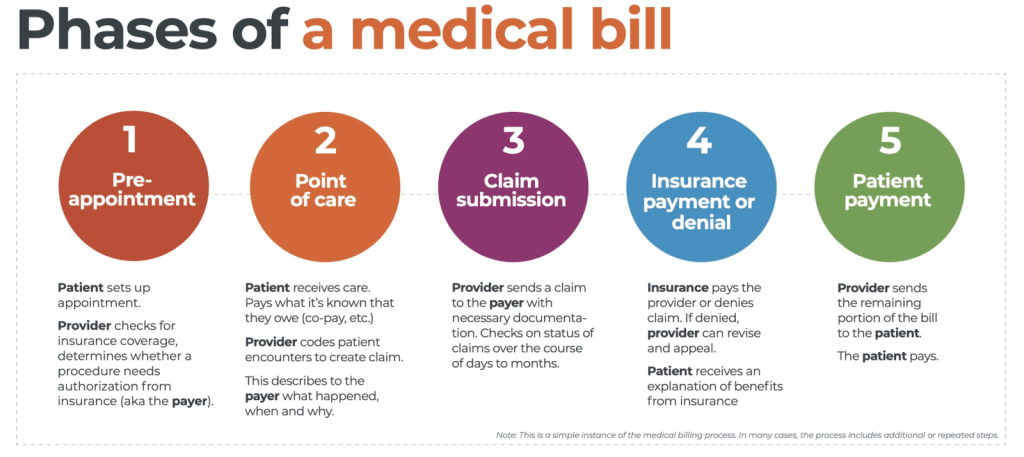
Medical billing and coding is a crucial aspect of the healthcare industry. It involves two distinct processes: medical coding and medical billing. Medical coding is the process of assigning standardized numeric or alphanumeric codes to diagnosis, procedures, and treatments, while medical billing focuses on generating and submitting claims for reimbursement from insurance companies