When faced with the challenging task of disputing medical billing, it is essential to have a comprehensive understanding of the most effective approach. In this article, we will explore the most advantageous strategies for disputing medical bills, offering valuable insights into the importance of thorough documentation, effective communication with healthcare providers, and the potential benefits of seeking professional assistance. By equipping yourself with this knowledge, you will be better equipped to navigate the often complex and confusing landscape of medical billing disputes, ensuring your rights are protected and your financial well-being preserved.
Understanding the Medical Billing Process
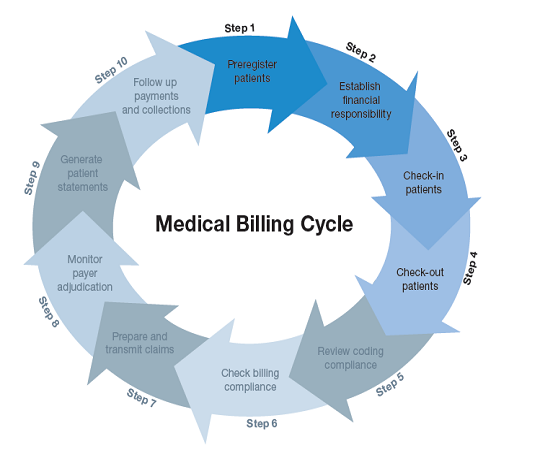
Getting familiar with the medical billing process is essential to effectively dispute any errors or discrepancies in your medical bills. The process begins with understanding medical billing codes, which are alphanumeric codes used to classify medical procedures and services. These codes help healthcare providers and insurance companies accurately determine the cost of services rendered.
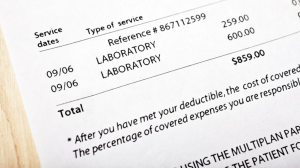
Reviewing the Explanation of Benefits (EOB) is another crucial step in understanding medical billing. The EOB is a document sent by your insurance company that outlines the services provided, the amount charged, and the portion covered by insurance. Carefully reviewing the EOB allows you to ensure that the charges and services listed are accurate and align with the treatment you received.
Verifying services and charges is an important aspect of understanding medical billing. It involves comparing the itemized bill provided by your healthcare provider with the services documented in your medical records. This step helps identify any discrepancies or services that were not rendered, which could potentially lead to inaccurate charges.
Understanding your insurance coverage is vital for navigating the medical billing process. Familiarize yourself with the terms of your insurance policy, such as deductibles, co-pays, and out-of-pocket limits. Knowing what your insurance covers will empower you to identify any inaccuracies or denied claims, as well as ensure you receive the benefits you are entitled to.
Identifying Billing Errors
To effectively dispute medical billing, it is crucial to identify any errors that may be present in the billing statements. Comparing the medical bill with the Explanation of Benefits (EOB) is a fundamental step in this process. By cross-referencing the two documents, you can ensure that the charges listed on the bill match the services and costs authorized by your insurance company.
Checking for duplicate charges is another important aspect of identifying billing errors. Inaccurate duplicates can appear on your bill due to administrative errors or technical glitches. By carefully reviewing each itemized charge, you can identify any duplicated services or charges that need to be corrected.
Confirming correct coding is essential to prevent billing errors. Medical billing codes play a crucial role in determining the cost of medical services. Ensure that the billing codes used align with the services you received and that they accurately reflect the complexity and extent of your treatment.
Validating the accuracy of personal information is imperative when reviewing medical bills. Ensuring that your personal details, such as name, address, and insurance information, are correctly listed on the bill reduces the risk of billing errors and helps facilitate the resolution process.
Gathering Relevant Information
To effectively dispute medical billing, it is essential to gather all relevant information regarding your medical treatment and associated charges. Obtaining copies of your medical records is a crucial step in this process. These records provide detailed documentation of the services you received, allowing you to cross-reference them with the itemized bill and identify any discrepancies.
