If you are considering a career in the healthcare industry, you may have come across the field of medical billing and coding. But is medical billing and coding a good career choice? With the increasing demand for healthcare services, the answer is a resounding yes. In today’s fast-paced healthcare system, medical billing and coding professionals play a crucial role in ensuring accurate and timely processing of patient information and insurance claims. This article explores the reasons why pursuing a career in medical billing and coding can be a rewarding and promising path for those looking to enter the healthcare field.
Salary and Job Market

Average Salary
In the field of medical billing and coding, the average salary can vary depending on factors such as experience, education, and location. According to recent statistics, the median annual wage for medical records and health information technicians, which includes medical billers and coders, was $44,090 as of May 2020. However, it is important to note that salaries can range from around $28,000 to over $73,000, with professionals who have specialized certifications and extensive experience earning higher wages.
Job Growth
The job outlook for medical billing and coding professionals is promising. The healthcare industry is continuously expanding, and with it comes an increased need for trained professionals to manage and organize medical data. As electronic health records continue to become more prevalent, the demand for skilled medical billers and coders is expected to grow. The Bureau of Labor Statistics projects a 8 percent employment growth for medical records and health information technicians from 2019 to 2029, which is much faster than the average for all occupations.
Demand for Specialized Skills
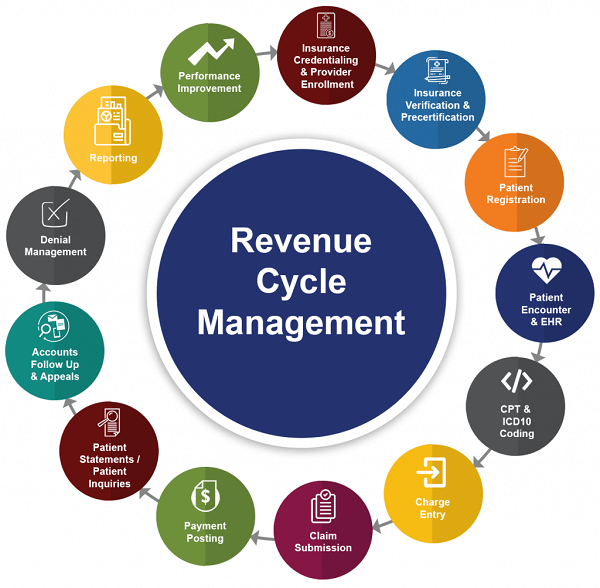
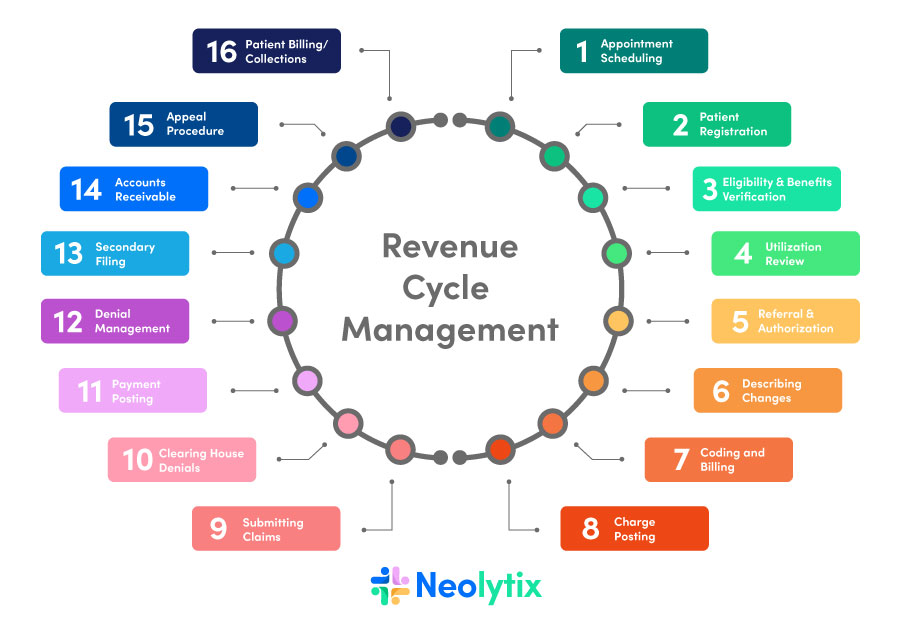
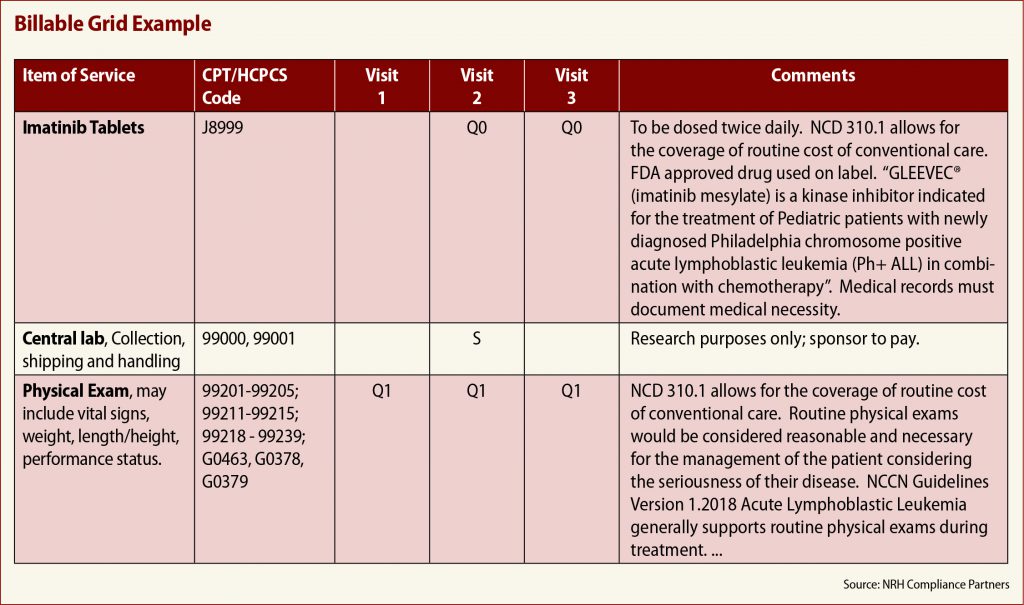
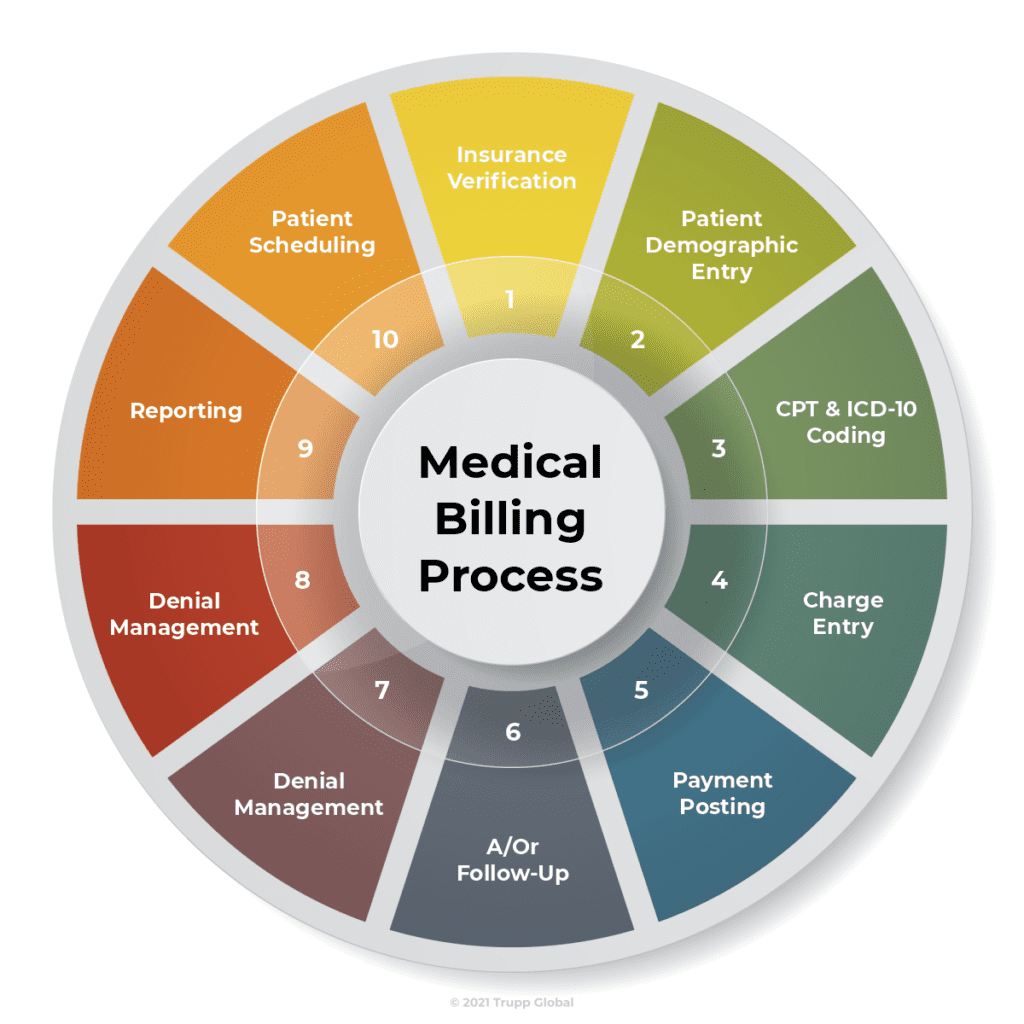
While healthcare organizations value professionals who possess a solid foundation in medical billing and coding, there is an increasing demand for specialized skills in this field. Knowledge and proficiency in coding systems such as ICD-10-CM and CPT are essential. Additionally, familiarity with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA) is crucial to ensure compliance and accuracy in medical billing and coding processes. Professionals who can demonstrate expertise in these areas may have an advantage in the job market and potentially earn higher salaries.
