Clinical coding systems play a crucial role in the healthcare industry by providing standardized codes that accurately represent medical diagnoses, procedures, and treatments. These coding systems, such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT), are essential for ensuring consistent and precise documentation, billing, and reimbursement for healthcare services. The effective use of clinical coding systems not only improves patient care and safety but also facilitates efficient communication among healthcare professionals, insurers, and researchers. In this article, we will explore the importance and benefits of clinical coding systems in the healthcare industry.
Overview of Clinical Coding Systems
There are several other relevant degrees and certifications in the healthcare coding and management field:
Definition of clinical coding systems
Clinical coding systems play a crucial role in the healthcare industry by providing standardized codes to classify diagnoses, procedures, and other relevant medical information. These systems use alphanumeric codes to represent various aspects of patient care, enabling healthcare professionals to accurately document and communicate medical data. Clinical coding systems have become integral to medical record management, reimbursement processes, and healthcare data analysis.
Importance of clinical coding systems
The implementation of clinical coding systems is vital for several reasons. Firstly, these systems ensure consistent and uniform documentation, allowing healthcare providers to communicate effectively both within their organizations and with external entities. By using standardized codes, medical professionals can accurately convey patient information, facilitating seamless sharing of data across healthcare providers and improving care coordination.
Secondly, Clinical coding systems have significant implications for reimbursement and billing processes. The accurate capture and coding of medical services provided to patients are essential for appropriate reimbursement from insurance payers. The use of correct and specific codes ensures accurate claims processing, reducing the risk of claim denials and ensuring providers receive the fair reimbursement they deserve.
Furthermore, clinical coding systems contribute to healthcare data analysis and research efforts. These systems enable the aggregation and analysis of vast amounts of medical information, allowing researchers and policymakers to identify trends, evaluate outcomes, and make informed decisions. Clinical coding systems serve as a foundation for accurate and reliable healthcare data, which is instrumental in advancing medical knowledge and improving patient care.
Classification Systems

ICD-10
The International Classification of Diseases, Tenth Revision (ICD-10), is a widely used clinical coding system for classifying diseases, injuries, and external causes of morbidity and mortality. Developed by the World Health Organization (WHO), ICD-10 provides detailed codes that allow healthcare professionals to accurately document and analyze various health conditions. It contains over 70,000 diagnostic codes, making it a comprehensive and robust classification system.
ICD-11
ICD-11 is the latest version of the International Classification of Diseases, developed by the WHO. It is designed to capture advancements in medical knowledge and technology. ICD-11 introduces new concepts, such as extensions for clinical documentation and greater alignment with electronic health record (EHR) systems. This updated classification system supports more precise coding and enhances the interoperability of health information globally.
SNOMED CT
Systematized Nomenclature of Medicine-Clinical Terms (SNOMED CT) is a comprehensive clinical coding system used to represent clinical data in EHRs and other health information systems. SNOMED CT offers a broad coverage of medical concepts, facilitating the standardized documentation, sharing, and analysis of health information. It enables the capture of clinical details with high specificity, improving clinical decision-making and patient care.
HCPCS
The Healthcare Common Procedure Coding System (HCPCS) is a coding system used primarily for identifying medical services, supplies, and equipment for billing purposes in the United States. HCPCS includes two levels of codes: Level I codes are identical to those in the American Medical Association’s Current Procedural Terminology (CPT) system, while Level II codes are alphanumeric and provide additional specificity. HCPCS ensures uniformity in billing practices across healthcare providers and facilitates accurate reimbursement.
Medical Nomenclature
These standardized naming systems play a crucial role in ensuring accurate and consistent communication among healthcare professionals, researchers, and organizations within the medical field. Medical nomenclature is essential for effective medical documentation, diagnosis, treatment, and research.
Definition of medical nomenclature
Medical nomenclature refers to the naming conventions and terminologies used in medicine to describe diseases, conditions, procedures, anatomical structures, and other relevant medical concepts. It provides a standardized language that healthcare professionals can use to communicate clinical information accurately. Medical nomenclature systems often interact with clinical coding systems, as the codes assigned to medical data must align with the terminology used.
Common medical nomenclatures
Several medical nomenclature systems are widely used in healthcare. The Systematized Nomenclature of Medicine (SNOMED) provides a comprehensive and hierarchically organized terminology for clinical medicine. SNOMED includes more detailed terms compared to other nomenclatures, enabling precise clinical documentation. Additionally, the Medical Subject Headings (MeSH) is a nomenclature system used in biomedical literature indexing for categorizing topics and concepts. MeSH facilitates efficient information retrieval in research databases, enhancing knowledge discovery and literature review processes.
