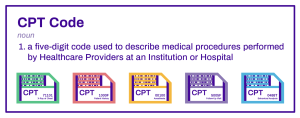
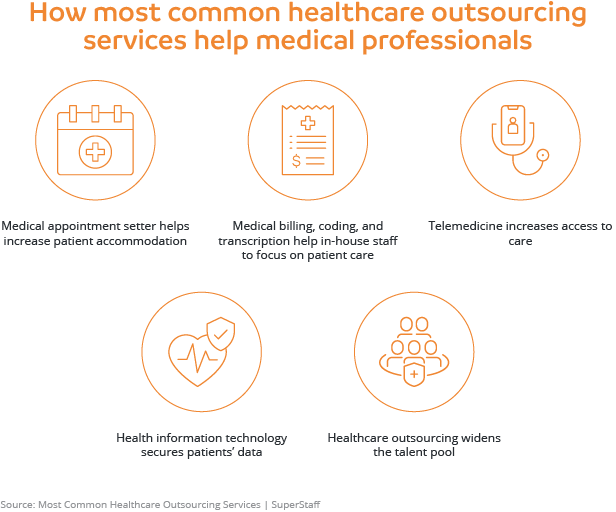
Medical coding is a vital component of the healthcare industry, playing a crucial role in ensuring accurate billing and reimbursement for services rendered. From assigning standardized codes to medical diagnoses, procedures, and treatments, to billing and documentation purposes, medical coding is a language of its own. This article aims to shed light on a few examples of medical coding, highlighting the various code sets used in the field, such as ICD-10, CPT, and HCPCS, and exploring how these codes aid in translating complex medical information into a concise and universally understood format. Whether you’re a healthcare professional seeking to enhance your coding knowledge or a patient interested in understanding how your medical records are documented and analyzed, this article will provide you with valuable insight into the world of medical coding and its significance in the realm of healthcare.
Evaluation and Management Codes
Evaluation and Management (E/M) codes are used in medical billing and coding to describe the level of complexity and time involved in providing patient care during office or other outpatient visits. These codes are crucial for healthcare providers as they determine the appropriate reimbursement for their services.
Under the category of E/M codes, there are subcategories that define specific services provided during different types of patient encounters. One such subcategory is for office or other outpatient services. This includes routine check-ups, consultations, and follow-up visits with healthcare providers in a non-hospital setting. The E/M codes for these services range from basic to complex, reflecting the complexity of the medical decision-making involved and the time spent with the patient.
Another subcategory of E/M codes is for hospital observation services. In this case, the patient requires a period of observation in a hospital setting but does not meet the criteria for inpatient admission. The E/M codes for hospital observation services consider factors such as the level of medical decision-making, the complexity of the patient’s condition, and the time spent providing care.
Finally, emergency department services also have their own set of E/M codes. These codes are used to describe the evaluation and management of patients in an emergency department setting. The codes take into account the severity of the patient’s condition, the complexity of the medical decision-making, and the level of care provided by the emergency healthcare team.
Surgical Codes
Surgical codes are used to describe different types of surgical procedures performed by healthcare providers. Each surgical code corresponds to a specific procedure, enabling accurate documentation and billing for the services rendered. The codes also capture important details such as the complexity of the surgery, the body area involved, and any additional procedures performed during the surgery.
Some examples of surgical codes include those for biopsies, endoscopies, and cataract surgery. A biopsy is a procedure where a sample of tissue is extracted for examination and diagnosis. Endoscopies, on the other hand, involve the use of a flexible tube with a camera to visualize and treat certain conditions in the body, such as gastrointestinal issues. Lastly, cataract surgery is the surgical removal and replacement of a clouded lens in the eye.
By using specific surgical codes, healthcare providers and insurance companies can ensure accurate billing and reimbursement for surgical procedures, as well as maintain patient records for future reference.
Anesthesia Codes
Anesthesia codes are used to document and bill for the administration of anesthesia during medical procedures. Anesthesia is essential to ensuring patient comfort and safety during surgeries and other invasive procedures. These codes capture the type, complexity, and length of anesthesia provided.