Job Stability and Security

Employment Opportunities
One of the major benefits of pursuing a career in medical billing and coding is the multitude of employment opportunities available. Medical billers and coders can work in a variety of healthcare settings, including hospitals, clinics, physician offices, long-term care facilities, and insurance companies. This versatility allows individuals to choose an environment that aligns with their preferences and career goals. Moreover, as the healthcare industry continues to grow, the demand for medical billing and coding professionals is expected to remain strong, providing job stability and security.
Remote Work Options
The COVID-19 pandemic has significantly impacted the way we work, and the field of medical billing and coding is no exception. With the advancement of technology, many healthcare organizations have transitioned to remote work arrangements, providing professionals with the opportunity to work from the comfort of their own homes. Remote work offers flexibility, eliminates the need for commuting, and provides a better work-life balance. This trend towards remote work in the medical billing and coding field is likely to continue, making it an appealing option for individuals seeking job stability with the added convenience of a flexible work environment.
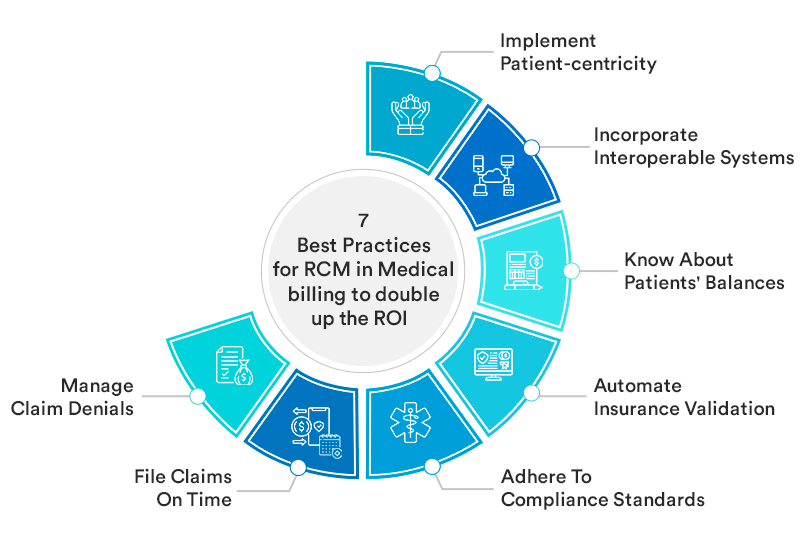
Industry Outlook
The medical billing and coding industry is expected to experience continued growth in the coming years. As healthcare organizations strive to streamline their operations, improve patient care, and maintain compliance with regulations, the demand for skilled professionals in this field will remain high. Additionally, advancements in technology, including the use of artificial intelligence and automation, will further shape the industry and create new opportunities for medical billers and coders. Staying up-to-date with the latest developments and continuously expanding one’s skill set will be crucial for professionals looking to thrive in this dynamic and ever-evolving industry.
Short Training Period

Duration of Training
One of the appealing aspects of pursuing a career in medical billing and coding is the relatively short training period required. Unlike other healthcare professions that may require several years of education, becoming a medical biller and coder typically involves obtaining a certificate or an associate degree, which can be completed in as little as 9-12 months. This shorter training period allows individuals to enter the workforce more quickly and start building their careers sooner.
Flexible Learning Options
The field of medical billing and coding offers a range of flexible learning options to accommodate different schedules and preferences. Many educational institutions offer online programs, allowing individuals to study at their own pace and from the comfort of their homes. Online courses often provide access to virtual classrooms, interactive learning materials, and dedicated instructors, ensuring a comprehensive educational experience. This flexibility in learning options makes it easier for individuals to balance their education with other commitments, such as work or family responsibilities.
Affordability
Another advantage of pursuing a career in medical billing and coding is the affordability of the required training programs. Compared to other healthcare professions that may have higher tuition fees, the cost of obtaining a certificate or an associate degree in medical billing and coding is generally more accessible. Additionally, there may be financial assistance options available, such as scholarships, grants, or student loans, to help alleviate the financial burden. This affordability factor makes it easier for individuals from diverse backgrounds to enter the field and pursue a rewarding career in medical billing and coding.
