In the field of healthcare, medical coding plays a vital role in ensuring accurate documentation and proper reimbursement for services rendered. It involves the assignment of alphanumeric codes to various medical procedures, diagnoses, and treatments. This article will explore a few notable examples of medical coding, highlighting its significance in healthcare management and the impact it has on both patients and healthcare providers alike. From the classification of diseases to the identification of specific pharmaceutical products, medical coding offers a systematic approach to streamline healthcare operations and facilitate effective communication among healthcare professionals.
Medical Coding Basics

Introduction to Medical Coding
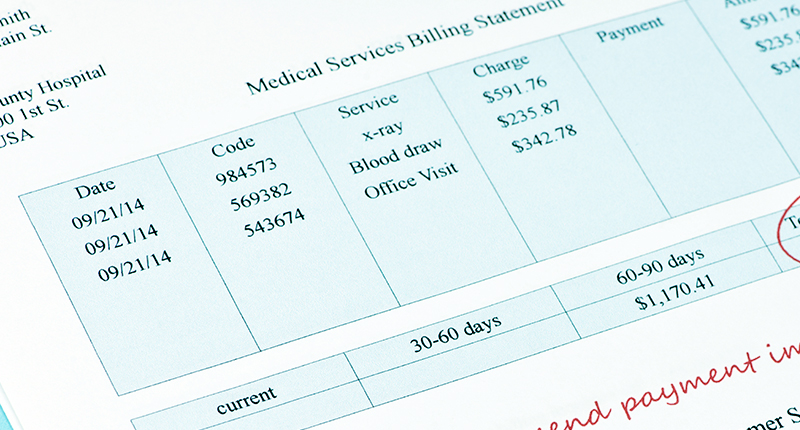
Medical coding is an integral part of the healthcare industry as it plays a crucial role in the accurate documentation, billing, and reimbursement processes. It involves translating medical diagnoses, procedures, and services into alphanumeric codes, which are then used for communication and reimbursement purposes. This standardized system allows healthcare providers, insurance companies, and regulatory bodies to understand and track the services provided to patients.
Purpose of Medical Coding
The primary purpose of medical coding is to ensure uniformity and accuracy in healthcare documentation and billing processes. By assigning specific codes to medical diagnoses, procedures, and services, medical coding enables effective communication and information exchange between healthcare professionals, insurance companies, and other stakeholders. These codes also play a crucial role in determining appropriate reimbursement for healthcare services, facilitating research, and supporting quality improvement initiatives.
Medical Coding Systems
Medical coding systems form the foundation of the coding process, providing a structured framework for assigning codes to various healthcare services. The three main coding systems used in medical coding are:
- International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM)
- Current Procedural Terminology (CPT) Codes
- Healthcare Common Procedure Coding System (HCPCS) Codes
ICD-10-CM
Overview of ICD-10-CM
ICD-10-CM is a widely used coding system designed to capture and classify diagnoses and signs, symptoms, abnormal findings, and external causes of diseases or injuries. It is maintained and regularly updated by the World Health Organization (WHO) and is used by healthcare providers, hospitals, and insurance companies globally. The system utilizes alphanumeric codes to categorize various medical conditions, providing a detailed and comprehensive classification framework.
Benefits of ICD-10-CM Coding
The implementation of ICD-10-CM has brought several benefits to the healthcare industry. Some of the key advantages include:
- Increased Specificity: ICD-10-CM offers a greater level of detail and specificity compared to its predecessor, ICD-9-CM. This enables more accurate reporting and improved clinical documentation, resulting in better healthcare planning, resource allocation, and epidemiological research.
- Enhanced Reimbursement: The use of ICD-10-CM codes enables healthcare providers to accurately code and bill for services provided to patients. This helps minimize billing errors and ensures appropriate reimbursement, ultimately enhancing financial stability for healthcare organizations.
- Improved Research and Analytics: The detailed nature of ICD-10-CM codes allows for better analysis of healthcare data, leading to improved research capabilities, identification of disease patterns, and monitoring of public health trends. This enables proactive healthcare interventions and evidence-based decision-making.
