In the realm of healthcare administration, it is crucial to understand the intricacies of medical billing. By comprehending the various types of medical billing, professionals can effectively manage and process financial transactions within the healthcare industry. This article seeks to shed light on the different types of medical billing, including fee-for-service, capitation, and resource-based relative value scale (RBRVS). Whether you are a healthcare provider, administrator, or simply curious about the field, this comprehensive exploration will equip you with the necessary knowledge to navigate the complex world of medical billing.

This image is property of rightmedicalbilling.com.
Types of Medical Billing
Medical billing is an essential component of the healthcare industry, ensuring that healthcare providers receive proper payment for the services they provide. With advancements in technology and changes in healthcare regulations, various types of medical billing have emerged to meet the ever-evolving needs of healthcare organizations. This article will explore and discuss the different types of medical billing, including traditional medical billing, electronic medical billing, outsourced medical billing, in-house medical billing, centralized medical billing, decentralized medical billing, fee-for-service medical billing, value-based medical billing, global medical billing, and professional medical billing.
Traditional Medical Billing
Medical cost concept with stethoscope and medical bill
Traditional medical billing refers to the conventional method of processing healthcare claims and billing patients and insurance companies for services rendered. It involves the use of paper-based documents and manual data entry to generate and submit claims for reimbursement.
Process
In traditional medical billing, healthcare providers gather patient information, including demographic details, insurance coverage, and the services provided. This data is then manually entered into paper forms, which include the necessary codes for the services rendered. The completed forms, along with supporting documentation, are submitted to the insurance company for claim processing.
Advantages
One advantage of traditional medical billing is that it allows for a more personalized approach, as it involves direct interaction with patients and insurance companies. It also provides a physical record of the billing process, which can be useful in case of any disputes or audits.
Disadvantages
However, traditional medical billing is a labor-intensive process that requires significant administrative work and can be prone to errors. The manual data entry and paper-based approach also result in longer processing times, potentially delaying reimbursements for healthcare providers.
Electronic Medical Billing

Electronic medical billing, also known as electronic claims processing, involves the use of electronic systems to create, submit, and process healthcare claims. It utilizes electronic health records (EHR) and designated software programs to streamline the billing process.
Process
With electronic medical billing, healthcare providers capture patient information electronically and input it into their EHR system. The software generates electronic claims based on the services provided and submits them electronically to insurance companies for processing. This automated process eliminates the need for paper-based documents and reduces manual data entry.
Advantages
Electronic medical billing offers numerous advantages, including increased accuracy and efficiency. It reduces errors caused by manual data entry, resulting in fewer claim rejections and denials. The electronic submission also expedites claim processing, leading to faster reimbursement for healthcare providers.
Disadvantages
However, the implementation of electronic medical billing requires an initial investment in software and staff training. Additionally, there may be interoperability challenges when integrating different EHR systems, which can hinder the seamless exchange of information between healthcare providers and insurance companies.