or patients. These codes are essential for accurate record-keeping, insurance claims, and financial transactions in healthcare facilities.
Definition of Medical Billing and Coding
Medical billing and coding is the backbone of healthcare administrative processes, facilitating the flow of information and finances between healthcare providers, insurance companies, and patients. It ensures that medical services are accurately documented, recognized, and paid for.
Roles and Responsibilities of Medical Billers and Coders
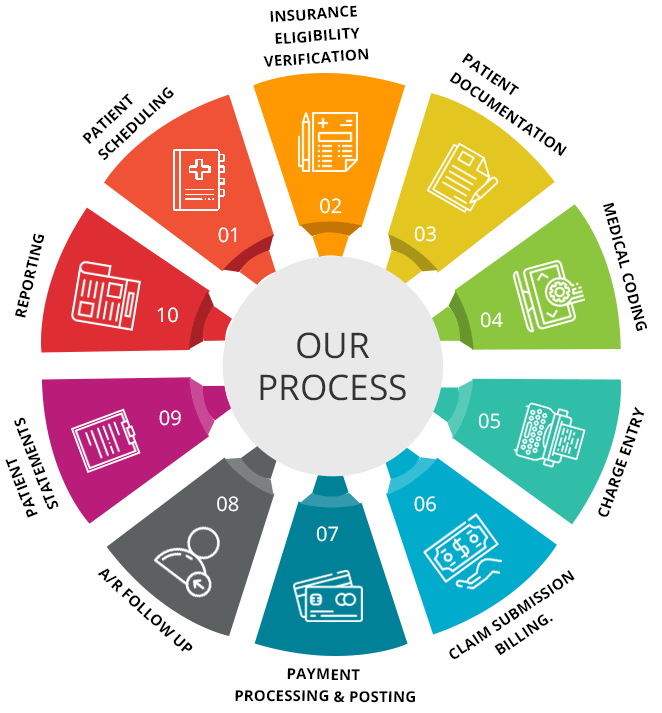
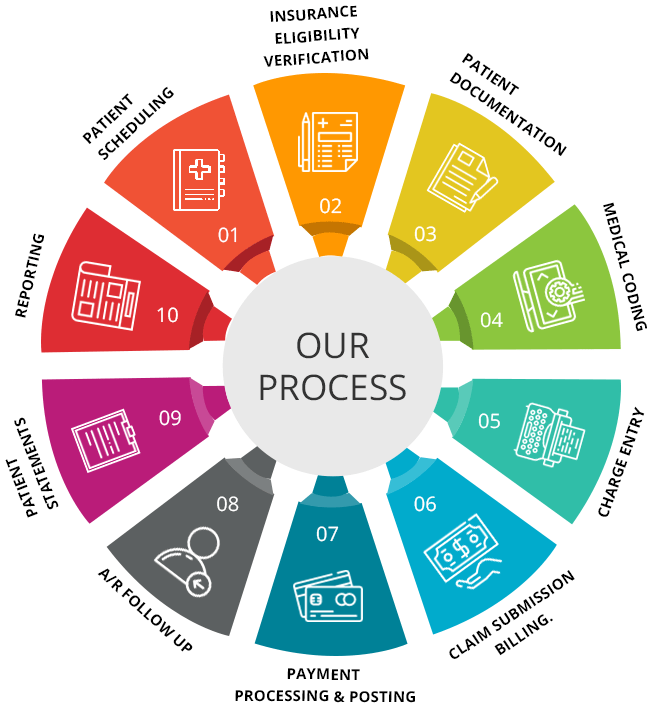
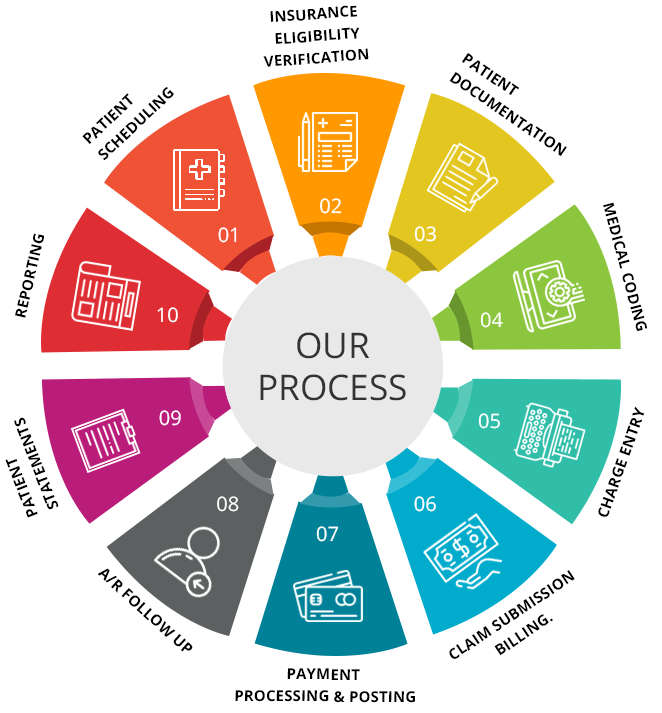
Medical billers and coders play a critical role in maintaining accurate medical records and ensuring that healthcare providers receive timely and appropriate payment for their services. The responsibilities of medical billers and coders may include:
