In the realm of medical billing, understanding the concept of contractual obligation is crucial to ensuring accurate and efficient payment processes. Essentially, contractual obligation refers to the legal and financial responsibilities established between healthcare providers and insurance companies. This arrangement sets forth the terms, conditions, and reimbursement rates that both parties must adhere to. By familiarizing yourself with the intricacies of contractual obligation, you will be better equipped to navigate the complexities of medical billing and ensure proper reimbursement for the services provided.
Understanding Medical Billing

Overview of medical billing
medical billing refers to the process of submitting and following up on claims with health insurance companies in order to receive payment for services provided by healthcare providers. It involves various tasks such as verifying insurance coverage, coding medical procedures, and submitting claims. Medical billing is a crucial aspect of the healthcare industry as it ensures that healthcare providers are appropriately compensated for their services.
Importance of contractual obligation
Contractual obligation plays a significant role in medical billing. It refers to the legal and ethical responsibilities that healthcare providers have towards insurance companies and patients regarding payment for services. Understanding and adhering to contractual obligations is essential for accurate and timely reimbursement, maintaining legal and ethical standards, avoiding disputes, and building strong relationships with healthcare providers.
Contractual Obligation in Medical Billing
Medical cost concept with stethoscope and medical bill
Definition of contractual obligation
Contractual obligation in medical billing refers to the legally binding requirements and responsibilities between healthcare providers, insurance companies, and patients. These obligations are outlined in contractual agreements and dictate the terms and conditions for payment, insurance coverage, billing guidelines, and other aspects of medical billing.
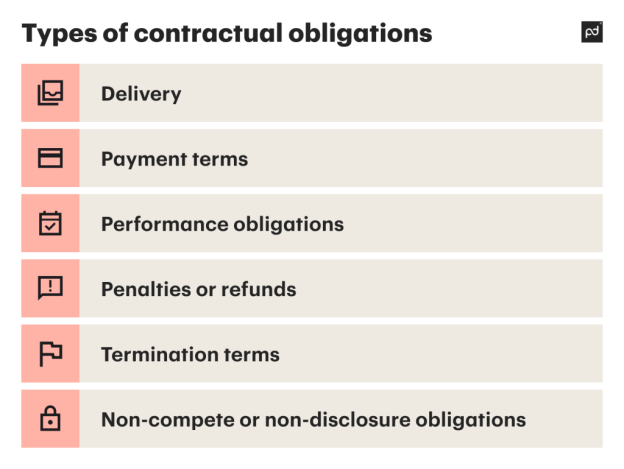
Types of contractual obligations
There are various types of contractual obligations in medical billing. One type is the agreement between healthcare providers and insurance companies, which outlines the payment terms, fee schedules, and insurance coverage. Another type is the agreement between healthcare providers and patients, which defines the financial responsibilities of the patient and the services covered by their insurance.
Contractual agreements with healthcare providers
Healthcare providers enter into contractual agreements with insurance companies to establish the terms and conditions for payment and reimbursement. These agreements define the fee schedules, payment terms, and insurance coverage for services rendered by the healthcare provider. They also outline the legal and ethical obligations that both parties must comply with.
Role of contractual obligation in medical billing
Contractual obligation acts as a framework for medical billing. It ensures that healthcare providers receive accurate and timely payment for their services, while also protecting the rights and interests of insurance companies and patients. By establishing clear responsibilities and guidelines, contractual obligations facilitate a smooth and efficient billing process.
Key Elements of Contractual Obligation