Retrieving itemized bills from your healthcare provider is vital for understanding the breakdown of charges. An itemized bill provides a detailed list of each service rendered along with the corresponding costs. This detailed information is essential for verifying the accuracy of charges and identifying any potential errors.
Collecting supporting documentation is necessary to strengthen your case when disputing medical billing. This may include receipts, letters, or other relevant documents that provide additional evidence or clarification. By gathering and organizing all the necessary paperwork, you can present a comprehensive case when disputing any billing errors.
Organizing all the necessary paperwork is crucial to ensure that you have a clear and comprehensive record of the issues you are disputing. By keeping all relevant documents in one place, such as a binder or digital folder, you can easily access and reference them throughout the dispute resolution process.
Contacting the Healthcare Provider
When disputing medical billing, it is important to maintain open and professional communication with the billing department of your healthcare provider. Speaking directly with the billing department allows you to explain your concerns and inquire about any confusing charges or billing errors.
Requesting an itemized bill from the healthcare provider is essential for obtaining a comprehensive breakdown of charges. By requesting this detailed bill, you can ensure that each service and corresponding cost is clearly and accurately documented, making it easier to identify any errors or discrepancies.
During your communication with the healthcare provider, clarifying any confusing charges is crucial in order to fully understand the services rendered and the associated costs. If any charges do not seem clear or if you have questions about specific services, don’t hesitate to ask for further explanation or clarification.
Addressing possible billing errors in a professional manner is important when contacting the healthcare provider. Clearly and calmly express your concerns and provide any evidence or documentation that supports your claim. By doing so, you demonstrate that you are actively engaged in resolving the issue and seeking a fair resolution.
Contacting the Insurance Company
In addition to contacting the healthcare provider, it is necessary to reach out to your insurance company when disputing medical billing. Contact the insurance provider’s customer service department and clearly explain your concerns regarding specific charges or claims.
Confirming coverage and benefits is an important step when contacting the insurance company. By verifying your policy details, such as deductibles, co-pays, and coverage limits, you can ensure that you are eligible for the benefits claimed by your healthcare provider. Understanding your insurance coverage will help you identify any potential inconsistencies or errors in the billing process.
Inquiring about denied claims is crucial when contacting the insurance company. If any of your claims have been denied, ask for an explanation and the specific reason for the denial. This information will help you understand the insurance company’s perspective and allow you to address any underlying issues during the dispute resolution process.
Appealing claim denials is an option to consider if your insurance company denies coverage for certain services. Familiarize yourself with the appeals process outlined by your insurance company and gather any relevant supporting documentation or medical records to strengthen your case. By appealing a denial, you increase your chances of receiving the coverage you are entitled to.
Writing a Formal Dispute Letter

If initial communication with the healthcare provider and insurance company does not resolve the billing dispute, writing a formal dispute letter can be an effective method to escalate the issue. When writing the letter, maintain a professional tone and clearly state the issue you are disputing.
Clearly stating the issue in the dispute letter will help ensure that your concerns are properly addressed. Provide a concise and detailed explanation of the specific charges or services you are disputing, including any relevant dates and reference numbers. By clearly outlining the issue, you increase the chances of a prompt and accurate resolution.
Including relevant details and dates is important when writing a dispute letter. Be specific about any supporting documentation you have included and clearly reference any previous communication or attempts to resolve the issue. Providing a clear timeline and all relevant information will assist the recipient in understanding the nature and severity of the dispute.
Requesting a prompt resolution is essential when writing a dispute letter. Clearly state your expectations and deadline for a response or resolution. By setting clear expectations, you demonstrate that you are serious about resolving the issue and expect a timely and satisfactory outcome.
Submitting the Dispute
Submitting the dispute letter to the correct address is crucial to ensure that it reaches the appropriate party. Double-check the contact information for the healthcare provider or insurance company and follow any specific instructions provided. Ensuring the dispute letter is delivered to the correct address reduces the likelihood of delays in the resolution process.
