In the world of healthcare, medical billing companies play a crucial role in ensuring the efficient management of financial transactions for medical services rendered. With a meticulous demeanor and an intricate understanding of medical coding and billing regulations, these companies take charge of the complex process of documenting, submitting, and following up on claims to insurance providers. By meticulously navigating the intricate maze of healthcare regulations and streamlining the billing process, medical billing companies prove to be invaluable partners for medical professionals, facilitating the smooth flow of revenue and enabling healthcare providers to focus on their primary objective of delivering exceptional patient care.
Medical Billing Companies
This image is property of www.ultimatemedical.edu.
Overview
Medical billing companies play a vital role in the healthcare industry by providing services related to medical billing, revenue cycle management, electronic health records, and compliance with regulatory requirements. These companies help healthcare providers streamline their billing processes, ensuring accurate and timely reimbursement for the services they provide. By outsourcing their billing and administrative tasks, healthcare organizations can focus on delivering quality patient care while reducing administrative burden and maximizing revenue.
Role in Healthcare Industry
Medical billing companies act as intermediaries between healthcare providers, insurance companies, and patients. They handle all the necessary paperwork and communication required for the billing and reimbursement process. By navigating the complex landscape of health insurance, coding standards, and regulatory requirements, medical billing companies ensure that healthcare providers receive appropriate compensation for their services.
Services Provided
Medical billing companies offer a wide range of services designed to optimize the revenue cycle and improve overall efficiency. These services include patient registration, verification of insurance, coding and documentation, claim submission, claims review and management, billing and invoicing, payment processing, denial management, financial reporting, electronic health record integration and management, security and privacy, HIPAA compliance, and adherence to medical coding standards.
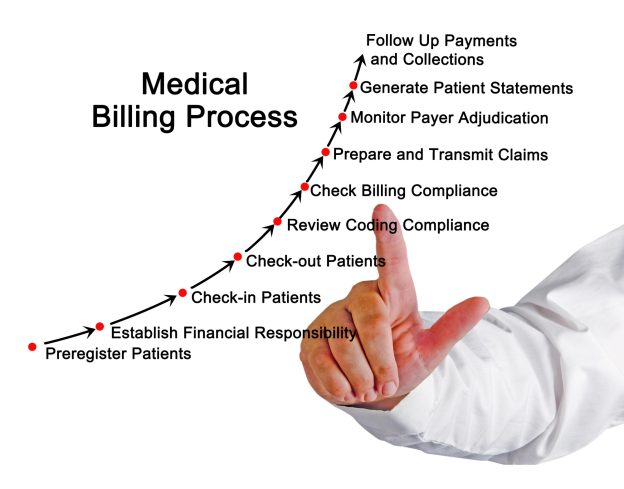
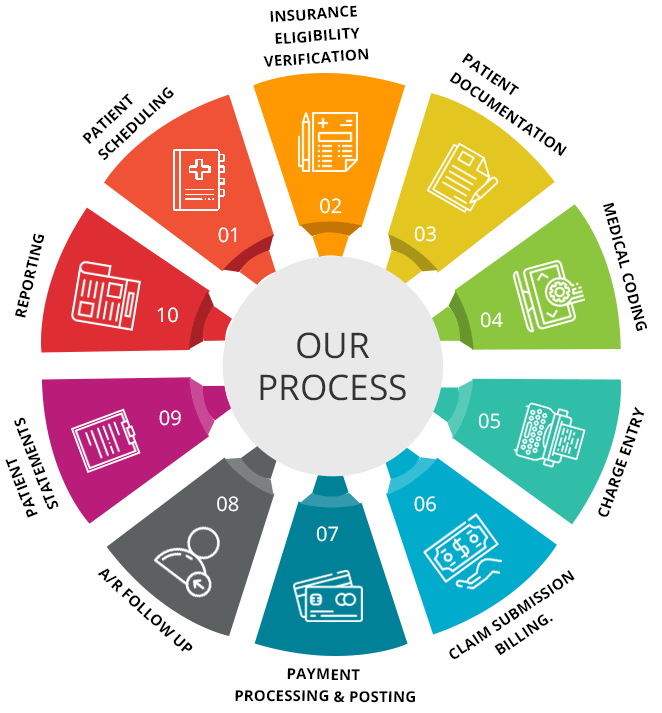
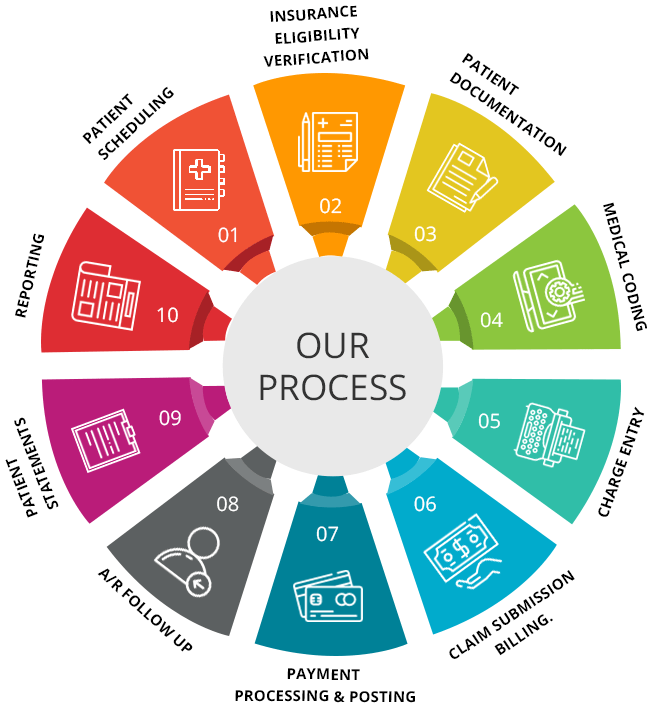
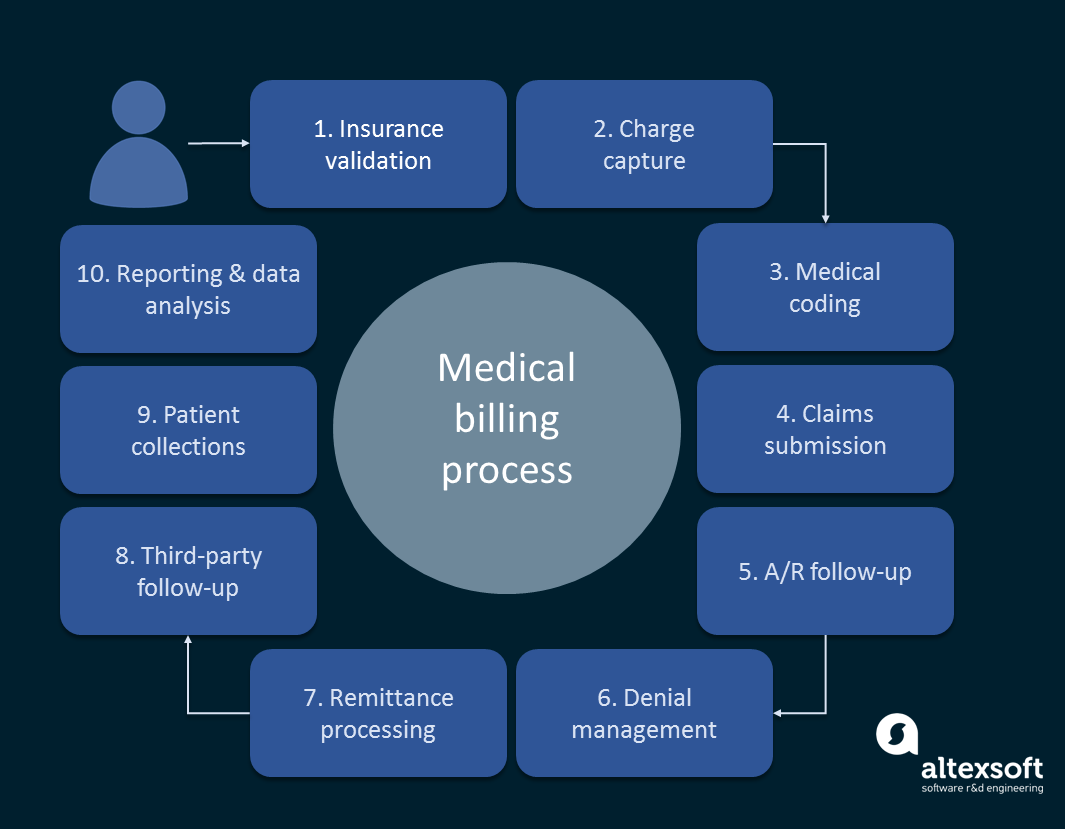
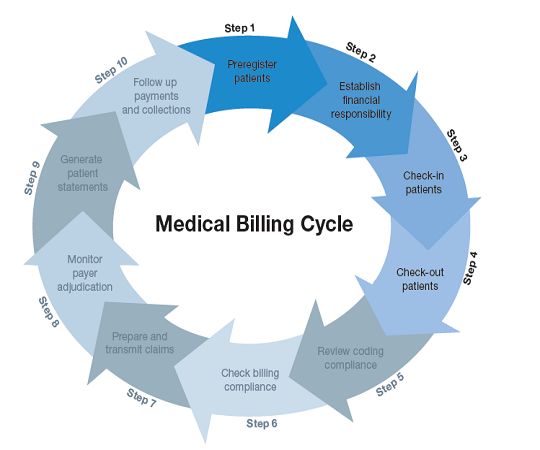
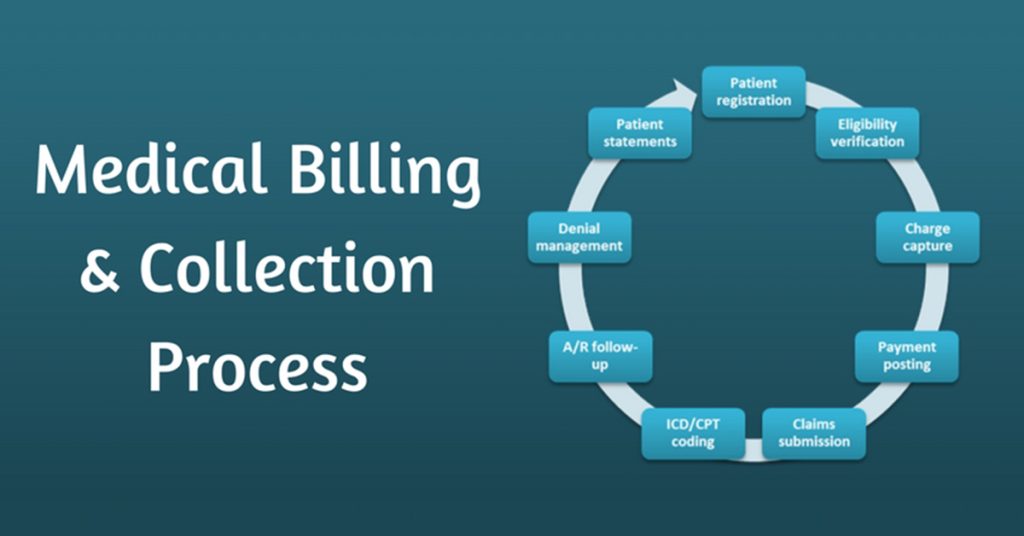
Medical Billing Process
The medical billing process consists of several key steps that medical billing companies guide healthcare providers through:
Patient Registration
At the beginning of the billing process, medical billing companies ensure accurate patient registration. They collect all necessary information from patients, such as personal details, insurance information, and consent forms. This step is crucial for creating a detailed and accurate record of patient demographics, which is essential for proper billing and reimbursement.
Verification of Insurance
The next step involves verifying the provided insurance information. Medical billing companies contact the insurance companies to confirm coverage details, including eligibility, deductibles, co-pays, and pre-authorization requirements. This verification process helps healthcare providers understand the financial responsibility of patients and reduces the risk of claim denials due to inaccurate or insufficient insurance coverage.
Coding and Documentation
Medical billing companies work closely with healthcare providers to ensure proper coding and documentation of medical services. They review medical records and use established coding systems, such as the Current Procedural Terminology (CPT) and the International Classification of Diseases (ICD), to assign appropriate codes to each service rendered. Accurate coding and documentation are crucial for proper reimbursement and compliance.