Outsourced Medical Billing

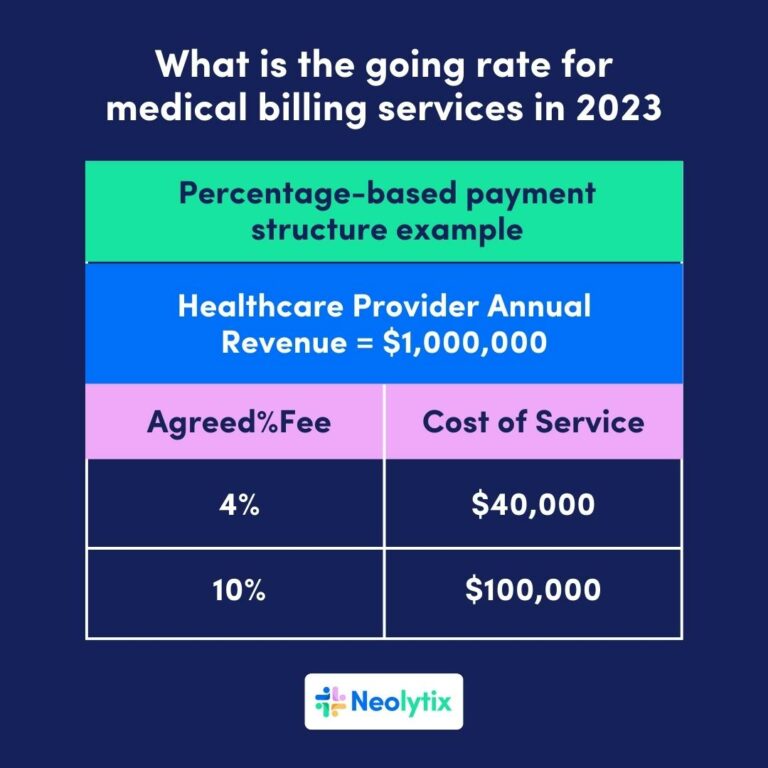
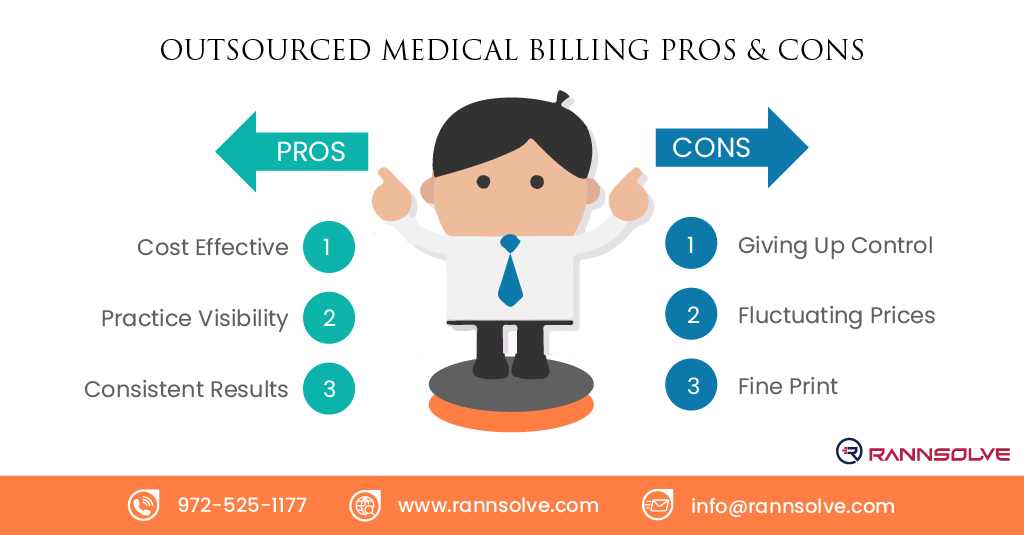
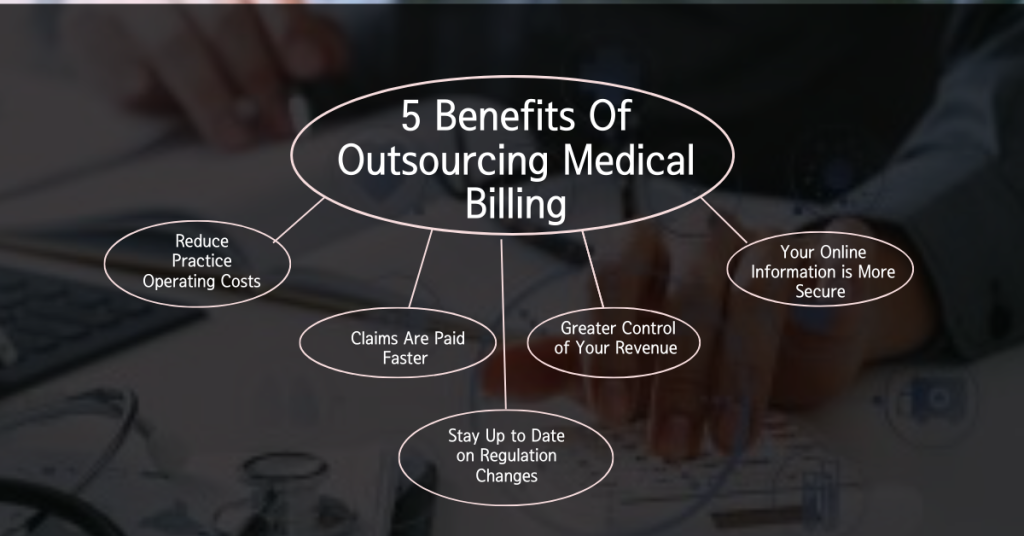
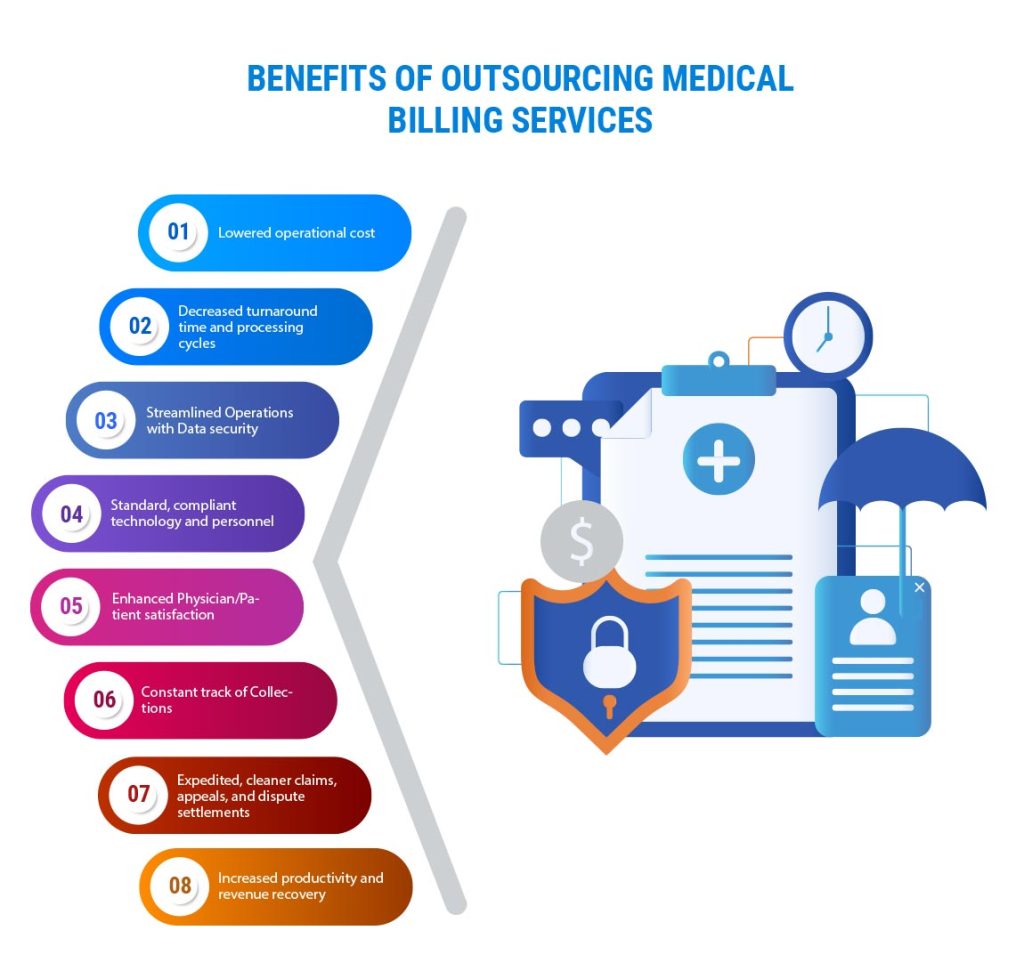
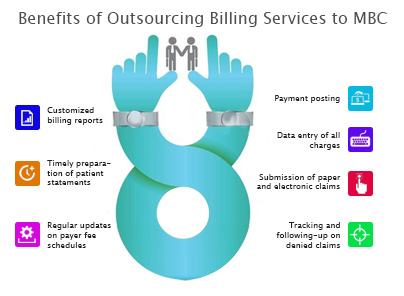
outsourced medical billing involves partnering with a third-party billing company to handle the billing and collections process on behalf of healthcare providers. This type of medical billing allows healthcare organizations to focus on patient care while outsourcing the administrative tasks associated with billing.