There are different types of anesthesia codes, including those for general anesthesia, regional anesthesia, and monitored anesthesia care (MAC). General anesthesia involves inducing a controlled state of unconsciousness to eliminate pain and awareness during surgery. Regional anesthesia, on the other hand, blocks sensation in a specific region of the body, such as a limb or the lower half of the body. MAC refers to the administration of anesthesia while the patient is conscious, but sedated, during certain procedures.
Anesthesia codes help healthcare providers accurately document the type and extent of anesthesia provided, allowing for appropriate reimbursement and record-keeping. These codes also play a crucial role in patient safety by providing a standardized way of tracking and assessing anesthesia administration.
Radiology Codes
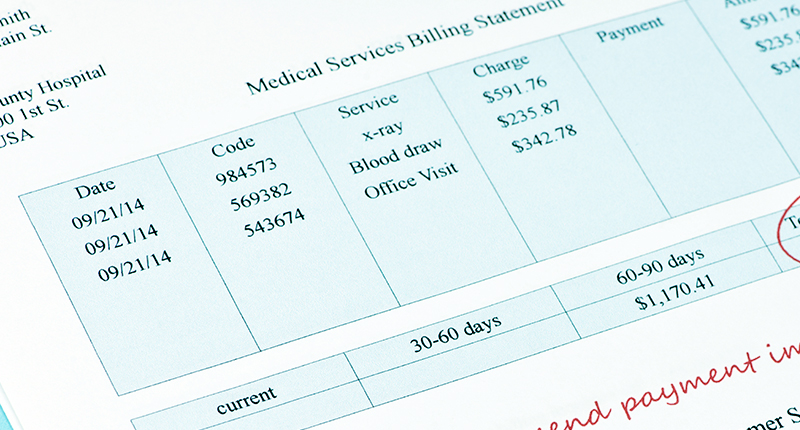
Radiology codes are used to describe various imaging procedures performed to diagnose and monitor medical conditions. These codes enable healthcare providers to accurately document and bill for radiology services, facilitating efficient communication with insurance companies and ensuring appropriate reimbursement.
X-ray, magnetic resonance imaging (MRI), and computed tomography (CT) scans are examples of imaging procedures covered by radiology codes. X-rays capture images of the body’s internal structures using low levels of radiation, and they are commonly used to detect fractures, lung infections, and other conditions. MRI scans use powerful magnets and radio waves to create detailed images of the body’s organs and tissues, aiding in the diagnosis of various diseases. CT scans involve combining multiple X-ray images taken from different angles to produce cross-sectional images of the body, providing valuable insights into specific medical conditions.
By utilizing specific radiology codes, healthcare providers can accurately document the type of imaging performed, the body part examined, and any additional techniques or procedures involved. This ensures proper billing and reimbursement for radiology services while maintaining accurate patient records.
Pathology and Laboratory Codes
Pathology and laboratory codes play a vital role in documenting and billing for diagnostic tests and examinations. These codes are used to describe the collection, processing, and analysis of various specimens to aid in the diagnosis and treatment of diseases. By using specific codes, healthcare providers can accurately communicate the type of test performed, the condition being investigated, and the results obtained.
Blood tests, pap smears, and tissue specimen examinations are examples of diagnostic procedures covered by pathology and laboratory codes. Blood tests encompass a wide range of tests, including complete blood counts, cholesterol screenings, and glucose tests, which provide valuable information about a patient’s overall health. Pap smears are used to screen for cervical cancer and involve collecting a sample of cells from the cervix for further examination. Tissue specimen examinations involve the microscopic analysis of biopsy samples to diagnose various diseases, such as cancer.
By employing pathology and laboratory codes, healthcare providers can ensure accurate documentation, appropriate billing, and effective communication with insurance companies and other healthcare professionals involved in patient care.
Medicine Codes
Medicine codes encompass a wide range of services and procedures provided in the field of medicine. These codes cover various medical specialties and treatments, such as allergy testing and treatment, chemotherapy administration, and physical therapy. By utilizing specific medicine codes, healthcare providers can accurately document and bill for the services they provide.
Allergy testing and treatment codes are used to document and bill for procedures like allergy testing, immunotherapy injections, and the evaluation and management of allergic conditions. Chemotherapy administration codes, on the other hand, capture the administration of chemotherapy drugs for the treatment of cancer and other related conditions. Physical therapy codes document the evaluation and management of patients requiring rehabilitation services to improve their physical functioning.