Transferable Skills

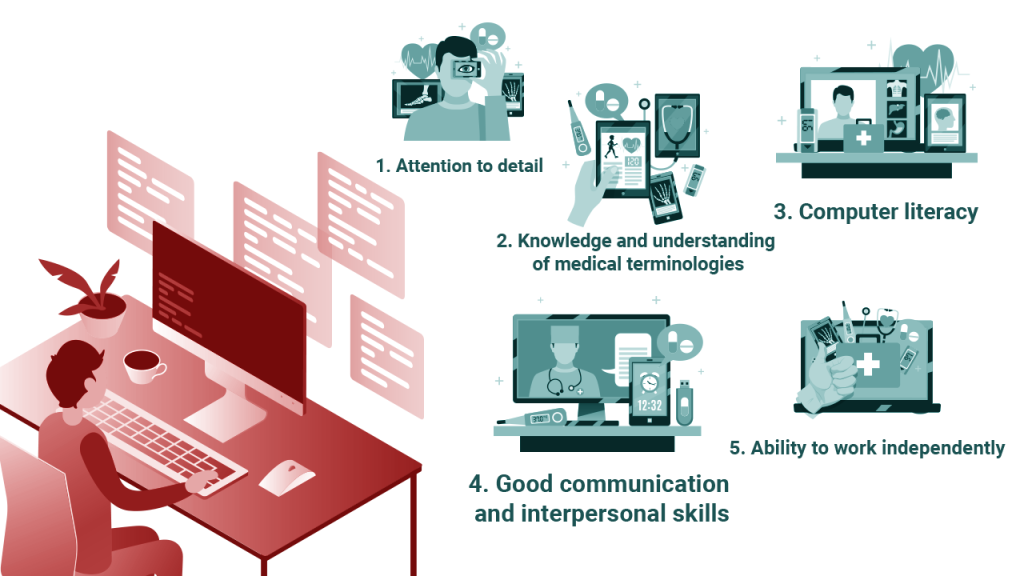
Attention to Detail
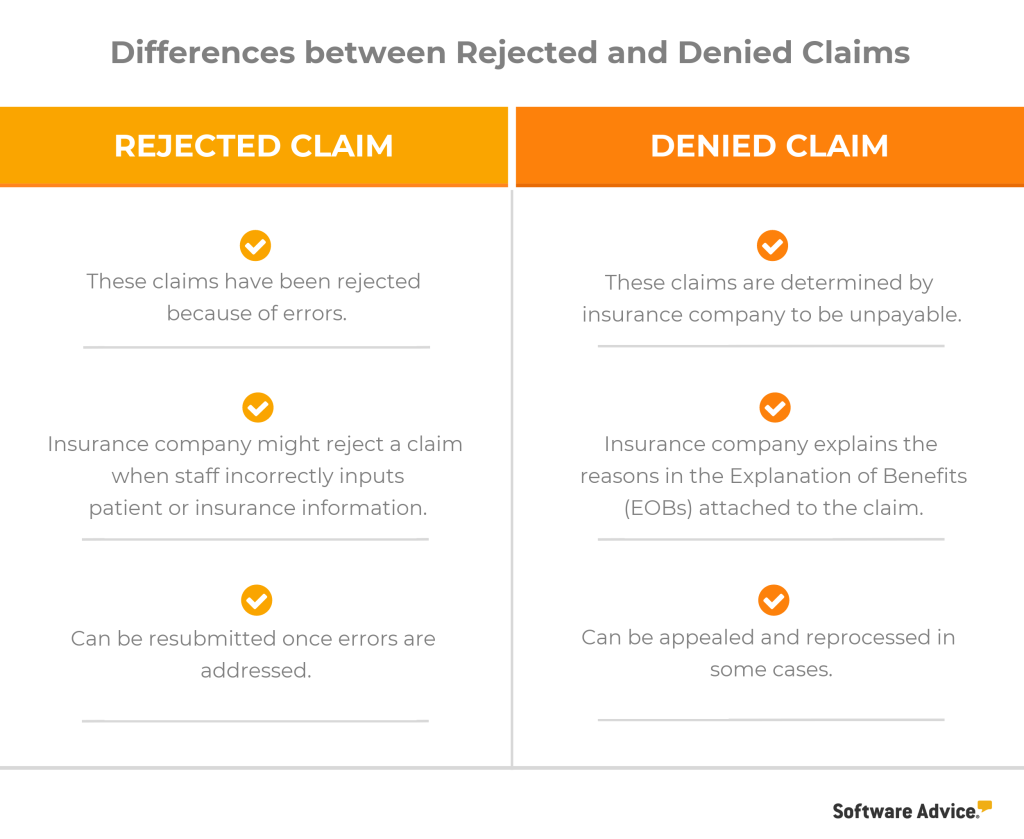
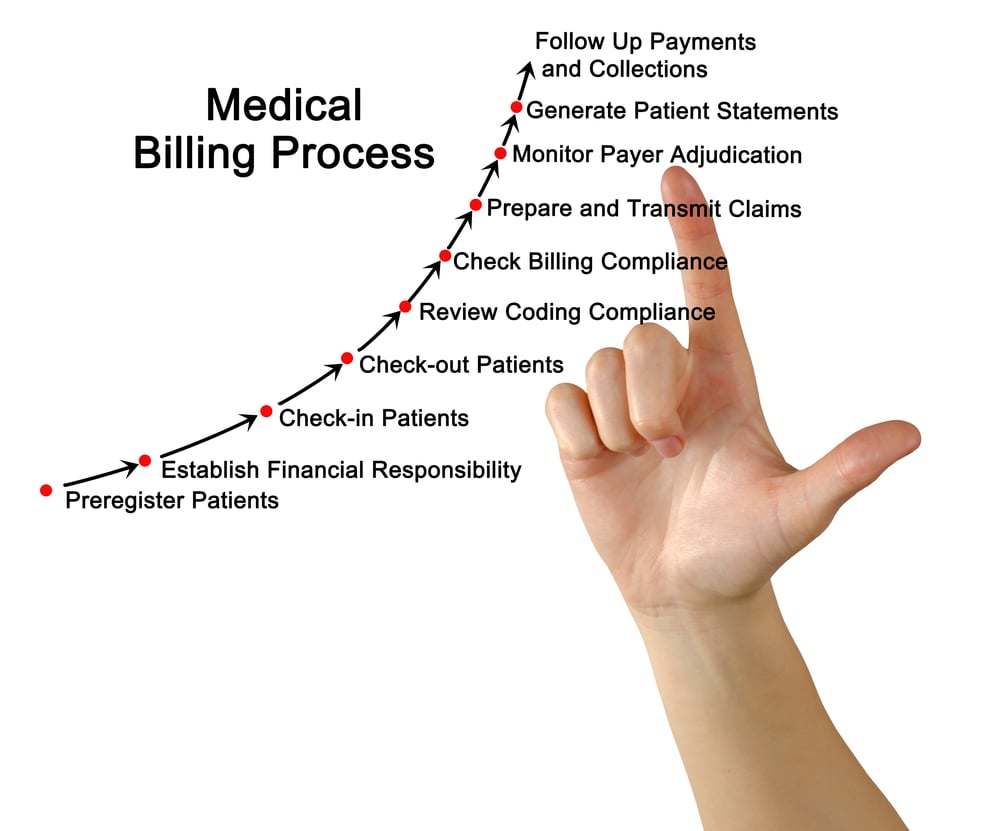
Attention to detail is a crucial skill for medical billing and coding professionals. Accuracy is of utmost importance when assigning codes and processing medical records, as Errors can lead to financial discrepancies, denied claims, and potential legal issues. Professionals in this field must possess the ability to closely review and analyze medical documentation, ensuring that all relevant information is captured accurately and coded appropriately. Developing and maintaining sharp attention to detail is vital for success in medical billing and coding.
Organizational Skills
Effective organizational skills are essential in the fast-paced and detail-oriented world of medical billing and coding. Professionals in this field are responsible for managing large volumes of medical records and ensuring that they are properly coded and processed in a timely manner. Strong organizational skills allow individuals to prioritize tasks, maintain efficient workflow, and effectively retrieve information when needed. By staying organized, medical billers and coders can contribute to the overall efficiency and success of healthcare organizations.
Analytical Thinking
Analytical thinking is a valuable skill for medical billing and coding professionals. It involves the ability to analyze complex medical documentation, identify relevant information, and apply coding guidelines accurately. This skill allows professionals to interpret medical charts, patient histories, and diagnostic reports, translating them into appropriate codes for billing and reimbursement purposes. Analytical thinking also comes into play when troubleshooting coding discrepancies, identifying potential errors, and ensuring compliance with industry standards and regulations. The ability to think critically and analytically is essential for success in the field of medical billing and coding.
Opportunities for Growth
This image is property of www.elearners.com.
Career Advancement