Payment terms and conditions
Payment terms and conditions are a crucial element of contractual obligations in medical billing. These define how and when healthcare providers will be reimbursed for their services. Payment terms may include details such as the timeframe for claims submission, the frequency of payment, and any penalties or interest for late payments.
Fee schedules
Fee schedules outline the fees charged by healthcare providers for specific medical procedures and services. These schedules are often negotiated between healthcare providers and insurance companies to determine the reimbursement rates. Fee schedules are an important aspect of contractual obligations as they govern the financial aspect of medical billing.
Insurance coverage
Insurance coverage is another key element of contractual obligation in medical billing. Healthcare providers must ensure that the services they render are covered by the patient’s insurance plan. This involves verifying insurance eligibility, obtaining pre-authorization for certain procedures, and submitting claims based on the coverage provided by the insurance company.
Medical coding and billing guidelines
Accurate medical coding is crucial for proper billing and reimbursement. Contractual obligations include adherence to coding guidelines and standards set forth by regulatory bodies and insurance companies. Healthcare providers must ensure that the procedures and diagnoses are coded correctly, as errors can lead to claim denials and delayed payments.
Legal implications
Contractual obligations in medical billing have legal implications. Breaching these obligations can result in consequences such as payment delays, claim denials, financial penalties, and even legal action. It is important for healthcare providers to understand and comply with the contractual obligations to avoid legal complications and maintain a professional reputation.
Importance of Contractual Obligation in Medical Billing

Ensuring accurate and timely payment
Complying with contractual obligations is essential for healthcare providers to receive accurate and timely payment for their services. By adhering to the payment terms and conditions, submitting claims based on insurance coverage, and following coding guidelines, healthcare providers increase the chances of successful reimbursement without delays or denials.
Maintaining legal and ethical standards
Contractual obligations in medical billing encompass legal and ethical responsibilities. Adhering to these obligations demonstrates professionalism and integrity in the healthcare industry. By maintaining legal and ethical standards, healthcare providers contribute to the overall trust and confidence in the billing process.
Avoiding contractual disputes
Clear contractual obligations help prevent disputes between healthcare providers and insurance companies. When both parties understand and comply with the agreed-upon terms, it reduces the likelihood of conflicts regarding payment, reimbursement, or coverage. Avoiding contractual disputes promotes a positive working relationship between healthcare providers and insurance companies.
Building strong relationships with healthcare providers
Compliance with contractual obligations can also lead to stronger relationships with healthcare providers. When insurance companies consistently fulfill their contractual obligations, healthcare providers are more likely to continue providing services and maintain a favorable relationship. Building strong relationships contributes to a smoother billing process and mutual trust between the parties involved.
Payment Terms and Conditions

Understanding payment terms
Payment terms in medical billing refer to the specific conditions that healthcare providers and insurance companies agree upon regarding payment. These terms outline when and how healthcare providers will receive reimbursement for their services. Common payment terms include the timeframe for claims submission, the frequency of reimbursement, and any penalties or interest for late payments.
Common payment conditions in medical billing
In medical billing, there are several common payment conditions that healthcare providers must understand. These conditions typically include the requirement for proper claims submission within a specified timeframe. Insurance companies often have deadlines for claims submission, and healthcare providers must comply to receive reimbursement. Additionally, payment conditions may specify the preferred method of payment, such as electronic funds transfer or paper checks.
Negotiating payment terms with healthcare providers
Healthcare providers have the opportunity to negotiate payment terms with insurance companies. By engaging in open and transparent communication, they can discuss and clarify payment terms to ensure a mutually beneficial agreement. Negotiating payment terms can help healthcare providers establish a fair and timely reimbursement process, reducing the potential for payment delays or disputes.
Fee Schedules

Defining fee schedules
Fee schedules in medical billing refer to the predetermined fees that healthcare providers charge for specific medical procedures and services. These schedules outline the costs associated with each service provided by the healthcare provider. Fee schedules are essential for consistent reimbursement rates and provide transparency regarding the financial aspects of medical billing.
Factors influencing fee schedules
Several factors influence fee schedules in medical billing. These may include the complexity of the procedure, the geographical location of the healthcare provider, the level of expertise required, and the prevailing market rates. Insurance companies often negotiate fee schedules with healthcare providers to determine the reimbursement rates for their services.
Billing based on fee schedules
Healthcare providers use fee schedules as a basis for billing and reimbursement. They refer to the predetermined fees when submitting claims to insurance companies for payment. Billing based on fee schedules ensures consistency and transparency in the billing process, providing a clear understanding of the services rendered and the associated costs.
Compliance with fee schedules
Healthcare providers must comply with the fee schedules agreed upon with insurance companies. Non-compliance with fee schedules can lead to delayed payments or claim denials, resulting in financial losses for the healthcare provider. By adhering to the agreed-upon fee schedules, healthcare providers ensure proper reimbursement and maintain a professional relationship with insurance companies.
Insurance Coverage