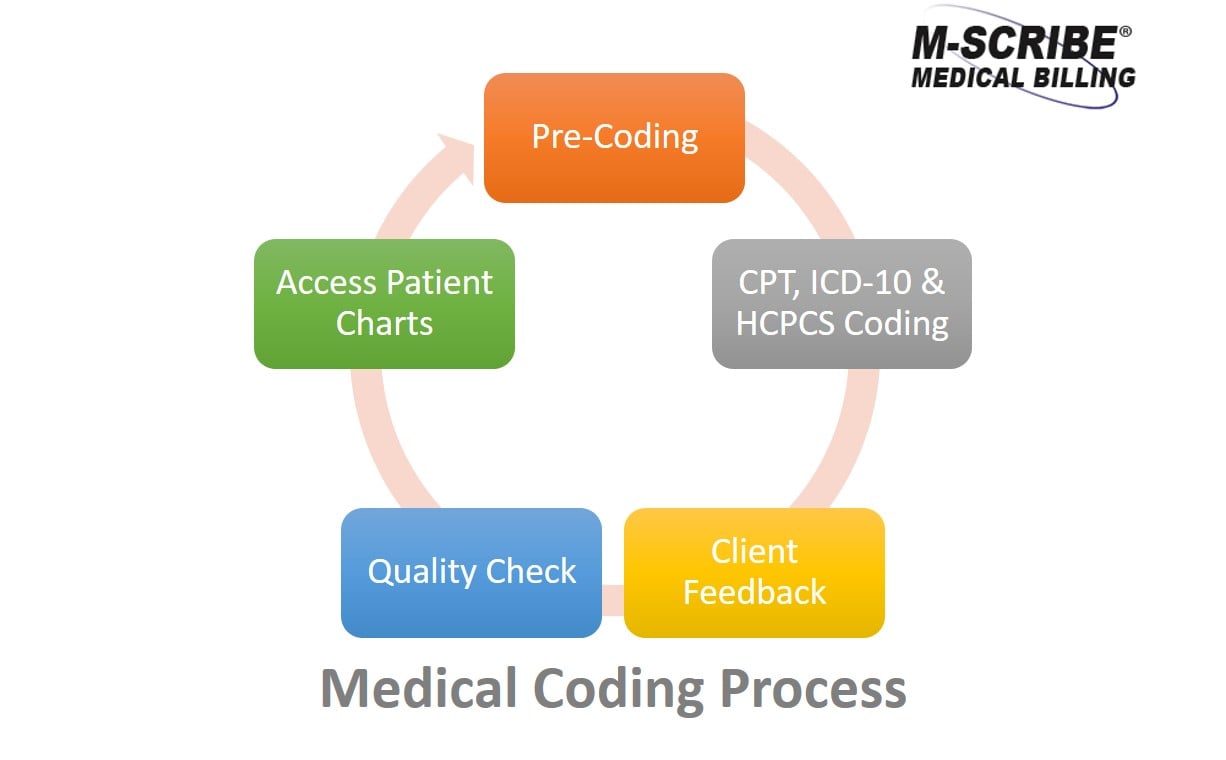
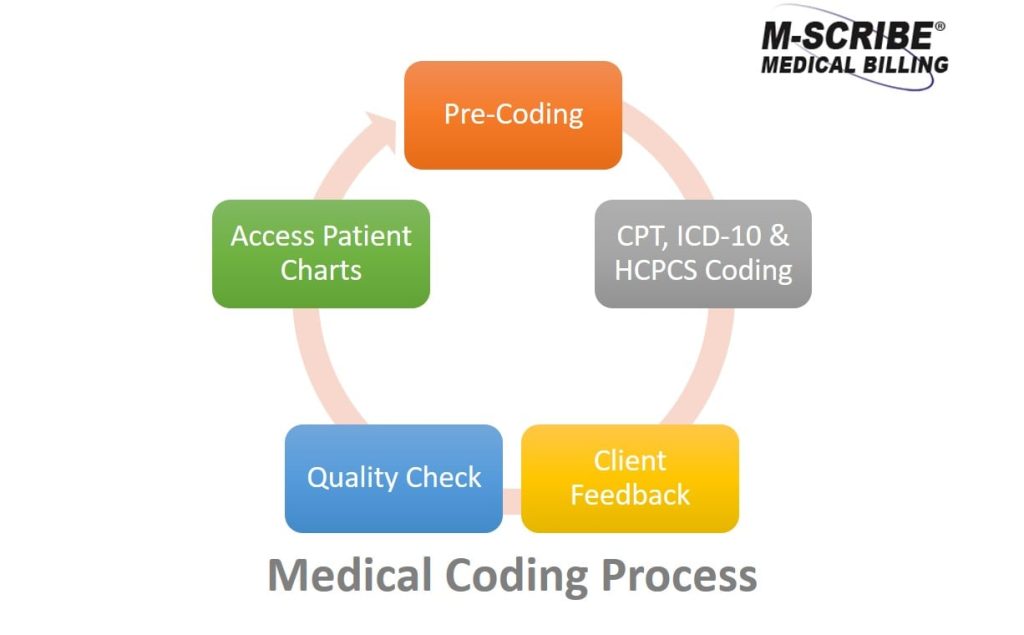
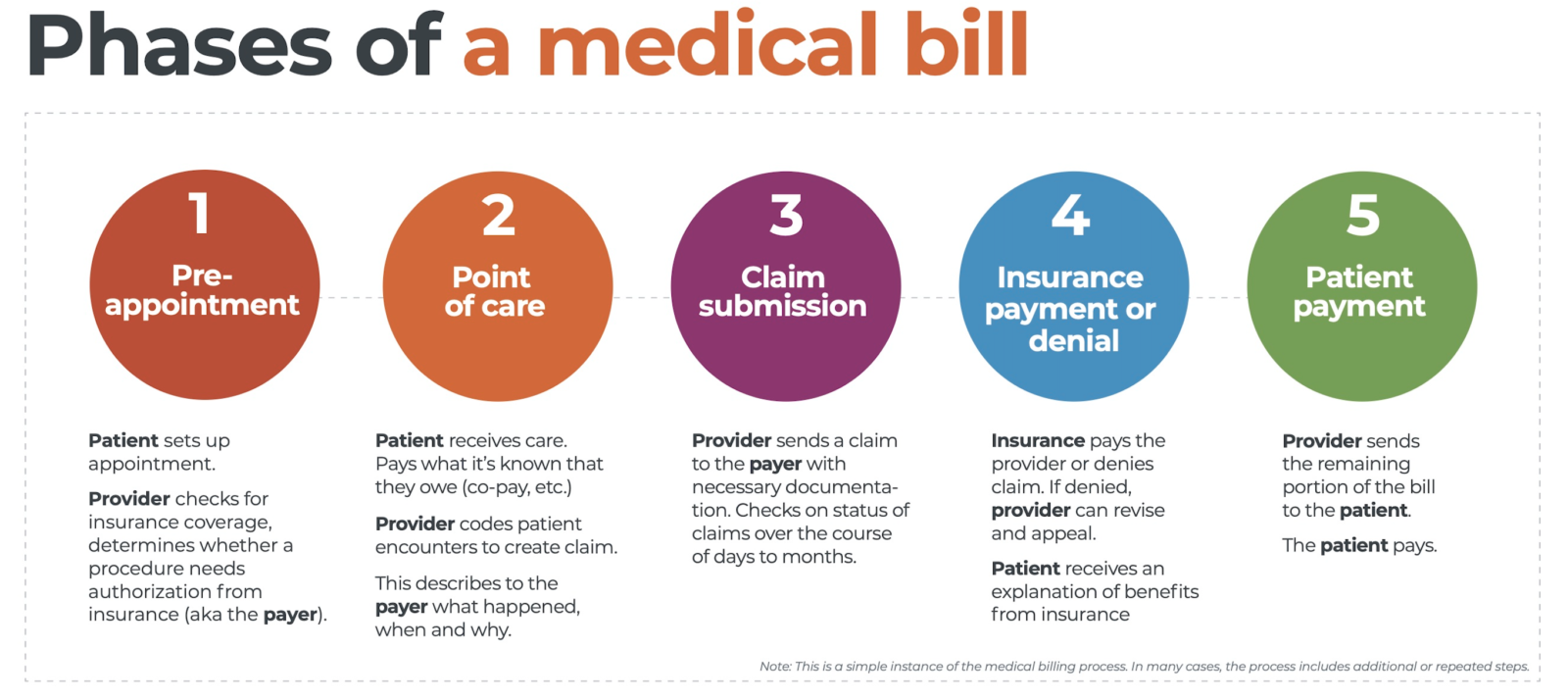
- Assigning appropriate codes: Medical coders analyze medical records and accurately assign codes to diagnoses, procedures, and treatments using industry-standard coding systems such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT).