Coding Guidelines
Coding guidelines in healthcare serve a critical purpose in ensuring the accurate and consistent assignment of codes to medical data. These guidelines provide a standardized framework and a set of rules that clinical coders must follow when translating clinical information into codes.
Purpose of coding guidelines
Coding guidelines serve as a standardized framework for clinical coders to follow when assigning codes to medical data. These guidelines provide instructions and rules to ensure consistency and accuracy in code assignment. Coding guidelines help coders interpret complex clinical scenarios, navigate ambiguous documentation, and apply the appropriate codes in a systematic and consistent manner.
Key principles of coding guidelines
Coding guidelines are based on several key principles aimed at promoting accurate code assignment. One primary principle is code specificity, which emphasizes the use of the most precise code available to describe a patient’s condition or procedure. Specific codes contribute to more accurate data analysis and improve the quality of research and decision-making based on coded data.
Another key principle is adherence to official coding guidelines. These guidelines are developed by coding authorities, such as the Centers for Medicare and Medicaid Services (CMS) in the United States, and provide instructions specific to each coding system. Following these guidelines ensures compliance with regulatory requirements and promotes coding consistency across healthcare organizations.
Clinical coders should also ensure that the assigned codes are supported by sufficient clinical documentation. Accurate coding relies on the availability of detailed and comprehensive documentation, which accurately reflects the patient’s medical condition and the services provided. Coding guidelines emphasize the importance of obtaining complete and accurate clinical documentation to support coding decisions.
Clinical coding accuracy
Achieving high levels of clinical coding accuracy is essential for several reasons. Accurate coding ensures that the patient’s medical information is correctly reflected in their health records, enabling healthcare providers to make informed clinical decisions and provide optimal care. It also contributes to accurate reimbursement, as coded data is used for billing and claims processing. Additionally, accurate coding supports healthcare data analysis by providing reliable and valid information for research, quality improvement initiatives, and population health management.
Role of Clinical Coders

Responsibilities of a clinical coder
Clinical coders play a critical role in accurately representing healthcare data through coding. Their responsibilities include reviewing and analyzing medical documentation, assigning appropriate codes, and verifying the completeness and accuracy of coded data. Clinical coders must possess in-depth knowledge of coding systems, guidelines, and medical terminology to effectively assign codes. They collaborate closely with healthcare professionals to clarify documentation and ensure accurate code assignment.
Clinical coders also have a responsibility to maintain patient privacy and confidentiality. They handle sensitive health information and must strictly adhere to legal and ethical standards governing the protection of patient data. Coders must also stay updated on industry regulations and coding requirements to ensure compliance with evolving standards.
Skills and qualifications
Successful clinical coders possess several key skills and qualifications. Proficiency in medical terminology, anatomy, and physiology is crucial to accurately interpret and assign codes based on clinical documentation. Knowledge of coding systems, such as ICD-10 and SNOMED CT, is essential to understand the coding structure and guidelines.
Analytical and critical thinking skills are fundamental for clinical coders to review complex medical records, identify pertinent information, and assign appropriate codes. Attention to detail is crucial, as the accuracy of coded data impacts patient care, reimbursement, and healthcare data analysis.
Clinical coders typically hold certifications, such as Certified Coding Specialist (CCS) or Certified Professional Coder (CPC), to validate their coding expertise. These certifications often require completion of formal education or coding training programs and passing a rigorous examination.
Importance of ongoing education and training
Continuing education and training are vital for clinical coders to stay informed about advancements in coding systems, guidelines, and industry best practices. Regular training ensures coders remain up to date with changes to coding systems, including updates to codes and guidelines. Ongoing education also helps coders enhance their skills, stay abreast of emerging medical technologies, and maintain proficiency in coding accuracy and compliance.
By participating in professional development activities, clinical coders can refine their coding skills, expand their knowledge base, and adapt to changing healthcare regulations. Continuous learning also prepares coders for the introduction of new coding systems and technologies, such as the transition from ICD-10 to ICD-11, ensuring a smooth integration into their coding practices.
Coding Audits

Purpose of coding audits
Coding audits are systematic reviews of coded healthcare data to assess its accuracy, completeness, and compliance with coding guidelines. The primary purpose of coding audits is to identify any discrepancies or errors in the coding process and to ensure adherence to regulatory requirements. Coding audits play a vital role in maintaining coding integrity, minimizing coding errors, and improving coding accuracy and compliance.