Process
In outsourced medical billing, healthcare providers share necessary patient and service information with the third-party billing company. The billing company then takes responsibility for claim generation, submission, and follow-up with insurance companies. They also handle patient billing and collections on behalf of the healthcare provider.
Advantages
outsourcing medical billing offers several advantages, particularly for smaller healthcare practices. It relieves healthcare providers of the administrative burden and allows them to concentrate on patient care. Additionally, outsourcing provides access to specialized billing expertise, reducing the risk of billing errors and maximizing revenue potential.
Disadvantages
However, one potential disadvantage of outsourced medical billing is the loss of direct control over the billing process. Communication and coordination between the healthcare provider and the billing company are crucial to ensure accurate and timely billing. Additionally, there may be concerns about the security and confidentiality of patient information when outsourcing billing functions.

This image is property of www.pharmaknowledgecentre.com.
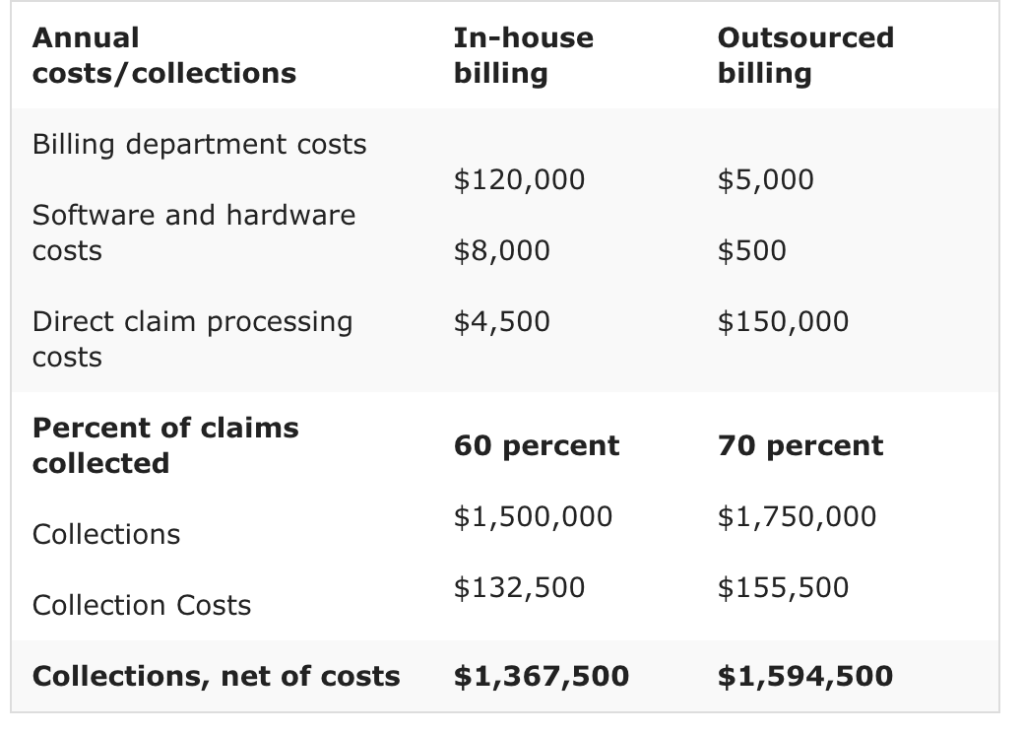
In-House Medical Billing
In-house medical billing refers to the healthcare provider’s decision to manage the entire billing process internally, utilizing their own staff and resources. It involves the establishment of a dedicated billing department within the healthcare organization.
Process
In in-house medical billing, healthcare providers create and maintain their own billing infrastructure, including personnel, software systems, and equipment. This allows them to directly handle all aspects of the billing process, from claim generation to submission and follow-up.
Advantages
One advantage of in-house medical billing is the ability to have complete control over the billing process. The healthcare provider can tailor the process to their specific needs and maintain tight supervision over billing operations. In-house billing also provides the opportunity for direct communication with patients and insurance companies, facilitating prompt resolution of billing issues.