Examples of ICD-10-CM Codes
ICD-10-CM codes cover a wide range of medical conditions. Here are some examples of ICD-10-CM codes:
- A09 – Infectious gastroenteritis and colitis, unspecified
- G20 – Parkinson’s disease
- M54.5 – Low back pain
- N18.3 – Chronic kidney disease, stage 3 (moderate)
- S72.001A – Unspecified fracture of right femur, initial encounter for closed fracture
CPT Codes
Overview of CPT Codes
Current Procedural Terminology (CPT) codes are a set of standard codes maintained by the American Medical Association (AMA). They are primarily used to describe medical procedures and services provided by healthcare professionals, such as physicians, surgeons, and other allied healthcare providers. CPT codes provide a common language for reporting medical procedures, facilitating accurate billing, and improving communication within the healthcare system.
Common CPT Codes
CPT codes cover a wide range of medical procedures and services. Some common categories of CPT codes include:
- Evaluation and Management (E&M): These codes are used to document and bill for patient encounters, such as office visits, hospital visits, and consultations.
- Surgical Procedures: CPT codes for surgical procedures cover various specialties, including general surgery, orthopedics, cardiovascular surgery, and more.
- Diagnostic Testing: CPT codes exist for a range of diagnostic tests, such as blood tests, imaging studies (X-rays, MRIs), and electrocardiograms (ECGs).
- Therapy Services: Codes for therapy services encompass physical therapy, occupational therapy, speech therapy, and other rehabilitative treatments.
Examples of CPT Codes
Here are a few examples of CPT codes to provide a better understanding of their usage:
- 99213 – Established patient office visit, typically 15 minutes
- 64721 – Carpal tunnel release, with or without tenosynovectomy
- 58662 – Laparoscopy, surgical; with bilateral total pelvic lymphadenectomy and biopsy(ies) of uterine adnexa
- 36415 – Collection of venous blood by venipuncture
- 90837 – Psychotherapy, 60 minutes, for an individual in an outpatient setting
HCPCS Codes

Introduction to HCPCS Codes
The Healthcare Common Procedure Coding System (HCPCS) is a coding system used to report and bill for supplies, equipment, and services that are not covered by CPT codes. HCPCS codes are maintained by the Centers for Medicare and Medicaid Services (CMS) and are used primarily in the United States. These codes provide a comprehensive range of alphanumeric codes that cover durable medical equipment, drugs, ambulance services, and more.
Types of HCPCS Codes
HCPCS codes are divided into two main levels. Level I codes are identical to CPT codes and represent physician and other providers’ services. Level II codes, on the other hand, are alphanumeric and cover items and services not included in Level I codes. Level II codes are further subdivided into various sections, including:
- A – Transportation, Medical and Surgical Supplies, Miscellaneous and Experimental
- E – Durable Medical Equipment (DME)
- J – Drugs administered other than oral method, chemotherapy drugs
Examples of HCPCS Codes
Here are a few examples of HCPCS codes across different sections:
- A0425 – Ground mileage, per statute mile
- E0607 – Pressure pad for mattress, standard
- J0881 – Injection, darbepoetin alfa, 1 microgram (non-esrd use)
- Q5001 – Synthetic interferon, alpha 2B
- S5550 – Cranial cervical orthosis
DRG Codes

Understanding DRG Codes
The Diagnosis-Related Group (DRG) coding system is used primarily for categorizing and classifying inpatient hospital stays in the United States. DRGs group patients with similar characteristics, conditions, and resource utilization, allowing for consistent reimbursement rates and comparisons between hospitals. Each DRG has a specific payment weight associated with it, determining the reimbursement for the entire hospital stay, regardless of the actual costs incurred.
Use of DRG Codes
DRG codes play a pivotal role in the hospital reimbursement process, as they determine the payment for inpatient services rendered. Insurance companies, including Medicare and Medicaid, utilize DRG codes to calculate reimbursement rates based on the patient’s diagnosis, procedures performed, age, and other factors. Additionally, DRG codes facilitate benchmarking and outcome analysis, enabling hospitals to evaluate their performance and make data-driven improvements.