Medicine codes provide a standardized method of documenting and billing for medical services, ensuring accurate communication and appropriate reimbursement for healthcare providers, as well as facilitating effective coordination of patient care.
Maternity and Delivery Codes
Maternity and delivery codes play a crucial role in documenting and billing for services related to prenatal care, delivery, and postpartum care. These codes are essential in capturing the complexity and extent of care provided during pregnancy and childbirth.
Prenatal care codes are used to document and bill for the regular check-ups, screenings, and tests performed during pregnancy to ensure the health and well-being of both the mother and the baby. Delivery codes encompass the various procedures and interventions involved in the actual birth process, such as vaginal deliveries, cesarean sections, and the management of complications during delivery. Finally, postpartum care codes capture the healthcare services provided to the mother following childbirth, including follow-up visits, breastfeeding support, and the management of postpartum complications.
Accurate documentation and billing for maternity and delivery services are crucial in ensuring appropriate reimbursement for healthcare providers and maintaining comprehensive patient records. These codes also help facilitate effective communication and coordination of care among different healthcare professionals involved in the maternity care journey.
Emergency Department Codes
Emergency department (ED) codes are used to document and bill for services provided in emergency room settings. These codes capture the severity and complexity of the medical conditions encountered, as well as the level of care provided by emergency healthcare professionals.
Emergency room visit codes document and bill for the evaluation and management of patients who present to the ED seeking immediate care for various medical conditions and injuries. Trauma procedure codes cover the various surgical interventions and procedures performed in emergency situations, such as wound repair, fracture reduction, and stabilization of life-threatening injuries. Critical care services codes are used to capture the provision of intensive care to patients in life-threatening situations, often requiring constant monitoring and life-saving interventions.
Accurate documentation and billing for emergency department services are crucial in properly reflecting the level of care provided by emergency healthcare providers. These codes also facilitate the appropriate reimbursement for emergency services and ensure thorough record-keeping for future reference.
Chiropractic Codes
Chiropractic codes are used to document and bill for services provided by chiropractors, who focus on the diagnosis and treatment of musculoskeletal disorders, particularly those affecting the spine. Chiropractic codes encompass a wide range of services, including spinal manipulation, therapeutic procedures, and evaluation and management.
Spinal manipulation codes capture the manual adjustment of the spine to alleviate pain, improve joint mobility, and restore proper function. Therapeutic procedure codes encompass various treatments provided by chiropractors, such as therapeutic exercises, electrical stimulation, and ultrasound therapy, to address musculoskeletal conditions. Evaluation and management codes are used to document and bill for the comprehensive assessment, diagnosis, and treatment planning provided by chiropractors.
By utilizing specific chiropractic codes, healthcare providers can accurately document their services, communicate with insurance companies, and ensure proper reimbursement for chiropractic care. These codes also contribute to effective coordination of care among different healthcare professionals involved in the management of musculoskeletal conditions.
Dental Codes
Dental codes are used to document and bill for services provided by dental professionals. These codes cover a wide range of dental treatments and procedures, enabling accurate communication, documentation, and billing within the dental industry.
Oral examination codes capture the comprehensive assessment of a patient’s oral health, including the examination of the teeth, gums, and oral tissues, as well as the identification of any dental conditions or abnormalities. Tooth extraction codes encompass the removal of one or more teeth, whether it be for preventive or therapeutic purposes. Denture construction codes are used to document and bill for the fabrication and fitting of partial or complete dentures, which are removable prosthesis used to replace missing teeth.
By utilizing specific dental codes, dental professionals can accurately document their services, communicate with insurance companies, and ensure proper reimbursement for dental treatments and procedures. These codes also contribute to effective record-keeping and continuity of care for dental patients.
In conclusion, medical coding is a crucial aspect of healthcare administration that enables accurate documentation and billing for a wide range of medical services. Evaluation and Management codes, surgical codes, anesthesia codes, radiology codes, pathology and laboratory codes, medicine codes, maternity and delivery codes, emergency department codes, chiropractic codes, and dental codes are just a few examples of the many coding systems in place to ensure proper documentation, reimbursement, and coordination of care within the healthcare industry.