Claim Submission
Once the coding and documentation are completed, medical billing companies submit claims to insurance companies on behalf of the healthcare providers. They ensure that all required information is included, such as patient demographics, insurance details, provider information, and supporting documentation. Timely and accurate claim submission is essential to expedite the reimbursement process.
Claims Review and Management
After claim submission, medical billing companies track and manage the claims through the review and reimbursement process. They follow up with insurance companies to ensure timely adjudication and resolve any denials or discrepancies. Medical billing companies also handle appeals for denied claims, aiming to maximize reimbursement for healthcare providers. Efficient claims review and management minimize revenue cycle delays and improve cash flow.
Revenue Cycle Management
Medical billing companies play a crucial role in optimizing the revenue cycle of healthcare providers. They employ strategies and processes to maximize revenue generation, reduce payment delay, and manage denials effectively. Key components of revenue cycle management include billing and invoicing, payment processing, denial management, and financial reporting.
Billing and Invoicing
Medical billing companies generate accurate and timely billing statements and invoices on behalf of healthcare providers. They ensure that all services provided are properly documented, coded, and billed according to the applicable fee schedules and contractual agreements. By streamlining the billing process, medical billing companies can reduce billing errors and accelerate the reimbursement cycle.
Payment Processing
Once the claims are submitted, medical billing companies handle the processing of payments from insurance companies and patients. They reconcile the payments received, identify any discrepancies, and ensure that the correct payment amounts are posted to the provider’s accounts. Efficient payment processing improves cash flow and reduces the financial strain on healthcare providers.
Denial Management
Medical billing companies are skilled in managing claim denials and actively work to minimize their impact on revenue. They thoroughly review denial reasons, identify patterns, and implement corrective measures to prevent future denials. By effectively addressing claim denials, medical billing companies improve reimbursement rates and help healthcare providers maintain financial stability.
Financial Reporting
To support informed decision-making and financial planning, medical billing companies provide comprehensive financial reporting. They generate various reports, including revenue analysis, claim status, accounts receivable aging, and reimbursement trends. These reports provide valuable insights into the financial health of healthcare providers and help identify areas for improvement and optimization.
Electronic Health Records
Medical billing companies assist healthcare providers in the integration and management of electronic health records (EHR). EHR systems offer a streamlined and efficient way to store and access patient medical records, including demographics, medical history, prescriptions, and lab results. Medical billing companies ensure the proper integration of EHR systems with billing and coding software, facilitating seamless data transfer and accuracy.
Security and Privacy
Medical billing companies prioritize the security and privacy of patient information. They take extensive measures to ensure compliance with industry standards, such as the Health Insurance Portability and Accountability Act (HIPAA). By implementing robust security protocols, data encryption methods, and access controls, medical billing companies protect sensitive patient data from unauthorized access or breaches.
Compliance and Regulatory Requirements
Medical billing companies navigate the complex landscape of compliance and regulatory requirements, ensuring healthcare providers adhere to industry standards. Two critical aspects of compliance are HIPAA and medical coding standards.
HIPAA Compliance
Medical billing companies ensure that healthcare providers comply with the regulations outlined in the Health Insurance Portability and Accountability Act (HIPAA). They help organizations implement policies and procedures to protect the privacy and security of patients’ protected health information (PHI). By ensuring HIPAA compliance, medical billing companies mitigate the risk of penalties and reputation damage for healthcare providers.
Medical Coding Standards
Accurate and consistent medical coding is essential for effective billing and reimbursement. Medical billing companies adhere to standardized coding systems, such as the Current Procedural Terminology (CPT) and the International Classification of Diseases (ICD). Compliance with medical coding standards ensures that healthcare providers receive appropriate reimbursement and maintain accurate records.
Benefits of Using Medical Billing Companies
Healthcare providers can experience numerous benefits by utilizing the services of medical billing companies.
Efficiency and Accuracy
Medical billing companies are specialized in their field and possess the expertise and resources to streamline billing processes efficiently. They leverage advanced billing software, coding tools, and industry knowledge to ensure accurate coding, quick claim submission, and effective reimbursement management. By outsourcing these tasks, healthcare providers can focus on delivering quality care without the burden of administrative tasks.