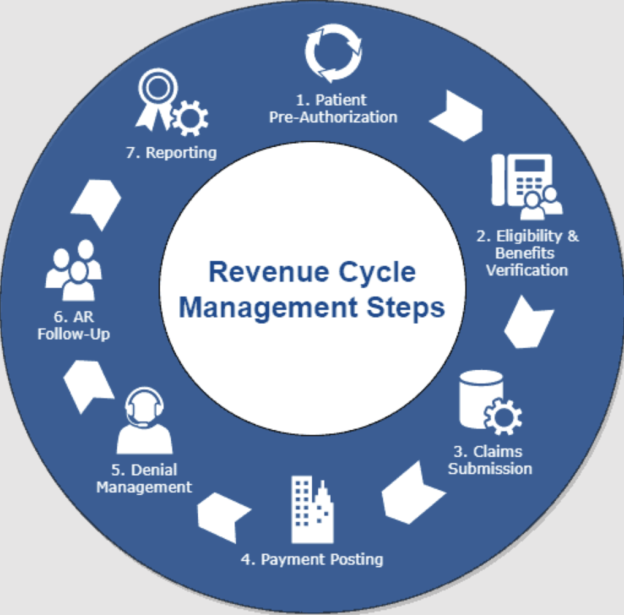
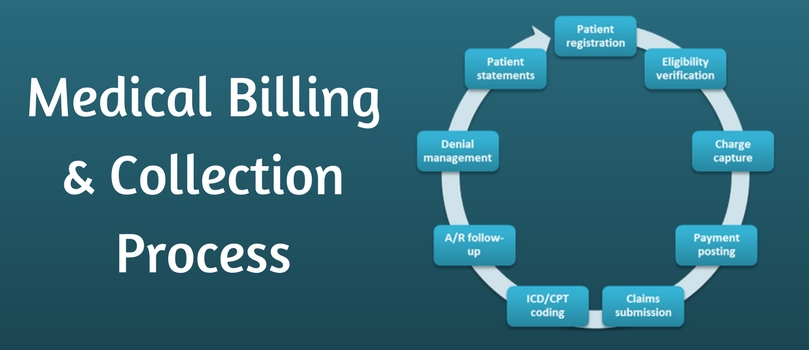
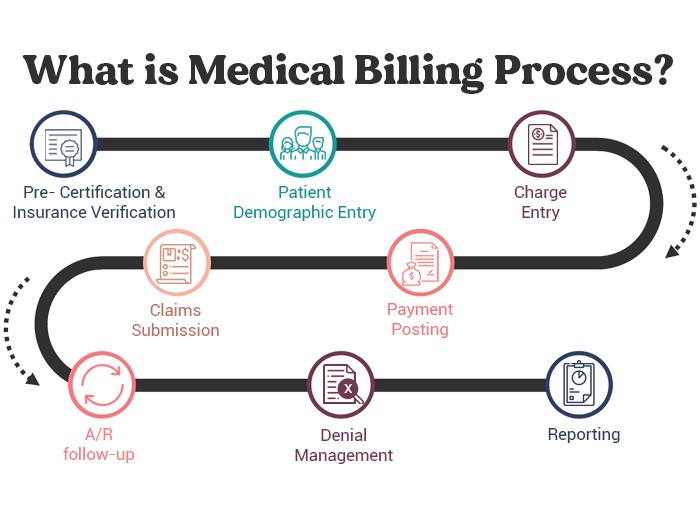
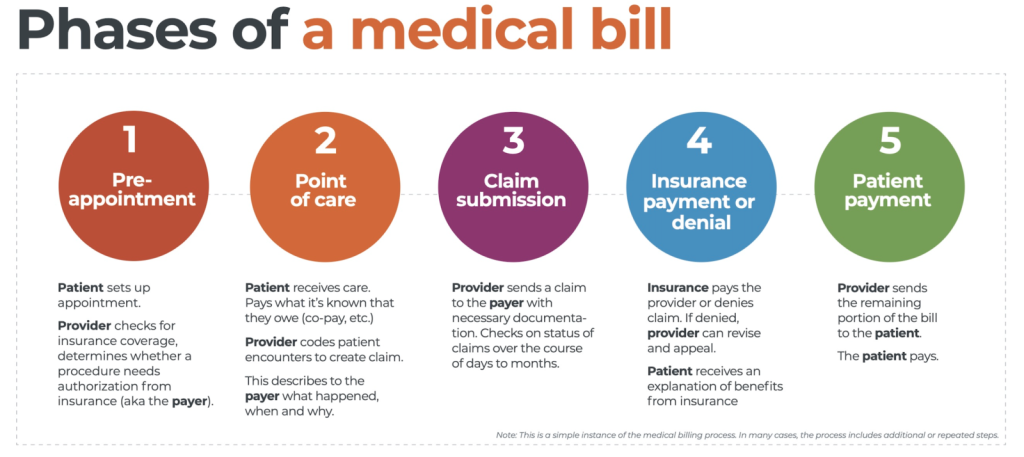
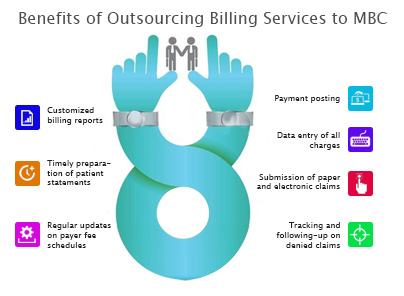
- Preparing and submitting claims: Medical billers compile the coded information, along with relevant patient and insurance details, to generate claims. These claims are then submitted to insurance companies or patients for reimbursement.
- Following up on claims: Medical billers track the progress of submitted claims, ensuring they are processed in a timely manner. They may communicate with insurance companies to resolve any issues or discrepancies that may arise during the reimbursement process.
- Handling patient billing: Medical billers also manage patient billing, including calculating and generating invoices for services rendered, sending out bills, and engaging in patient financial counseling.
Mathematical Skills in Medical Billing and Coding
Importance of Mathematical Skills in Medical Billing and Coding
Mathematical skills are fundamental in the field of medical billing and coding. Accuracy and precision are crucial when dealing with numbers, calculations, and financial transactions. A strong foundation in math enables medical billers and coders to perform their duties effectively and efficiently, minimizing errors and ensuring the smooth flow of financial records and insurance claims.
Mathematical Calculations Involved in Medical Billing and Coding
Medical billers and coders must be proficient in various mathematical calculations, such as:
- Addition and subtraction: These basic arithmetic operations are essential for calculating totals, deductibles, co-pays, and remaining balances on patient invoices.
- Multiplication and division: These operations are often required to determine the reimbursement amounts for specific procedures, calculate insurance coverage percentages, or divide costs among multiple payers.
- Percentage calculations: Medical billers and coders frequently deal with percentages when calculating discounts, copayment percentages, and reimbursement rates.
- Ratio and proportion: Understanding ratios and proportions is vital when determining the appropriate distribution of costs between insurance companies, patients, and healthcare providers.
- Statistical analysis: Medical billers and coders may need to interpret complex statistical data, such as reimbursement rates, utilization rates, and revenue projections. Having a grasp of statistical concepts and interpreting data accurately is important.