The field of medical billing and coding offers numerous opportunities for career advancement. As professionals gain experience and expertise, they can pursue roles with greater responsibilities, such as coding supervisors, medical records managers, or even healthcare administrators. Advancement may also come through specializing in a particular area of medical coding, such as coding for specific medical specialties or healthcare settings. Continuous professional development, obtaining specialized certifications, and staying up-to-date with industry trends are key to unlocking opportunities for growth in this field.
Specialization Options
Specializing in a specific area of medical billing and coding can open up new doors for career advancement and increased earning potential. Some professionals choose to specialize in coding for certain medical specialties, such as cardiology, orthopedics, or oncology. Others may focus on coding for specific healthcare settings, such as hospitals or outpatient clinics. Specialization allows individuals to develop a deeper understanding of the specific coding requirements and regulations within their chosen area, making them valuable assets to healthcare organizations seeking specialized expertise.
Continuing Education
Continuing education is vital for professionals in the medical billing and coding field to stay current with industry changes, coding updates, and evolving regulations. Technology, healthcare practices, and coding guidelines are constantly evolving, making it essential for professionals to engage in ongoing learning and professional development. Fortunately, there are numerous opportunities for continuing education, including workshops, conferences, online courses, and professional certifications. By investing in continuing education, individuals can stay ahead of the curve and position themselves for long-term career growth and success.
Work-Life Balance

Flexible Schedules
One of the many advantages of a career in medical billing and coding is the potential for flexible work schedules. Many healthcare organizations recognize the importance of providing their employees with work-life balance and offer options for flexible hours. This flexibility allows individuals to adapt their work schedules to fit personal commitments, such as childcare, education, or other responsibilities. Whether it’s working part-time, having the ability to choose shifts, or even working remotely, medical billing and coding professionals can enjoy a better work-life balance compared to some other healthcare professions.