Increased Revenue
Medical billing companies have extensive experience in optimizing the revenue cycle for healthcare providers. By minimizing claim denials, reducing payment delays, and improving billing accuracy, these companies help maximize revenue generation. With their expertise, healthcare providers can optimize financial performance and ensure a steady cash flow.
Reduced Administrative Burden
Outsourcing billing and administrative tasks to medical billing companies helps healthcare providers reduce their administrative burden significantly. These companies handle all aspects of the billing process, including patient registration, insurance verification, claim submission, and denial management. By freeing up valuable time and resources, healthcare providers can focus on patient care and strategic initiatives.
Considerations when Choosing a Medical Billing Company
When selecting a medical billing company, healthcare providers should consider several factors to ensure a successful partnership:
Experience and Expertise
The experience and expertise of a medical billing company are key considerations. Healthcare providers should explore the company’s track record, industry reputation, and client testimonials. Assessing the company’s expertise in specific medical specialties or billing systems can help determine the suitability for their specific needs.
Cost and Pricing
Understanding the pricing structure and cost implications is crucial when selecting a medical billing company. Providers should evaluate whether the company charges a flat fee, a percentage of collections, or a combination. They should also consider any additional fees for services such as software licensing, integration, or support. Balancing cost considerations with the expected return on investment is essential.
Technology and Integration
Assessing the technological capabilities and compatibility of a medical billing company is vital. Providers should evaluate the company’s billing software, coding tools, and EHR integration capabilities. Integration with existing systems and workflow is essential to ensure seamless data exchange and minimize disruptions.
Customer Support
Responsive and reliable customer support is critical in the partnership with a medical billing company. Providers should inquire about the company’s customer support channels, response times, and availability. Effective communication and support ensure a smooth billing process and prompt resolution of any issues that may arise.
Challenges Faced by Medical Billing Companies
Medical billing companies face various challenges in the ever-evolving healthcare landscape. Some of the significant challenges include:
Changing Regulations
The healthcare industry is subject to frequent regulatory changes, making it challenging for medical billing companies to stay updated and compliant. Regulatory changes in coding standards, billing requirements, and reimbursement policies can impact revenue cycles and necessitate continuous adaptation.
Insurance Reimbursement Issues
Insurance companies frequently update their policies, coverage criteria, and reimbursement rates. Medical billing companies must stay informed about these changes to ensure accurate claim submission and reimbursement. Negotiating with insurance companies to optimize reimbursement rates can be an ongoing challenge for medical billing companies.
Data Security Risks
As medical billing processes increasingly rely on electronic systems and data exchange, data security risks are a significant concern. Medical billing companies must employ robust security measures, training programs, and audits to prevent data breaches and protect patient information effectively. The ever-evolving landscape of cybersecurity threats requires ongoing vigilance.
High Staff Turnover
Medical billing companies often experience high staff turnover due to the demanding and complex nature of their work. New hires require training and onboarding, which can impact efficiency and continuity in billing processes. Companies with robust training programs and effective employee retention strategies mitigate this challenge.
Future Trends in Medical Billing
Looking ahead, medical billing is poised for evolution and advancement. Emerging trends are set to shape the industry’s future:
Automation and Artificial Intelligence
Automation and artificial intelligence (AI) have the potential to revolutionize medical billing processes. AI-powered software can streamline data entry, coding, claim submission, and denial management, reducing errors and improving efficiency. Automation can free up valuable resources and enable medical billing companies to focus on value-added tasks.
Telemedicine and Remote Billing
The rise of telemedicine and remote healthcare services has opened new opportunities for medical billing companies. These companies are adapting to the unique billing requirements of telemedicine, such as remote patient consultations and virtual care delivery. As telemedicine continues to grow, medical billing companies will play a crucial role in ensuring accurate and timely reimbursement for these services.
Conclusion
Medical billing companies play a crucial role in the healthcare industry, providing services that optimize revenue cycles, streamline billing processes, and ensure compliance with regulatory requirements. By outsourcing billing and administrative tasks, healthcare providers can focus on delivering quality patient care while maximizing revenue and reducing administrative burden. With the ever-evolving landscape of healthcare and emerging trends like automation and telemedicine, medical billing companies will continue to play a vital role in the future of healthcare reimbursement.

This image is property of statimllc.com.