Basic Math Skills Required
Understanding and Interpreting Numbers
Medical billers and coders should be comfortable working with numbers and understanding their significance in the context of medical billing and coding. This includes interpreting numerical codes, numerical ranges, and numerical values associated with medical procedures, diagnoses, and treatments.
Performing Basic Arithmetic Calculations
Basic arithmetic calculations, such as addition, subtraction, multiplication, and division, are essential for medical billers and coders. These calculations are used daily to determine costs, reimbursement amounts, and patient balances. Proficiency in basic math skills ensures accurate calculations, preventing errors that could impact financial transactions and claims.
Advanced Math Skills Required

Understanding Percentages, Ratios, and Proportions
Advanced math skills become necessary when working with percentages, ratios, and proportions in medical billing and coding. Medical billers and coders must understand how to calculate percentages for copayments, discounts, or reimbursement rates. Similarly, they must be able to use ratios and proportions to allocate costs and determine fair distribution among payers.
Interpreting Complex Statistical Data
Interpreting complex statistical data is another advanced math skill required in medical billing and coding. Analyzing data such as reimbursement rates, utilization rates, and revenue projections requires a solid understanding of statistics and the ability to draw meaningful conclusions from the data. This skill is vital for decision-making and financial analysis in healthcare organizations.
The Relationship Between Math and Accuracy in Medical Billing and Coding

How Math Skills Contribute to Accuracy in Medical Billing and Coding
Math skills play a crucial role in ensuring accuracy in medical billing and coding. Incorrect calculations, misplaced decimal points, or misinterpreted numerical data can lead to significant financial discrepancies, denied claims, and delays in reimbursement. Strong math skills enable medical billers and coders to perform their duties meticulously, reducing the risk of errors and ensuring financial transactions align with actual services provided.
Examples of Math-Related Errors in Medical Billing and Coding
Math-related errors in medical billing and coding can have serious consequences. For example, miscalculating a patient’s co-pay percentage may result in an incorrect invoice amount, potentially straining the patient’s financial situation. Similarly, misinterpreting reimbursement rates may lead to underpayment or overpayment, affecting the financial health of healthcare providers. These errors can also lead to delays in claims processing and negatively impact the cash flow of healthcare facilities.
Training and Education for Math Skills in Medical Billing and Coding

Math Courses and Curriculum in Medical Billing and Coding Programs
Most medical billing and coding programs include math courses as part of their curriculum to ensure students develop the necessary mathematical skills for the profession. These courses cover basic arithmetic, percentages, ratios, proportions, and statistical analysis. By completing these courses, students gain the mathematical foundation required to perform accurate and efficient medical billing and coding.
Resources and Tools for Improving Mathematical Skills in the Field
Apart from formal education, medical billers and coders can enhance their mathematical skills through various resources and tools. Online tutorials, math refresher courses, and practice exercises specifically designed for medical billing and coding can provide valuable opportunities to strengthen mathematical abilities. Additionally, proficiency in spreadsheet software such as Microsoft Excel can aid in performing complex calculations and analyzing numerical data effectively.