Predictable Workflow
In the medical billing and coding field, professionals typically have a more predictable workflow compared to direct patient care roles. While there may be occasional periods of increased workload, such as during end-of-month billing cycles or when coding updates occur, overall, medical billers and coders can expect a consistent workflow. This predictability allows individuals to plan their time effectively, manage their workload, and maintain a balanced lifestyle. Knowing what to expect in terms of workload and deadlines contributes to reduced stress levels and a healthier work-life balance.
Limited Patient Interaction
For individuals who prefer less direct patient interaction, a career in medical billing and coding can be an ideal choice. While medical billers and coders play a crucial role in the healthcare system, their primary focus is on managing and organizing medical data, rather than engaging directly with patients. This aspect of the profession can be appealing to those who thrive in a more behind-the-scenes role. Medical billing and coding professionals still contribute to the quality and efficiency of patient care, but they do so in a manner that allows for a greater level of separation from direct patient interactions.
Job Satisfaction

This image is property of www.trainingdirectusa.com.
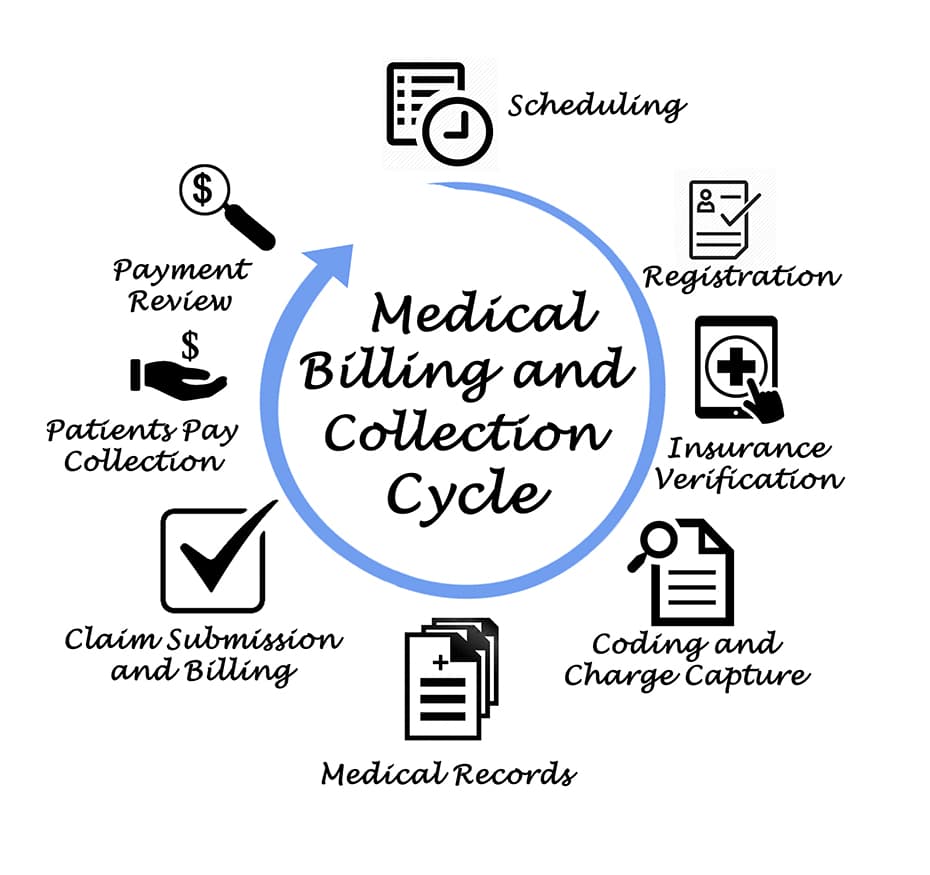
Contributing to Healthcare
One of the most rewarding aspects of a career in medical billing and coding is the opportunity to contribute to the healthcare industry. By accurately coding and managing medical records, professionals in this field ensure that healthcare providers are appropriately reimbursed for the services they provide. This, in turn, helps to maintain the financial health of healthcare organizations and supports the delivery of quality patient care. Knowing that their work directly impacts the functioning of the healthcare system can provide a sense of fulfillment and job satisfaction for medical billers and coders.
Positive Work Environment
Medical billing and coding professionals typically work in environments that prioritize teamwork, collaboration, and mutual support. Healthcare organizations understand the importance of creating a positive work environment that promotes employee well-being, job satisfaction, and productivity. This positive atmosphere fosters relationships with colleagues, encourages professional growth, and provides opportunities for learning and mentorship. Being part of a supportive work environment can significantly contribute to the overall job satisfaction in the medical billing and coding field.