Examples of DRG Codes
DRG codes cover a broad range of medical conditions and procedures. Here are a few examples of DRG codes:
- DRG 247 – Percutaneous cardiovascular procedures with drug-eluting stent with medically managed acute myocardial infarction
- DRG 392 – Esophagitis, gastroent, misc digest disorders with major gastrointestinal procedure with CC
- DRG 456 – Spinal fusions except cervical with spinal curvature or malignancy or infection or extensive fusion of the spine
- DRG 637 – Diabetes with complication, age > 35 with complications with major CC
- DRG 811 – Red blood cell disorders with MCC
Modifiers
Importance of Modifiers in Medical Coding
Modifiers are essential components of the medical coding system as they provide additional information to clarify the nature and extent of a medical service or procedure. These two-digit codes are added to the main procedure or service code to indicate specific circumstances, such as multiple procedures, altered anatomical sites, or distinct levels of service. Modifiers play a critical role in ensuring accurate billing, communication between healthcare providers, and appropriate reimbursement determination.
Common Modifiers
Modifiers are categorized into various groups and subsets, each serving a specific purpose. Some commonly utilized modifiers include:
- -25: Significant, separately identifiable evaluation and management service by the same physician on the same day of a procedure or other service.
- -59: Distinct procedural service, indicating that a procedure or service is independent of another service performed on the same day.
- -TC: Technical component, indicating that only the technical aspect of a service or procedure was performed.
- -RT/-LT: Right side/left side, indicating that a procedure or service was performed on a specific side of the body.
Examples of Modifier Usage
Here are a few examples to illustrate the usage of modifiers in medical coding:
- 99213-25 – Office visit – established patient, significant, separately identifiable evaluation and management service on the same day as a procedure
- 29881-59 – Arthroscopy, knee, surgical; with meniscectomy, medial and lateral, including any meniscal shaving
- 93880-TC – Duplex scan of extracranial arteries; complete bilateral study
- 27829-RT – Open treatment of patellar fracture, with internal fixation, right patella
- 97110-59 – Therapeutic exercises, 15 minutes, requiring skilled therapists, distinct procedural service
E&M Coding
This image is property of nokomishealth.com.
Definition of Evaluation and Management (E&M) Coding
Evaluation and Management (E&M) coding refers to the process of assigning codes to patient encounters or visits that involve the evaluation, examination, and management of a patient’s medical condition. E&M codes reflect the level of complexity, medical decision-making, and documentation required for the encounter. These codes are vital for billing purposes, determining reimbursement, and communicating the severity of the patient’s condition to other healthcare professionals.
Components of E&M Coding
E&M codes consider various components to determine the appropriate level of service. The key components include:
- History: Assessing the patient’s symptoms, medical background, and pertinent details related to the current visit.
- Examination: Performing a relevant physical examination to assess the patient’s condition systematically.
- Medical Decision-Making: Evaluating the complexity of the patient’s condition, considering factors such as diagnosis, treatment options, risk, and follow-up requirements.
- Time: Considering the total time spent on the encounter, including face-to-face time with the patient and any additional work performed outside the encounter.
Examples of E&M Codes
Here are examples of E&M codes that represent different levels of service:
- 99202 – Office visit – new patient, low complexity, with a detailed history, expanded problem-focused examination, straightforward medical decision-making
- 99213 – Office visit – established patient, moderate complexity, with an expanded problem-focused history, expanded problem-focused examination, straightforward medical decision-making
- 99285 – Emergency department visit – moderate to high complexity, with a comprehensive history, comprehensive examination, medical decision-making of moderate complexity
- 99245 – Office consultation – new or established patient, comprehensive history, comprehensive examination, high complexity medical decision-making, face-to-face time over 60 minutes
Anesthesia Codes
Overview of Anesthesia Coding
Anesthesia coding involves assigning codes to the administration of anesthesia during surgical or medical procedures. Anesthesia services are essential to ensure patient comfort and safety during invasive or painful interventions. Proper coding of anesthesia services allows for accurate billing, appropriate reimbursement, and documentation of the specific anesthesia techniques employed.
Types of Anesthesia Codes
Anesthesia codes can be divided into three main categories based on the type of anesthesia provided:
- General Anesthesia: Codes for general anesthesia indicate a state of drug-induced unconsciousness, pain control, and muscle relaxation throughout the entire procedure.
- Regional Anesthesia: These codes represent the injection or infusion of anesthetic agents to block specific nerve impulses, rendering a specific area of the body temporarily numb.
- Monitored Anesthesia Care: Codes for monitored anesthesia care signify anesthesia services provided for procedures that do not require general or regional anesthesia. These services involve the administration of sedation or analgesia, with continuous patient monitoring.