Methods of conducting coding audits
Coding audits can be conducted through various methods, depending on the organization’s size, resources, and specific goals. Some common methods include sample-based audits, targeted audits, and retrospective or concurrent audits.
Sample-based audits involve selecting a representative sample of coded records for review. This method allows auditors to assess the overall accuracy and compliance of coded data by examining selected cases.
Targeted audits focus on specific areas of concern or high-risk coding areas. These audits may be triggered by identified patterns of errors or changes in coding guidelines. Targeted audits provide a focused review of specific coding-related issues and allow for corrective action to be implemented.
Retrospective audits involve reviewing coded data after the patient’s treatment or encounter has concluded. This method allows auditors to assess the accuracy and compliance of coded data based on the completed clinical documentation.
Concurrent audits, on the other hand, occur in real-time, alongside the patient’s treatment or encounter. These audits provide immediate feedback to coders and clinicians, allowing for timely corrections and improvements in documentation and coding processes.
Benefits of coding audits
Coding audits offer numerous benefits to healthcare organizations. Firstly, they help identify coding errors, discrepancies, and documentation gaps, allowing for corrective actions to be taken to improve coding accuracy and compliance. By addressing coding deficiencies, organizations can minimize claim denials, reduce the risk of audits, and optimize revenue cycle management.
Coding audits also serve as a valuable educational tool for clinical coders. Audits provide feedback on coding performance, highlighting areas for improvement and identifying opportunities for targeted education and training. By addressing coding knowledge gaps, coders can enhance their skills, ultimately leading to improved accuracy and compliance.
Furthermore, coding audits contribute to the overall quality of healthcare data. Audits help validate the integrity and reliability of coded data, ensuring its accuracy and completeness. Accurate and reliable data supports informed decision-making, quality improvement initiatives, and research efforts, ultimately leading to improved patient outcomes and healthcare delivery.
Electronic Health Records
This image is property of mljhky9ue8ba.i.optimole.com.
Integration of clinical coding systems in EHRs
The integration of clinical coding systems within electronic health records (EHRs) is essential for effective documentation, data management, and interoperability. By incorporating clinical coding systems into EHRs, healthcare providers can accurately capture and classify patient information while maintaining consistency and standardization.
Clinical coding systems integrated into EHRs enable healthcare professionals to assign codes directly to patient data within the electronic documentation. This integration enhances coding efficiency, reduces errors, and ensures accurate code assignment. It also supports the seamless exchange of coded data across healthcare settings, promoting care continuity and facilitating the sharing of health information for collaborations and research.
Advantages and challenges
The integration of clinical coding systems into EHRs offers several advantages. Firstly, it improves the accuracy and completeness of coded data. When coding is performed within the EHR, coders have direct access to comprehensive clinical documentation, reducing the risk of incomplete or inaccurate coding. This not only ensures accurate representation of the patient’s condition but also facilitates more accurate reimbursement and healthcare data analysis.
Another advantage is the enhanced interoperability of coded data. With coding systems integrated into EHRs, healthcare organizations can easily exchange coded information, allowing for seamless information sharing and improved care coordination. This interoperability supports population health management, research collaborations, and the development of clinical decision support systems.
However, integrating clinical coding systems into EHRs also comes with challenges. One challenge is the need for ongoing system updates and maintenance to reflect changing coding guidelines and updates in the classification systems. Regular updates ensure that the EHR captures and supports the latest coding requirements, minimizing the risk of non-compliance and outdated coding practices.
Additionally, training and education on the use of coding systems within EHRs are necessary to ensure proper utilization by healthcare professionals. Adequate user training and support are critical for coders, clinicians, and other EHR users to understand the coding functionalities and utilize them effectively. Education programs can help users optimize the benefits of clinical coding systems within EHRs while maintaining accuracy and compliance.
Improving clinical documentation
The integration of clinical coding systems in EHRs provides an opportunity to improve clinical documentation practices. With direct access to coding functionalities within the EHR, healthcare professionals can accurately assign codes as they document the patient’s care. This real-time coding promotes accurate and complete documentation, reducing the need for retrospective coding and minimizing errors.
Additionally, coding systems integrated into EHRs can offer prompts and suggestions based on the documented clinical information. These prompts help guide clinicians in providing thorough and specific documentation, ensuring that the necessary details for code assignment are captured.
