Medical coders play a vital role in the healthcare industry by meticulously analyzing medical records and assigning appropriate alphanumeric codes to accurately represent diagnoses, procedures, and treatments. These codes are essential for insurance reimbursement, statistical analysis, and ensuring proper medical documentation. Highly skilled in medical terminology and coding guidelines, medical coders navigate through complex documentation to establish a seamless and standardized system that assists healthcare providers in delivering efficient and effective care. In this article, we will explore the intricacies of the medical coding profession, shedding light on the indispensable contributions they make to the healthcare field.
Medical Coding Overview
Medical coding is a crucial aspect of the healthcare industry, ensuring that accurate and consistent codes are assigned to medical diagnoses, procedures, and treatments. This process involves transforming medical information into universally recognized codes that can be used for billing, reimbursement, and statistical analysis purposes.
Definition of Medical Coding
Medical coding is the process of assigning alphanumeric codes to specific medical procedures, diagnoses, and treatments in order to accurately represent the patient’s healthcare visit. These codes serve as a standardized language that enables healthcare providers, insurance companies, and other stakeholders to communicate and understand the services provided.
Importance of Medical Coding
Accurate medical coding is essential for several reasons. Firstly, it serves as the foundation for proper billing and reimbursement, ensuring that healthcare providers are appropriately compensated for the services they provide. Additionally, medical coding plays a pivotal role in maintaining patient records, facilitating research and analysis, and enabling the effective monitoring and management of public health.
Role of Medical Coders
Medical coders play a vital role in the healthcare industry, ensuring that accurate codes are assigned to medical procedures, diagnoses, and treatments. They are responsible for transforming complex healthcare documentation into precise and standardized codes that accurately represent the patient’s medical visit.
Assigning Medical Codes
A significant part of a medical coder’s role involves assigning appropriate codes to medical procedures, diagnoses, and treatments. This process requires a thorough understanding of coding guidelines, medical terminology, and familiarity with various code sets such as ICD-10-CM, CPT, and HCPCS. Accuracy in code assignment is crucial to ensure proper billing and reimbursement and to provide accurate data for research and analysis purposes.
Ensuring Accuracy and Compliance
Medical coders must ensure the accuracy and compliance of assigned codes. This involves reviewing medical documentation, analyzing the patient’s medical history, and ensuring that codes align with established coding guidelines and regulations. Coders must pay attention to detail and have a deep understanding of coding rules to avoid errors or omissions that could lead to billing discrepancies or potential compliance issues.
Utilizing Medical Coding Guidelines
To ensure consistency and accuracy, medical coders adhere to established coding guidelines. These guidelines provide instruction on how to assign codes accurately and appropriately in various healthcare scenarios. Following these guidelines promotes clarity, reduces errors, and ensures that codes are assigned consistently across different healthcare providers and settings.
Medical Codes and Classification Systems
Medical coding relies on a variety of code sets and classification systems that are specifically designed to represent different aspects of medical encounters.

ICD-10-CM
ICD-10-CM, which stands for International Classification of Diseases, Tenth Revision, Clinical Modification, is the primary code set used to classify and code diagnoses in the United States. It provides a comprehensive list of codes that accurately describe a wide range of medical conditions, enabling accurate communication and statistical analysis.
CPT
CPT, or Current Procedural Terminology, is a code set that is used to identify and report medical procedures and services performed by healthcare providers. Developed and maintained by the American Medical Association (AMA), CPT codes cover a broad range of medical procedures and treatments, allowing for accurate billing and reimbursement.
HCPCS
HCPCS, or Healthcare Common Procedure Coding System, is a set of codes that are used to describe and bill for medical services and products not covered by CPT codes. HCPCS codes include durable medical equipment, drugs, supplies, and other healthcare services. These codes are essential for proper billing and reimbursement for items and services that fall outside the scope of CPT codes.
Reviewing Medical Records
A critical aspect of a medical coder’s role is reviewing medical records to extract and assign the appropriate codes accurately.
Understanding Patient Information
To accurately assign codes, medical coders must have a deep understanding of the patient’s medical history and the circumstances surrounding the medical encounter. This requires them to review and interpret medical records, including physician documentation, laboratory reports, and diagnostic imaging results. By carefully analyzing this information, coders can accurately determine the appropriate codes to represent the patient’s medical visit.