Disadvantages
However, in-house medical billing requires significant investment in infrastructure, including staff training and software systems. The healthcare provider must constantly stay updated on changing billing regulations and industry standards to ensure compliance. Additionally, managing the billing process internally may divert resources and attention from core patient care activities.
Centralized Medical Billing
centralized medical billing involves consolidating the billing functions of multiple healthcare facilities or departments into a single centralized billing department. It streamlines and standardizes the billing process across the organization, promoting efficiency and consistency.
Process
With centralized medical billing, healthcare facilities or departments within an organization pool their billing operations into a central department. This allows for centralized management of billing personnel, software systems, and resources. The central billing department handles the generation, submission, and follow-up of claims, ensuring consistent processes and procedures across the organization.
Advantages
Centralized medical billing offers several advantages, including improved coordination and standardization. It eliminates redundant tasks and promotes efficient use of resources by consolidating billing operations. Centralization also enhances data analysis capabilities and allows for centralized oversight and control of the billing process.
Disadvantages
However, implementing centralized medical billing may face resistance from individual healthcare facilities or departments that are used to maintaining control over their billing operations. Transitioning to a centralized system requires effective communication and buy-in from all stakeholders. Additionally, any interruptions or technical issues in the central billing department can impact the entire organization’s billing process.
Decentralized Medical Billing
Decentralized medical billing, also known as departmental billing, involves assigning billing responsibilities to individual departments or healthcare facilities within an organization. Each department manages its own billing operations independently.
Process
In decentralized medical billing, each healthcare facility or department within an organization is responsible for its billing processes. This includes claim generation, submission, and follow-up, as well as patient billing and collections. The decentralized approach allows each department to tailor its billing operations to specific needs and priorities.
Advantages
Decentralized medical billing provides individual departments with greater control over their billing processes and allows for flexibility in adapting to specific departmental requirements. It promotes accountability and ownership within each department, potentially leading to increased efficiency and productivity.
Disadvantages
However, decentralized medical billing may result in inconsistencies and variations in billing practices across departments within an organization. It can lead to duplication of efforts and inefficient resource utilization. Coordinating billing operations and standardizing processes across decentralized departments can be challenging, requiring strong communication and oversight.