Examples of Anesthesia Codes
Here are examples of anesthesia codes representing various types:
- 00300 – Anesthesia for procedures on integumentary system of one extremity, not otherwise specified
- 01991 – Monitored anesthesia care for patient of extreme age, younger than 1 year and older than 70 years, first 30 minutes
- 00532 – Anesthesia for open or surgical arthroscopic procedures on knee joint; with gastrocnemius recession
- 01967 – Neuraxial labor analgesia/anesthesia for planned vaginal delivery, including any associated induction or augmentation
- 01404 – Anesthesia for pharyngeal surgery
Radiology Codes

Introduction to Radiology Coding
Radiology coding involves classifying and assigning codes to medical imaging procedures, such as X-rays, CT scans, MRIs, and ultrasounds. These procedures are vital for diagnosing and monitoring various medical conditions. Accurate and detailed coding of radiology services ensures proper billing, facilitates reimbursement, and supports effective communication among healthcare professionals.
Types of Radiology Codes
Radiology codes cover a wide range of imaging procedures across different modalities. Some common types of radiology codes include:
- Radiologic Supervision and Interpretation (RS&I): Codes for RS&I encompass the professional interpretation of radiologic images and supervision of the technical aspects of the radiology procedure.
- Diagnostic Radiology: These codes represent the technical component of the radiology procedure, including the use of specific equipment and techniques for image acquisition.
- Interventional Radiology: Codes for interventional radiology cover procedures that involve the use of radiological guidance to perform minimally invasive therapeutic or diagnostic interventions.
Examples of Radiology Codes
Here are examples of radiology codes across different modalities and procedures:
- 72040 – Radiologic examination, spine, entire, survey study, anteroposterior and lateral
- 70553 – MRI brain, without contrast, followed by contrast
- 74183 – CT abdomen and pelvis; without contrast material and without contrast material in certain specified clinical scenarios
- 76805 – Ultrasound, pregnant uterus, real-time with image documentation, fetal and maternal evaluation, second and third trimesters
- 76000 – Fluoroscopy, physician time more than one hour, assisting a non-radiologic physician
Pathology and Laboratory Codes

Understanding Pathology and Laboratory Coding
Pathology and Laboratory coding involves assigning codes to various laboratory tests, procedures, and services performed on patient specimens. These codes capture essential diagnostic, therapeutic, and monitoring elements required for providing comprehensive healthcare. Accurate coding of pathology and laboratory services enables effective communication, billing, and reimbursement for the diagnostic and analytical services provided.
Types of Pathology and Laboratory Codes
pathology and laboratory codes cover a broad spectrum of tests and services offered in the clinical laboratory setting. Some common categories of Pathology and Laboratory codes include:
- Laboratory Panels: Codes representing a comprehensive group of laboratory tests commonly performed together to screen for specific diseases or conditions.
- Molecular Pathology: These codes cover molecular diagnostic testing, including DNA/RNA analysis, genetic testing, and other molecular profiling techniques.
- Special Stain and IHC: Codes for special stains and immunohistochemistry (IHC) allow for the identification and characterization of specific cellular components and molecular markers.
- Microbiology: Microbiology codes include tests and services related to the detection, identification, and susceptibility testing of microorganisms, such as bacteria, viruses, and fungi.
Examples of Pathology and Laboratory Codes
Here are examples of pathology and laboratory codes across different categories:
- 80050 – General health panel – comprehensive metabolic panel (CMP) and complete blood count (CBC)
- 88305 – Surgical pathology, gross and microscopic examination, for each tissue or organ biopsy; with routine H&E stain(s)
- 81479 – Unlisted molecular pathology procedure, not otherwise specified
- 87081 – Bacterial culture, aerobic, with isolation and presumptive identification of isolates
- 88342 – Immunohistochemistry or immunocytochemistry, per specimen; each antibody separately identified
In conclusion, medical coding is a critical process in healthcare, ensuring standardized documentation, accurate billing, and effective communication. Understanding the basics of coding systems, such as ICD-10-CM, CPT codes, HCPCS codes, DRG codes, modifiers, E&M coding, anesthesia codes, radiology codes, and pathology and laboratory codes, is essential for healthcare professionals involved in coding and billing procedures. accurate and comprehensive coding helps streamline healthcare operations, supports reimbursement, improves patient care, and facilitates data analysis for research and quality improvement initiatives.