Alternatives to Strong Math Skills
Using Technology and Software as a Substitute for Math Skills
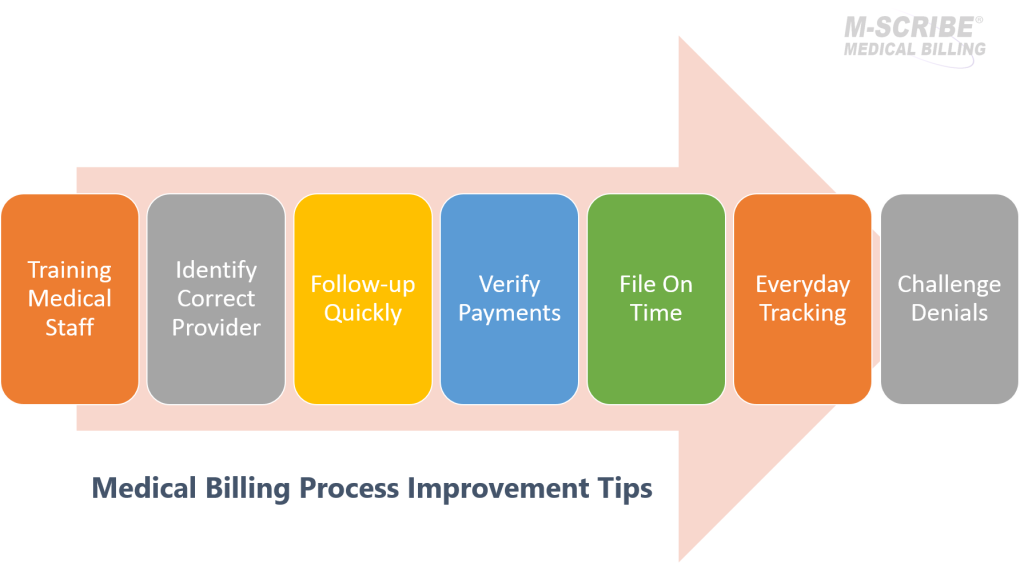
Advancements in technology and specialized software have made it easier for medical billers and coders to perform complex calculations and manage financial transactions without relying solely on strong math skills. Automated billing systems, coding software, and dedicated calculators can streamline mathematical calculations and reduce the potential for errors. This allows professionals to focus on interpreting and verifying the accuracy of the results rather than manually performing the calculations themselves.
Collaborating with Colleagues or External Resources
In cases where mathematical skills are not a strong suit for an individual medical biller or coder, collaboration with colleagues or seeking the assistance of external resources can be beneficial. Teamwork and support from colleagues with strong math skills can ensure accuracy in calculations. Additionally, consulting with accounting or financial professionals when needed can provide guidance and help resolve complex mathematical challenges.
Additional Skills and Qualifications Required in Medical Billing and Coding

Understanding Medical Terminology
Alongside mathematical skills, medical billers and coders must have a solid understanding of medical terminology. Familiarity with medical terms aids in accurately coding diagnoses and procedures, ensuring proper documentation and facilitating effective communication with healthcare providers and insurance companies.
Knowledge of Coding Systems and Regulations
Medical billers and coders must have a comprehensive understanding of coding systems, such as ICD and CPT, and keep up-to-date with coding regulations. Staying informed about coding updates and changes ensures accurate coding, claims submission, and compliance with industry standards and regulations.
Finding Success in Medical Billing and Coding without Strong Math Skills

Focusing on Strengths in Other Areas
While strong math skills are beneficial in medical billing and coding, individuals who are not naturally inclined towards math can still excel in the field by focusing on their strengths in other areas. Attention to detail, organization, communication, and problem-solving skills are equally important in this profession. Leveraging these strengths and combining them with basic mathematical abilities can contribute to success in medical billing and coding.
Seeking Additional Support and Development Opportunities
Continuous learning and professional development are essential for success in medical billing and coding. Individuals who feel their mathematical skills are lacking can seek additional support and development opportunities. Enrolling in refresher math courses, attending seminars or workshops, and actively seeking mentorship from experienced professionals can help improve mathematical abilities and enhance overall performance in the field.
Conclusion
In conclusion, while strong math skills are not an absolute requirement for a career in medical billing and coding, they are undeniably beneficial. The ability to accurately perform mathematical calculations, interpret numerical data, and apply statistical analysis contributes to accuracy, efficiency, and the overall financial health of healthcare organizations. However, alternatives such as technology and collaboration, along with complementary strengths in other areas, can still enable individuals to succeed in this field. Continuous learning, training, and leveraging available resources will ensure that medical billers and coders maintain proficient mathematical skills and adapt to the evolving demands of the healthcare industry.