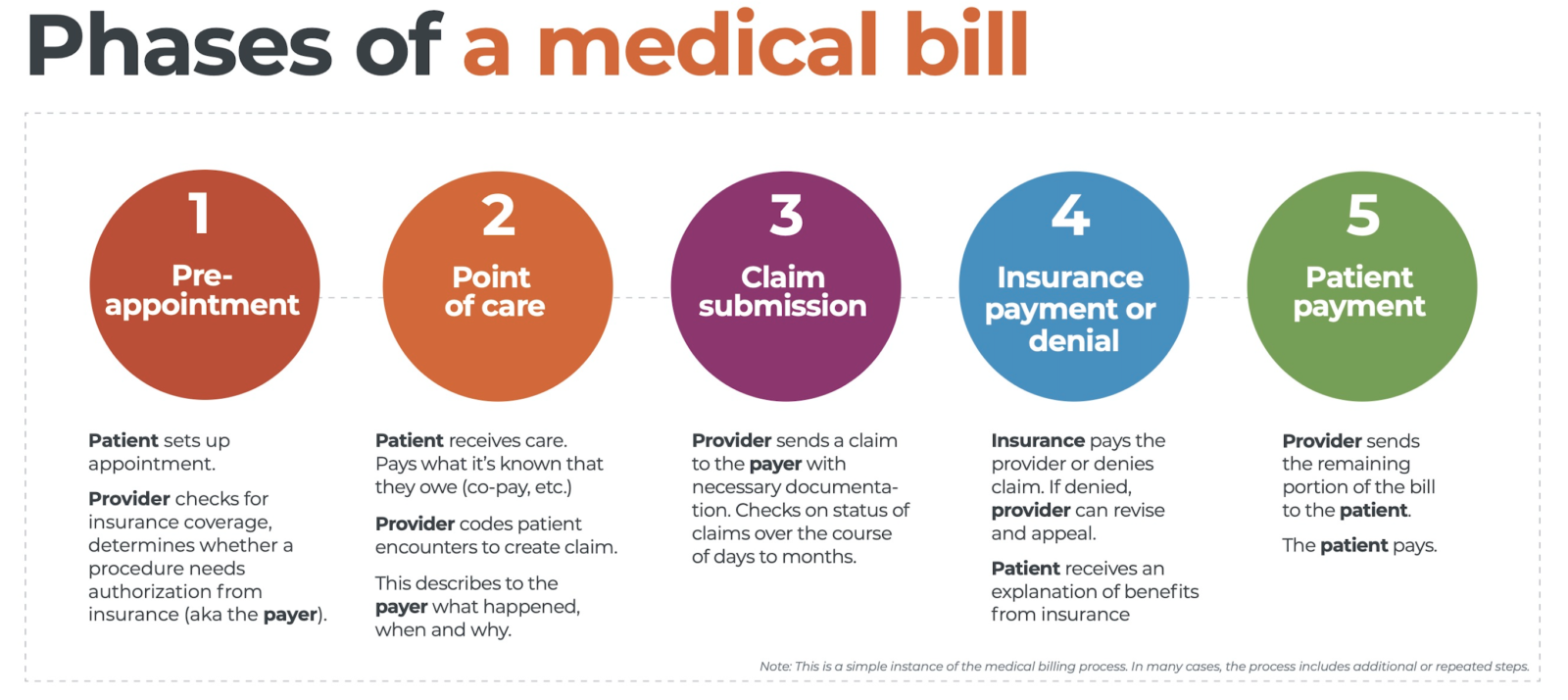
Fee-for-Service Medical Billing
fee-for-service medical billing, also known as traditional or volume-based billing, is a reimbursement model based on charging fees for individual medical services rendered. Healthcare providers bill insurance companies or patients for each specific service or procedure performed.
Process
In fee-for-service medical billing, each service or procedure performed by the healthcare provider is assigned a specific billing code, such as Current Procedural Terminology (CPT) codes. These codes indicate the type of service provided and the associated fee. Claims are generated based on the services rendered and submitted to insurance companies or patients for reimbursement.
Advantages
One advantage of fee-for-service medical billing is that it offers transparency in terms of costs and fees associated with specific services. It allows patients to understand the breakdown of charges, aiding in informed decision-making. Additionally, healthcare providers have the potential to maximize revenue by billing for each service rendered.
Disadvantages
However, fee-for-service medical billing can lead to fragmented care and overutilization of services as healthcare providers may focus on quantity rather than quality of care to maximize revenue. This reimbursement model may also result in higher healthcare costs for patients and increased administrative complexity due to the need for extensive coding and documentation.

This image is property of www.ucontrolbilling.com.
Value-Based Medical Billing
Value-based medical billing, also known as outcome-based or performance-based billing, is a reimbursement model based on the quality and effectiveness of healthcare services provided. It focuses on rewarding healthcare providers for delivering high-quality care and achieving positive patient outcomes.
Process
In value-based medical billing, healthcare providers are reimbursed based on the value and impact of their services rather than the quantity. This includes measuring outcomes, such as patient satisfaction, reduced readmissions, and improved health outcomes. The reimbursement can be tied to performance metrics and predetermined quality goals.
Advantages
Value-based medical billing promotes a patient-centric approach to healthcare by incentivizing healthcare providers to prioritize quality care and patient outcomes. It encourages coordination and collaboration among healthcare professionals to deliver coordinated, efficient care. Additionally, value-based billing can lead to cost savings by avoiding unnecessary or redundant services.
Disadvantages
However, value-based medical billing brings challenges in measuring and assessing the value and impact of healthcare services accurately. The implementation and coordination of performance metrics and quality goals can be complex and require robust data analytics capabilities. Transitioning from traditional fee-for-service models to value-based billing also requires collaboration and acceptance from all stakeholders in the healthcare ecosystem.