Using certified mail or online methods to submit the dispute provides a level of tracking and confirmation. Certified mail allows you to receive proof of delivery, which can be beneficial if legal action becomes necessary. Many healthcare providers and insurance companies also offer online dispute submission options, allowing for efficient and timely communication.
Tracking the delivery of the dispute is important to ensure that it reaches its intended recipient. Keep a record of the tracking number, delivery date, and any related updates. This information can be useful if follow-up is required or if there is a need to escalate the dispute.
Keeping a copy of the dispute letter for personal records is essential for your own reference. Make sure to retain a copy of the letter, any supporting documentation, and proof of delivery. This will serve as a record of the dispute and any actions taken, should you need to refer to it in the future.
Following Up on the Dispute
After submitting the dispute, it is important to follow up to ensure that the process is progressing and that your concerns are being addressed. Contact the healthcare provider to confirm that they have received your dispute letter and are investigating the matter.
Requesting updates on the investigation is crucial to stay informed about the progress of the dispute. Regularly reach out to the appropriate department or contact provided to inquire about any updates or findings. By maintaining active communication, you demonstrate your commitment to resolving the issue.
Maintaining regular communication with the healthcare provider or insurance company is important throughout the dispute resolution process. Regularly check in to ensure that your concerns are not forgotten, and to provide any additional information or documentation that may be requested. By actively participating, you increase the likelihood of a more accurate and timely resolution.
Escalating the complaint, if necessary, may be required if the dispute fails to progress or is not resolved to your satisfaction. This could involve contacting a supervisor or manager within the healthcare provider or insurance company. Consider the severity of the issue and the potential impact on your financial or personal well-being before escalating further.
Considering Mediation or Arbitration
If the dispute remains unresolved, considering mediation or arbitration as alternative dispute resolution methods may be beneficial. Mediation involves a neutral third party who helps facilitate communication and negotiation between you and the healthcare provider or insurance company. Arbitration involves a third-party decision-maker who listens to both parties’ arguments and makes a binding decision.
Researching mediation services in your area or provided by your insurance company is a good starting point. Look for mediators who specialize in healthcare disputes or have experience with medical billing issues. Mediation can be a less adversarial and more cost-effective way to reach a resolution without going to court.
Contacting the appropriate arbitration organization is essential if you choose to pursue arbitration. Organizations such as the American Arbitration Association can provide information on the arbitration process and connect you with a qualified arbitrator. Understand the fees and procedures associated with arbitration before proceeding.
Understanding the benefits and limitations of mediation or arbitration is crucial. These methods can provide a faster resolution and potentially avoid the need for legal action. However, the decisions reached through mediation or arbitration are binding and may not always favor your position. Carefully weigh the pros and cons before pursuing this avenue.
Seeking Legal Assistance

If all attempts to resolve the dispute have been unsuccessful, seeking legal assistance may be necessary. Consulting with a healthcare attorney specialized in medical billing disputes can provide valuable guidance and advice. They can explain your legal rights and options based on your specific circumstances.
Understanding legal rights and options is essential when considering involving legal professionals. A healthcare attorney can educate you on your rights as a patient and the legal recourse available to address your billing concerns. Being informed will enable you to make well-informed decisions regarding legal action.
Knowing when to involve legal professionals is a crucial decision that should be based on the complexity and severity of your dispute. If the medical billing issue involves significant amounts of money, potential damage to your credit, or unresolved administrative errors, consulting with an attorney can help navigate the legal process and protect your interests.
Considering the costs and potential outcomes of legal assistance is important before proceeding. Legal representation can be expensive, and the outcome of litigation is not guaranteed. Weigh the potential costs, benefits, and risks associated with legal action before making a final decision.
In conclusion, effectively disputing medical billing requires understanding the medical billing process, identifying billing errors, gathering relevant information, contacting the healthcare provider and insurance company, writing a formal dispute letter, submitting the dispute, following up on the dispute, considering alternative dispute resolution methods, and seeking legal assistance when necessary. By following these steps and maintaining a professional approach, you can increase the likelihood of successfully resolving any medical billing issues and obtaining a fair and accurate resolution.