Extracting Relevant Codes
Medical coders must extract relevant codes from the patient’s medical records based on their understanding of various coding systems. This involves identifying the medical procedures performed, the diagnoses made, and any treatments provided during the encounter. By accurately extracting codes, coders ensure that the services rendered are appropriately represented and billed.
Verifying Documentation Accuracy
In addition to assigning codes, medical coders play a crucial role in verifying the accuracy and completeness of the documentation within medical records. This involves ensuring that all required elements, such as physician signatures, dates, and relevant reports, are present. Accurate and complete documentation is crucial for proper coding and billing, as well as for legal and compliance purposes.
Collaborating with Healthcare Professionals
Medical coders work closely with various healthcare professionals to ensure accurate coding and billing processes.

Working with Physicians and Nurses
Strong collaboration between medical coders and physicians or nurses is essential for accurate coding. Coders often communicate directly with healthcare providers to clarify any documentation uncertainties, obtain additional information, or seek guidance on appropriate code assignment. This collaboration ensures that codes reflect the true nature of the medical encounter and that accurate billing and reimbursement occur.
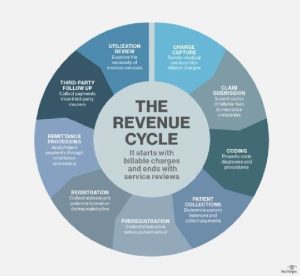
Communicating with Billing and Reimbursement Teams
Medical coders also collaborate closely with billing and reimbursement teams within healthcare organizations. This collaboration involves sharing coding information, discussing coding challenges, and ensuring that claims accurately reflect the services provided. Effective communication is crucial to address any discrepancies or issues promptly and to facilitate the revenue cycle process.
Medical Billing and Reimbursement
Medical coding and billing go hand in hand, with accurate coding serving as the foundation for proper billing and reimbursement.
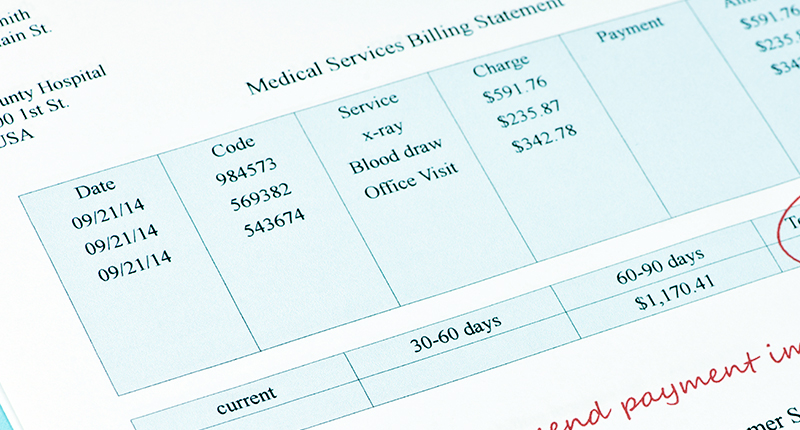
Submitting Claims and Invoices
Once codes have been assigned, medical coders work closely with billing teams to submit claims and invoices to insurance companies and other payers. They ensure that the correct and accurate codes are attached to the claims, along with all required documentation, such as laboratory results or operative reports. Timely submission of claims and invoices is crucial for timely reimbursement.
Following Insurance Guidelines
Medical coders must be knowledgeable about insurance guidelines to ensure that claims adhere to specific payer requirements. Different insurance companies may have different coding and billing criteria, and coders must stay up to date with these guidelines to ensure accurate claim submission. By following insurance guidelines, coders facilitate the reimbursement process and help avoid claim rejection or denial.
Resolving Rejection or Denial Issues
Medical coders play a crucial role in addressing claim rejection or denial issues. When claims are rejected or denied, coders analyze the reasons for rejection, identify any coding errors or discrepancies, and work collaboratively with the healthcare team to resolve these issues. Resolving rejection or denial issues in a timely manner is vital to ensure proper reimbursement for healthcare services.
Auditing and Compliance
Medical coders are responsible for conducting regular audits to ensure compliance with coding regulations and identify any coding errors or discrepancies.
Conducting Regular Audits
To maintain accuracy and compliance, medical coders must conduct regular audits of coded medical records. Audits can occur pre-billing, post-billing, or as part of ongoing quality assurance processes. These audits help identify any potential coding errors, inconsistencies, or deviations from coding guidelines, allowing for corrective actions to be implemented promptly.