Professional Fulfillment
In addition to the contributions made to the healthcare industry, professionals in the field of medical billing and coding can experience a sense of professional fulfillment. Mastering the intricacies of medical coding systems, staying up-to-date with industry regulations, and successfully navigating the complexities of healthcare billing can be intellectually stimulating. This continuous learning, growth, and mastery of specialized skills can provide a sense of achievement and professional satisfaction. Moreover, the ability to support healthcare providers in their mission to improve patient outcomes adds an additional layer of purpose and fulfillment to the work of medical billers and coders.
Challenges in the Field

Constant Learning
The field of medical billing and coding is ever-evolving, with constant changes in coding systems, industry regulations, and technology advancements. Medical billers and coders must stay up-to-date with these changes to ensure accuracy and compliance in their work. This ongoing learning process can be challenging and requires commitment to continuous professional development. However, for individuals who enjoy intellectually stimulating work and are eager to embrace new knowledge and skills, the continuous learning aspect of the field can be seen as an opportunity for personal and professional growth.
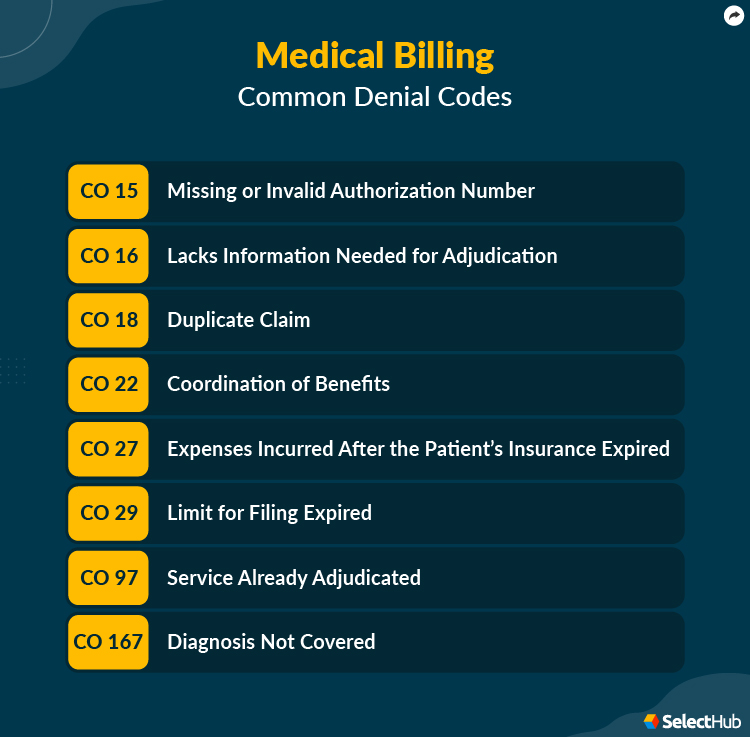
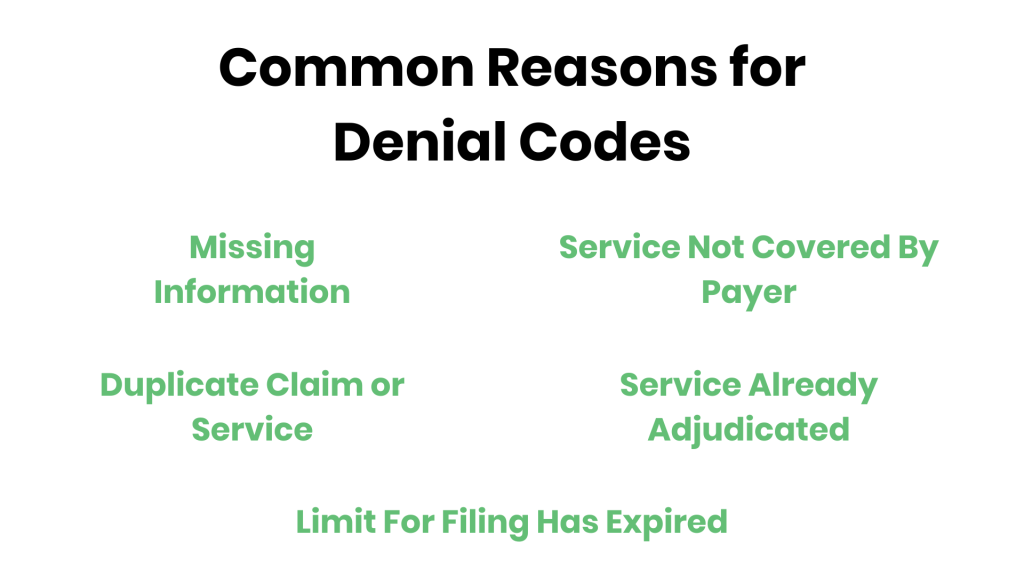
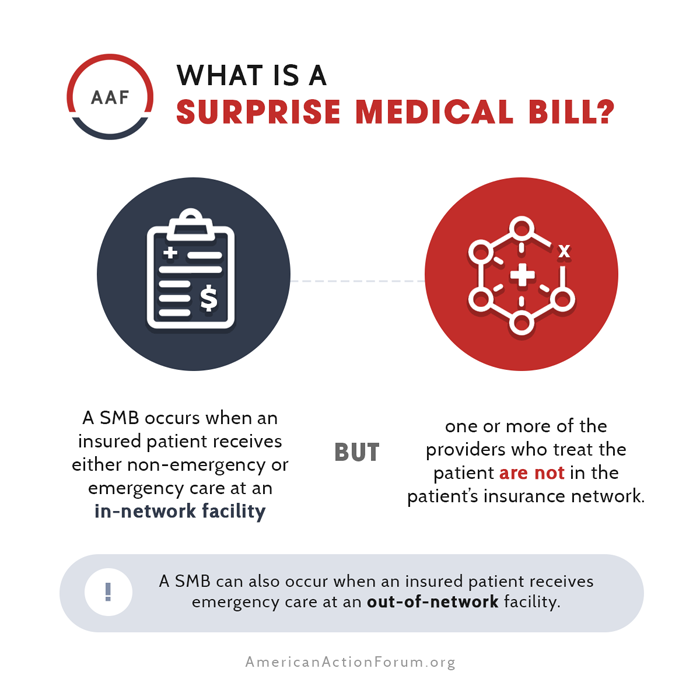
Keeping Up with Regulations
Regulations play a crucial role in the field of medical billing and coding, and their frequent updates can pose a challenge for professionals. It is essential for medical billers and coders to stay informed about changes in healthcare regulations, such as HIPAA and the ACA, to ensure compliance in their daily work. Failing to stay updated can result in coding errors, billing discrepancies, and potential legal issues. Maintaining a strong understanding of regulations and actively seeking out opportunities for education and training on compliance are essential for success in the field.
Managing Stress
Like any profession in the healthcare industry, medical billing and coding can be stressful at times. Professionals in this field often work under tight deadlines and must handle large volumes of data with meticulous attention to detail. Coping with the pressure of accuracy, managing increased workload during busy periods, and adapting to changes in coding systems or regulations can be challenging. Developing effective stress management techniques, such as time management, meditation, or exercise, can help medical billers and coders maintain a healthy work-life balance and reduce stress levels.
Work Environment

This image is property of southbend.iu.edu.
Employment Settings
Medical billing and coding professionals have the opportunity to work in various healthcare settings. These settings include hospitals, clinics, physician offices, long-term care facilities, and insurance companies. The diverse range of employment settings allows individuals to choose a work environment that aligns with their interests and preferences. Whether a professional prefers the fast-paced environment of a hospital or the more intimate setting of a small clinic, there are options available to suit different work styles and career goals.
Team Collaboration
