In the field of healthcare, medical coders play a crucial role in ensuring accurate documentation and billing processes. On a daily basis, a medical coder meticulously reviews patient medical records, assigning specific codes to each diagnosis, procedure, and treatment. These codes serve as a universal language that medical professionals and insurance companies utilize to communicate and process claims. By deciphering complex medical information and applying the appropriate codes, medical coders help maintain the integrity of healthcare data, streamline reimbursement procedures, and facilitate efficient patient care.
Patient Record Analysis

Reviewing medical documentation
As a medical coder, a significant portion of your daily responsibilities involves reviewing medical documentation. This includes patient records, physician notes, test results, and other relevant documents. By carefully analyzing these records, you can gain a holistic understanding of the patient’s medical history, diagnoses, treatments, and procedures. This step is crucial in ensuring accurate coding and billing processes.
Organizing and interpreting patient information
Once you have reviewed the medical documentation, it is essential to organize and interpret the information effectively. This involves extracting pertinent details such as the patient’s demographics, medical history, current conditions, and any ongoing treatments. By organizing this information in a systematic manner, you can easily reference and utilize it during the coding process.
Identifying relevant diagnoses and procedures
One of your primary responsibilities as a medical coder is to identify relevant diagnoses and procedures from the medical documentation. This requires a deep understanding of medical terminology, coding systems, and disease classifications. By accurately identifying and coding the diagnoses and procedures, you enable the coding process to translate the patient’s medical history into a standardized language that healthcare professionals and insurance companies can understand.
Medical Coding
Medical coding is a critical aspect of healthcare administration and billing. It involves assigning specific codes to diagnoses and procedures based on the patient’s medical records. By accurately coding this information, medical coders ensure proper billing, compliance with regulations, and consistency in healthcare documentation. In this guide, we will explore the key elements of medical coding, including the assignment of codes to diagnoses and procedures and the importance of accuracy and compliance with coding guidelines. Understanding these principles is essential for healthcare professionals involved in medical coding and billing processes.
Assigning appropriate codes to diagnoses
Medical coding involves assigning specific codes to the diagnoses found in the patient’s medical documentation. This process requires extensive knowledge of coding systems, such as the International Classification of Diseases (ICD), currently using ICD-10. By selecting the correct codes, you accurately represent the patient’s conditions, allowing for consistency across healthcare providers, insurance claims, and statistical analysis.
Assigning appropriate codes to procedures
Similar to diagnoses, medical coders are responsible for assigning appropriate codes to the procedures performed on patients. This includes surgeries, lab tests, imaging studies, and other interventions. Coding procedures accurately ensures that insurance claims reflect the complexity and resources required for each treatment. Additionally, this information is crucial for research and quality improvement initiatives.
Ensuring accuracy and compliance with coding guidelines
The accuracy of medical coding is of utmost importance to ensure compliance with coding guidelines. Adhering to coding rules and regulations ensures that the coding is consistent and follows standardized practices. Accurate and compliant coding leads to proper reimbursement, mitigates potential legal issues, and enables accurate reporting and analysis.
Medical Billing
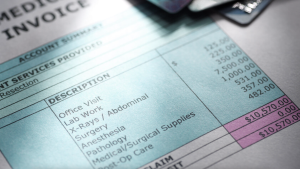
Preparing and submitting claims to insurance companies
Medical coders play a vital role in the medical billing process by preparing and submitting claims to insurance companies. This involves compiling the coded diagnoses and procedures into a comprehensive claim form and submitting it electronically or through other designated channels. Accurate and timely submission of claims is crucial to facilitate the reimbursement process.
Verifying insurance coverage and benefits
Prior to submitting claims, medical coders verify insurance coverage and benefits. This involves gathering information about the patient’s insurance provider, policy details, and any pre-authorization requirements. By ensuring that the patient’s insurance covers the provided services, medical coders help prevent claim rejections and facilitate smoother reimbursement processes.
Resolving billing discrepancies
Medical coders also play a crucial role in resolving billing discrepancies. This involves reviewing denied or rejected claims, identifying the cause of the discrepancy, and taking the necessary steps to rectify the issue. This may include contacting insurance companies, clarifying coding or documentation details, or appealing denied claims. By resolving billing discrepancies, medical coders ensure accurate reimbursement and maintain positive relationships with insurance providers.
Data Management