Ensuring Compliance with Regulations
Compliance with coding regulations, such as those set by the Centers for Medicare and Medicaid Services (CMS), is of utmost importance in the healthcare industry. Medical coders must ensure that all codes assigned adhere to these regulations and that any coding deviations are appropriately documented and reported. Compliance with coding regulations ensures the accuracy and integrity of healthcare data and ultimately contributes to patient safety.
Identifying and Reporting Coding Errors
In the process of conducting audits, medical coders carefully review coded medical records for potential errors or discrepancies. When coding errors are identified, coders are responsible for reporting these errors to the appropriate individuals or departments for further investigation and resolution. This reporting process helps maintain accurate and reliable coding practices and ensures compliance with healthcare regulations.
Continuous Learning and Professional Development
In the rapidly evolving field of medical coding, continuous learning and professional development are essential for medical coders to stay updated and proficient in their roles.
Staying Updated with Coding Changes
Medical coders must actively stay informed about changes in coding guidelines, regulations, and advancements in medical technology. Organizations such as the American Academy of Professional Coders (AAPC) and the American Health Information Management Association (AHIMA) provide resources, publications, and conferences to help coders stay up to date with emerging trends and coding changes.
Participating in Training Programs
Training programs provide medical coders with the knowledge and skills necessary to excel in their roles. These programs cover fundamental coding principles, coding guidelines, and coding systems. Ongoing training helps coders enhance their coding accuracy, stay informed about new coding practices, and adapt to changes in the healthcare industry.
Pursuing Certifications
Certifications demonstrate a coder’s proficiency and commitment to the profession. Certifying organizations, such as AAPC and AHIMA, offer various coding credentials, such as Certified Professional Coder (CPC) and Certified Coding Specialist (CCS), which validate a coder’s expertise in specific coding specialties. Obtaining certifications enhances career opportunities and provides recognition within the industry.
Coding in Different Healthcare Settings
Medical coders can work in various healthcare settings, each with its unique coding requirements.
Hospital Coding
Hospital coding involves assigning codes to the wide range of services provided in hospital settings, including inpatient, outpatient, and emergency department visits. Hospital coders must have a thorough understanding of complex medical procedures, diagnoses, and treatments. They often specialize in specific areas such as surgery, radiology, or emergency medicine.
Physician Office Coding
Physician office coding focuses on coding services provided in a physician’s office or clinic setting. Coders in this setting primarily handle evaluation and management (E/M) coding, which involves coding patient visits, consultations, and medical history reviews. Attention to detail and accurate documentation review are crucial in this setting.
Specialty Coding
Specialty coding encompasses coding in specialized areas of healthcare, such as mental health, oncology, or cardiology. These areas often have unique coding requirements and guidelines specific to the specialty. Coders specializing in these areas must have in-depth knowledge of the specialty, specialized coding rules, and familiarity with specific coding systems related to their specialization.
Future Trends in Medical Coding
As technology continues to advance, the field of medical coding is experiencing several trends that are shaping its future.

Technological Advancements
Technological advancements are revolutionizing the field of medical coding. Automated coding software and computer-assisted coding (CAC) systems are becoming increasingly prevalent, aiding coders in their code assignment processes. These technologies help accelerate coding while reducing the risk of errors and improving overall coding accuracy.
Telecommuting Opportunities
The field of medical coding offers increasing opportunities for telecommuting or remote work. With the availability of electronic medical record systems and secure communication platforms, coders can effectively work from home or other remote locations. This provides flexibility and work-life balance for coders while still contributing to the healthcare industry.
Artificial Intelligence in Coding
Artificial intelligence (AI) is gradually being integrated into the field of medical coding. AI-powered coding algorithms and natural language processing technologies are being developed to assist coders in accurate code assignment. These advancements have the potential to streamline coding processes, improve accuracy, and reduce the administrative burden on coders.
In summary, medical coding plays a vital role in the healthcare industry, enabling accurate billing, reimbursement, and data analysis. Medical coders are responsible for assigning codes, ensuring accuracy, and complying with coding guidelines. Collaborating with healthcare professionals, they facilitate the revenue cycle process and support proper documentation. By staying updated, pursuing professional development, and adapting to evolving trends, medical coders contribute to the accurate representation of patient care while embracing technological advancements that shape the future of coding.