Collaboration is an essential aspect of the medical billing and coding field. Professionals in this field often work closely with healthcare providers, physicians, nurses, and other administrative staff to ensure accurate coding and billing practices. Effective communication and collaboration are vital to ensure the availability of comprehensive medical records and the timely processing of claims. Working in a collaborative team environment provides opportunities for knowledge sharing, learning from others, and fostering a sense of camaraderie among colleagues.
Technological Advancements
Advancements in technology have significantly impacted the field of medical billing and coding. The use of electronic health records (EHRs) has streamlined processes, improved efficiency, and enhanced the accuracy of medical documentation. Medical billing and coding professionals now have access to sophisticated coding software and tools that automate certain processes, reducing the potential for human error and increasing productivity. Staying abreast of technological advancements in the field and being open to embracing new tools and systems is crucial for professionals in ensuring they remain competitive and efficient in their work.
Job Requirements

Required Skills and Knowledge
To excel in the field of medical billing and coding, professionals must possess a specific set of skills and knowledge. Strong attention to detail, organizational skills, and analytical thinking are essential qualities. In addition, individuals need a solid understanding of medical terminology, anatomy, and physiology. Proficiency in coding systems, such as ICD-10-CM and CPT, is also crucial. Effective communication skills, both written and verbal, are necessary to correspond with healthcare providers and insurance companies. Furthermore, familiarity with industry regulations, including HIPAA and the ACA, is vital to ensure compliance in medical billing and coding processes.
Certifications
Obtaining professional certifications in medical billing and coding is highly beneficial for individuals looking to enhance their career prospects and demonstrate their expertise in the field. The American Academy of Professional Coders (AAPC) and the American Health Information Management Association (AHIMA) offer reputable certifications, such as the Certified Professional Coder (CPC) and the Certified Coding Specialist (CCS), respectively. These certifications validate one’s knowledge and proficiency in medical coding and can open up new opportunities for career advancement and higher salaries. Maintaining these certifications requires continuous education, ensuring professionals stay current with industry changes and advancements.
Continuing Education
Continuing education is a fundamental aspect of a successful career in medical billing and coding. Medical coding systems, regulations, and industry practices are constantly evolving, requiring professionals to stay updated with the latest developments. Continuous education can be achieved through attending conferences, workshops, and online courses that provide opportunities for learning and staying ahead of industry changes. Additionally, many professional organizations offer resources, webinars, and publications to support ongoing professional development. Committing to continuous education ensures that medical billing and coding professionals remain competitive and capable of delivering high-quality work.