Understanding insurance coverage
Insurance coverage refers to the extent to which medical services and procedures are covered by a patient’s insurance plan. It outlines the specific services, treatments, and medications that are reimbursable under the insurance policy. Understanding insurance coverage is crucial for healthcare providers to ensure appropriate billing and reimbursement for the services they render.
Contractual obligations between insurance companies and healthcare providers
Insurance companies and healthcare providers have contractual obligations regarding insurance coverage. These obligations establish the terms and conditions for reimbursement based on the coverage provided by the insurance company. Healthcare providers must verify insurance coverage for each patient and submit claims based on the services covered under the insurance policy.
Verifying insurance coverage
Healthcare providers have a responsibility to verify the insurance coverage of their patients. This involves obtaining accurate insurance information, checking the patient’s eligibility, and determining the services covered by their insurance plan. Verifying insurance coverage helps healthcare providers understand the financial responsibilities of the patient and ensures accurate billing and reimbursement.
Submitting claims based on insurance coverage
Submitting claims based on the insurance coverage is an essential aspect of medical billing. Healthcare providers must accurately document and code the services provided, ensuring that they align with the coverage outlined in the patient’s insurance policy. This ensures that claims are processed correctly and reimbursed according to the insurance coverage.
Medical Coding and Billing Guidelines

Importance of accurate coding
Accurate medical coding is crucial for proper billing and reimbursement. Medical codes are used to represent diagnoses, procedures, and services provided by healthcare providers. They enable insurance companies to determine the appropriate reimbursement and ensure that services are billed accurately. Accurate coding ensures proper reimbursement and reduces the likelihood of claim denials or payment delays.
Adhering to billing guidelines
Medical billing guidelines provide a framework for the proper submission of claims. These guidelines outline the specific requirements and documentation necessary for accurate billing and reimbursement. Healthcare providers must adhere to these guidelines to ensure that claims are processed smoothly and without complications.
Role of contractual obligation in coding and billing
Contractual obligations play a pivotal role in coding and billing. They define the rules and guidelines that healthcare providers must follow when documenting and coding medical procedures. By adhering to the contractual obligations, healthcare providers ensure accuracy in coding, avoid compliance issues, and increase the chances of successful reimbursement.
Legal Implications

Consequences of breaching contractual obligations
Breaching contractual obligations in medical billing can have various consequences. It may lead to delayed or denied payments, financial penalties, and damage to the reputation of the healthcare provider. Additionally, breaching contractual obligations may result in legal action, as insurance companies or patients can seek legal remedies for non-compliance.
Resolving contractual disputes
When contractual disputes arise in medical billing, it is important to resolve them promptly and effectively. Disputes may occur due to disagreements about payment terms, insurance coverage, or coding and billing guidelines. Resolving contractual disputes often involves open communication, negotiation, and potentially seeking legal counsel to achieve a fair and equitable resolution.
Legal considerations in medical billing
Medical billing involves various legal considerations that healthcare providers must be aware of. These considerations include compliance with healthcare laws and regulations, protection of patient privacy and confidentiality, and adherence to contractual obligations. Understanding and adhering to the legal aspects of medical billing is crucial for healthcare providers to minimize legal risks and ensure ethical practices.
Conclusion
Contractual obligation plays a fundamental role in medical billing. It encompasses the legal and ethical responsibilities that healthcare providers have towards insurance companies and patients. By understanding and adhering to contractual obligations, healthcare providers can ensure accurate and timely payment, maintain legal and ethical standards, avoid disputes, and build strong relationships with healthcare providers. Compliance with contractual obligations is essential for a smooth and efficient billing process and contributes to the overall trust and confidence in the healthcare industry.