Maintaining and updating patient records
An essential aspect of a medical coder’s daily tasks includes maintaining and updating patient records. This involves accurately entering and recording coded data into electronic health record systems or other designated platforms. By ensuring the completeness and accuracy of patient records, medical coders contribute to efficient healthcare delivery and the availability of comprehensive patient information.
Entering coded data into computer systems
Once the diagnoses, procedures, and other relevant information are coded, medical coders enter this coded data into computer systems. The use of specific software or coding tools aids in the efficient and accurate entry of codes into electronic databases, ensuring accessibility, and facilitating information retrieval. This process allows other healthcare professionals to access and utilize coded data during patient care and administrative processes.
Ensuring confidentiality and security of data
The confidentiality and security of patient data are paramount in the field of medical coding. Medical coders must adhere to strict privacy regulations, ensuring that patient information remains confidential and secure. This involves following protocols, implementing encryption measures, and strictly adhering to the Health Insurance Portability and Accountability Act (HIPAA) guidelines. By maintaining the confidentiality and security of data, medical coders help foster trust between patients, healthcare providers, and insurance companies.
Audit and Compliance
Medical coders play a crucial role in maintaining the accuracy and compliance of healthcare records. This involves conducting coding audits to review coded information for accuracy and adherence to regulations.
Conducting coding audits for accuracy and adherence to regulations
To ensure accuracy and adherence to coding regulations, medical coders frequently conduct coding audits. These audits involve reviewing coded information for accuracy, completeness, and compliance with coding guidelines and regulations. By conducting these audits, medical coders contribute to quality assurance and identify areas where coding improvements or additional training may be necessary.
Maintaining knowledge of coding guidelines and regulations
In the ever-evolving field of healthcare, medical coders must stay updated on coding guidelines and regulations. This requires continuous learning and staying informed about changes in coding systems, such as updates to ICD, Current Procedural Terminology (CPT), and Healthcare Common Procedure Coding System (HCPCS). By maintaining knowledge of coding guidelines and regulations, medical coders ensure accurate and compliant coding practices.
Assisting with compliance programs
Medical coders often play an active role in assisting with compliance programs within healthcare organizations. This involves providing expertise in coding practices, participating in compliance training sessions, and contributing to the development of policies and procedures that adhere to coding regulations. By actively engaging in compliance programs, medical coders help ensure ethical and legal coding practices across the healthcare industry.
Medical Terminology and Coding Systems
Medical coders are essential in the healthcare industry, as they bridge the gap between medical terminology and coding systems. They must have a strong grasp of medical terminology, enabling them to interpret and translate medical information accurately.
Understanding medical terminology
A solid understanding of medical terminology is a fundamental requirement for medical coders. Medical coders must be familiar with the language used in medical documentation, including medical conditions, procedures, anatomy, and pharmacology. By having a strong grasp of medical terminology, medical coders can accurately interpret and translate medical information into appropriate codes.
Familiarity with coding systems (e.g., ICD-10, CPT, HCPCS)
Medical coders must be familiar with various coding systems used in healthcare, such as ICD-10, CPT, and HCPCS. These coding systems provide standardized codes for diagnoses, procedures, and medical supplies. By understanding the principles and conventions of these coding systems, medical coders can assign the most appropriate codes in a consistent and accurate manner, enabling effective communication and analysis within the healthcare industry.
Communication and Collaboration

Interacting with healthcare professionals to obtain missing information
As a medical coder, effective communication with healthcare professionals is essential. There may be instances where the medical documentation lacks necessary information for accurate coding. In such cases, medical coders communicate with physicians, nurses, and other members of the healthcare team to obtain the missing information. By collaborating with healthcare professionals, medical coders ensure the completeness and accuracy of coded data.
Collaborating with medical staff to clarify documentation
Collaboration with the medical staff is crucial for clarifying documentation and ensuring accurate coding. Medical coders may interface with physicians, nurses, and other clinical personnel to clarify ambiguous or incomplete documentation. By clarifying documentation, medical coders facilitate accurate coding, reduce potential coding errors, and contribute to the overall quality of patient care and reimbursements.
Providing coding guidance and education to healthcare team
Medical coders often serve as a valuable resource for providing coding guidance and education to other members of the healthcare team. This may involve conducting training sessions, presenting educational materials, or providing one-on-one guidance to improve coding knowledge and documentation practices. By sharing their expertise, medical coders enhance overall coding accuracy and ensure consistent coding practices within the healthcare team.
Quality Improvement