Global Medical Billing
Global medical billing refers to the billing and reimbursement processes involved in healthcare services provided across international borders. It encompasses the complex financial transactions and claim submissions associated with medical tourism and cross-border healthcare.
Process
In global medical billing, patients travel to another country to receive medical treatment, often due to cost savings, better access to specialized care, or reduced waiting times. The healthcare provider in the destination country generates and submits claims to the patient’s insurance company or directly bills the patient. It involves coordination between healthcare providers, insurance companies, and international medical billing specialists.
Advantages
Global medical billing provides patients with access to quality healthcare services that may not be available or affordable in their home country. It promotes medical tourism, contributing to the economic growth of destination countries. Healthcare providers in destination countries can also benefit from increased patient volume and revenue.
Disadvantages
However, global medical billing involves navigating complex international regulations, insurance networks, and currency conversions. It requires strong coordination and communication among all parties involved to ensure accurate claim submissions and timely reimbursements. There may also be challenges in maintaining continuity of care and medical records across borders.
Professional Medical Billing
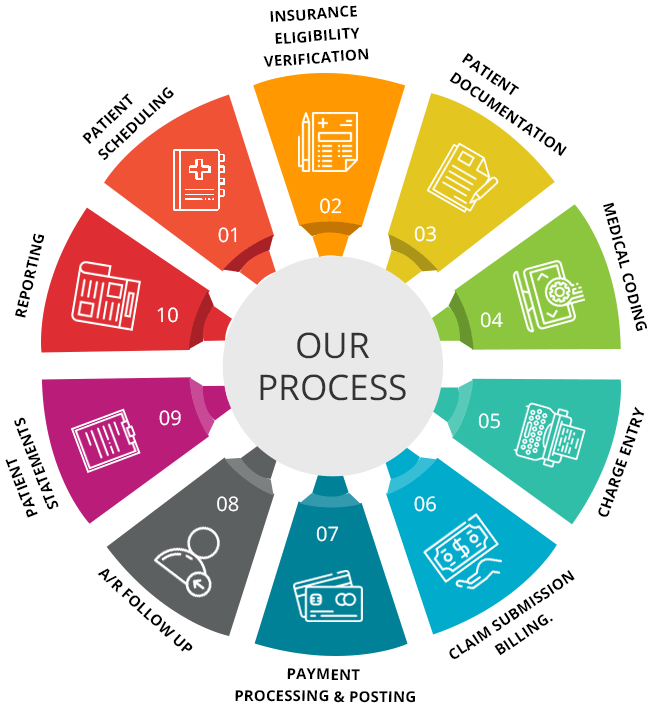
Professional medical billing involves the use of dedicated medical billing professionals or companies to handle the billing and collections process for healthcare providers. These professionals have specialized knowledge and expertise in medical billing regulations and coding.
Process
In professional medical billing, healthcare providers outsource their billing functions to professional billing companies or hire certified medical billers. These professionals handle the entire billing process, including claim generation, submission, follow-up, and patient billing and collections. They stay updated on the latest billing regulations and coding changes to ensure accurate and compliant billing practices.
Advantages
Professional medical billing offers the advantage of specialized knowledge and expertise in medical billing. Certified medical billers are trained in coding, billing regulations, and insurance practices, reducing the risk of errors and denials. Outsourcing billing to professionals also allows healthcare providers to focus on patient care and frees up resources that would otherwise be dedicated to billing operations.
Disadvantages
However, healthcare providers must carefully select and partner with reputable professional billing companies or employ certified medical billers. The cost of outsourcing or hiring professionals may also be a factor to consider. Effective communication and collaboration between the healthcare provider and the professional billing entity are vital to ensure accurate and timely billing, as well as resolution of any billing-related issues.
In conclusion, the landscape of medical billing has evolved significantly in recent years, with various types of medical billing emerging to meet the diverse needs of healthcare organizations. Traditional medical billing, electronic medical billing, outsourced medical billing, in-house medical billing, centralized medical billing, decentralized medical billing, fee-for-service medical billing, value-based medical billing, global medical billing, and professional medical billing all offer unique approaches and considerations. Understanding the different types of medical billing can help healthcare providers make informed decisions to optimize their billing processes and ultimately improve financial outcomes.