Identifying potential coding errors and inconsistencies
As part of their daily routine, medical coders are actively involved in identifying potential coding errors and inconsistencies. By carefully reviewing coded data and comparing it with medical documentation, coders can detect discrepancies or mistakes. This attention to detail and commitment to quality improvement helps in maintaining accurate healthcare data, preventing incorrect billing, and improving overall patient care.
Participating in quality improvement initiatives
Medical coders contribute to quality improvement initiatives by actively participating in efforts to enhance coding accuracy and efficiency. This may involve collaborating with quality improvement teams, attending meetings or conferences, and sharing best practices. By actively engaging in quality improvement initiatives, medical coders play a crucial role in refining coding processes and ultimately strengthening the healthcare system.
Contributing to accurate healthcare data for analysis
Accurate healthcare data is essential for analysis, research, and decision-making processes. Medical coders play a fundamental role in contributing to accurate healthcare data by ensuring the integrity and accuracy of coded information. Reliable and consistent coded data enable healthcare organizations and researchers to analyze trends, identify areas for improvement, and make informed decisions regarding patient care, resource allocation, and policy development.
Continuing Education

Staying updated on changes in medical coding guidelines
Medical coding is a dynamic field that undergoes frequent updates and changes. Medical coders must actively stay updated on these changes to remain current in their profession. This involves attending workshops, webinars, conferences, and reading industry publications to learn about the latest coding guidelines, regulations, and updates to coding systems. By staying updated, medical coders maintain their proficiency in accurate coding practices.
Participating in ongoing training and professional development
Continual learning and professional development are vital for medical coders. This process involves engaging in ongoing training programs that focus on enhancing coding skills, improving documentation practices, and staying updated on industry trends. By participating in these training opportunities, medical coders continuously refine their abilities and ensure the delivery of high-quality healthcare services.
Maintaining coding certifications
maintaining coding certifications is a requirement for medical coders to ensure their professional credibility and competency. Organizations such as the American Academy of Professional Coders (AAPC) and American Health Information Management Association (AHIMA) offer certifications such as Certified Professional Coder (CPC) and Certified Coding Specialist (CCS). By obtaining and maintaining these certifications, medical coders demonstrate their commitment to professionalism, compliance, and continuous learning.
Professional Ethics

Maintaining confidentiality of patient information
The ethical responsibility of medical coders includes maintaining the confidentiality of patient information. Medical coders must adhere to strict privacy regulations and protect sensitive patient data. This necessitates handling patient records with strict confidentiality, implementing security measures to prevent unauthorized access, and ensuring the secure transfer of information when required. By prioritizing patient privacy and confidentiality, medical coders promote trust and respect within the healthcare industry.
Adhering to professional standards and ethical guidelines
Medical coders must adhere to professional standards and ethical guidelines set by industry organizations. This includes following the professional code of ethics outlined by associations such as the AAPC and AHIMA. These standards emphasize qualities such as integrity, accuracy, professionalism, and honesty in coding practices. By upholding these professional standards, medical coders contribute to maintaining the integrity and reputation of the medical coding profession.
Avoiding conflicts of interest
Medical coders must adhere to the principle of avoiding conflicts of interest that may compromise their professional integrity. This includes refraining from engaging in activities that may result in personal gain at the expense of accurate coding. By prioritizing objectivity and the best interests of patients and healthcare organizations, medical coders maintain the trust and credibility required for effective coding and billing processes.
In conclusion, medical coders play a vital role in analyzing patient records, assigning appropriate codes, ensuring accurate billing, managing data, and maintaining compliance with coding guidelines. Their expertise in medical terminology, coding systems, and ethical practices contributes to the reliable analysis of healthcare data, effective reimbursement processes, and the provision of quality healthcare services. As the healthcare industry continues to evolve, medical coders must remain updated, engage in ongoing education, and prioritize professional ethics to meet the ever-changing challenges of their profession.