Improved clinical documentation benefits healthcare organizations in various ways. Accurate and detailed documentation supports better communication among healthcare providers, leading to enhanced care coordination and patient safety. It also facilitates more accurate and timely coding, contributing to appropriate reimbursement and minimizing the risk of claim denials. Furthermore, high-quality documentation supports comprehensive healthcare data analysis, enabling researchers and policymakers to generate meaningful insights and make informed decisions.
Coding Accuracy and Compliance

Importance of accurate coding
Accurate coding is paramount in healthcare for several reasons. Firstly, accurate coding ensures that the patient’s medical information is precisely captured and represented in their health records. This facilitates effective communication among healthcare providers, ensuring a clear understanding of the patient’s conditions, treatments, and outcomes.
Accurate coding is also crucial for the appropriate reimbursement of healthcare services. Insurance payers rely on coded data to process claims and determine reimbursement amounts. Incorrect or incomplete coding can lead to claim denials or underpayment, negatively impacting healthcare organizations’ financial sustainability.
Moreover, accurate coding supports population health management, research, and quality improvement initiatives. Coded data serves as a foundation for healthcare data analysis and research, enabling the identification of trends, evaluation of treatment outcomes, and measurement of healthcare quality indicators. Accurate coding promotes the reliability and validity of these analyses, leading to evidence-based decision-making and improved patient care.
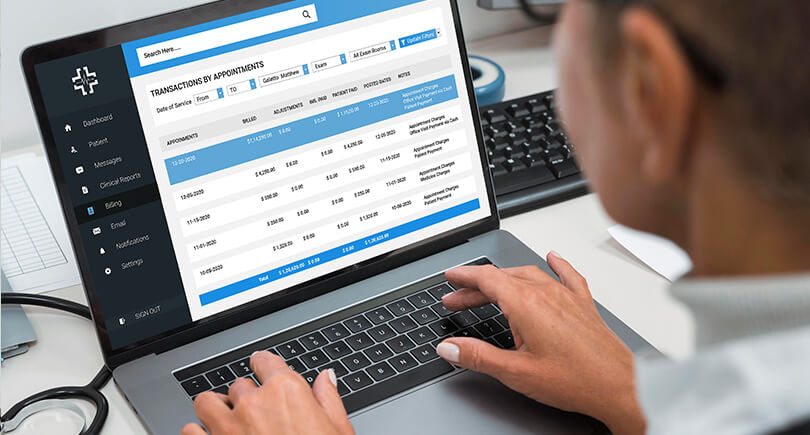
Reimbursement and billing
Accurate coding plays a vital role in the reimbursement and billing processes in healthcare. Insurance payers rely on coded data to process claims, determine appropriate reimbursement amounts, and prevent fraudulent or improper billing practices.
By assigning the correct codes, accurate reimbursement can be obtained for the services provided. Detailed and specific codes allow insurance payers to understand the complexity and severity of a patient’s condition, leading to appropriate reimbursement.
However, inaccurate coding can result in claim denials or underpayment. When codes do not accurately reflect the patient’s condition or the provided services, insurance payers may consider the claim ineligible for reimbursement. This can lead to financial losses for healthcare organizations, as the costs of providing care are not adequately covered.
Ensuring coding accuracy and compliance with coding guidelines is, therefore, crucial for healthcare organizations to receive timely and proper reimbursement for the services they provide. Accurate coding practices, coupled with thorough documentation, support the integrity of the reimbursement process and foster sustainable financial operations.
Impact on healthcare data analysis
Accurate coding has a significant impact on healthcare data analysis, research, and quality improvement initiatives. Coded data serves as a cornerstone for these activities, providing reliable and valid information for analyzing healthcare trends, evaluating treatment outcomes, and measuring the quality of care.
Inaccurate or incomplete coding can lead to erroneous data analysis, affecting the validity and reliability of research findings. It can also hinder the identification of patterns and trends in population health, impeding efforts to improve public health interventions.
By contrast, accurate coding ensures that coded data accurately reflects the reality of patients’ health conditions, treatments, and outcomes. This promotes the validity and reliability of healthcare data analyses, leading to evidence-based research, informed decision-making, and improved patient care.
Additionally, accurate coding supports quality improvement initiatives, such as benchmarking, monitoring of healthcare outcomes, and identification of areas for improvement. Reliable coded data allows healthcare organizations to measure their performance, compare it to industry standards, and implement targeted improvements in care delivery processes.
Quality Improvement Initiatives
This image is property of emedia.rmit.edu.au.
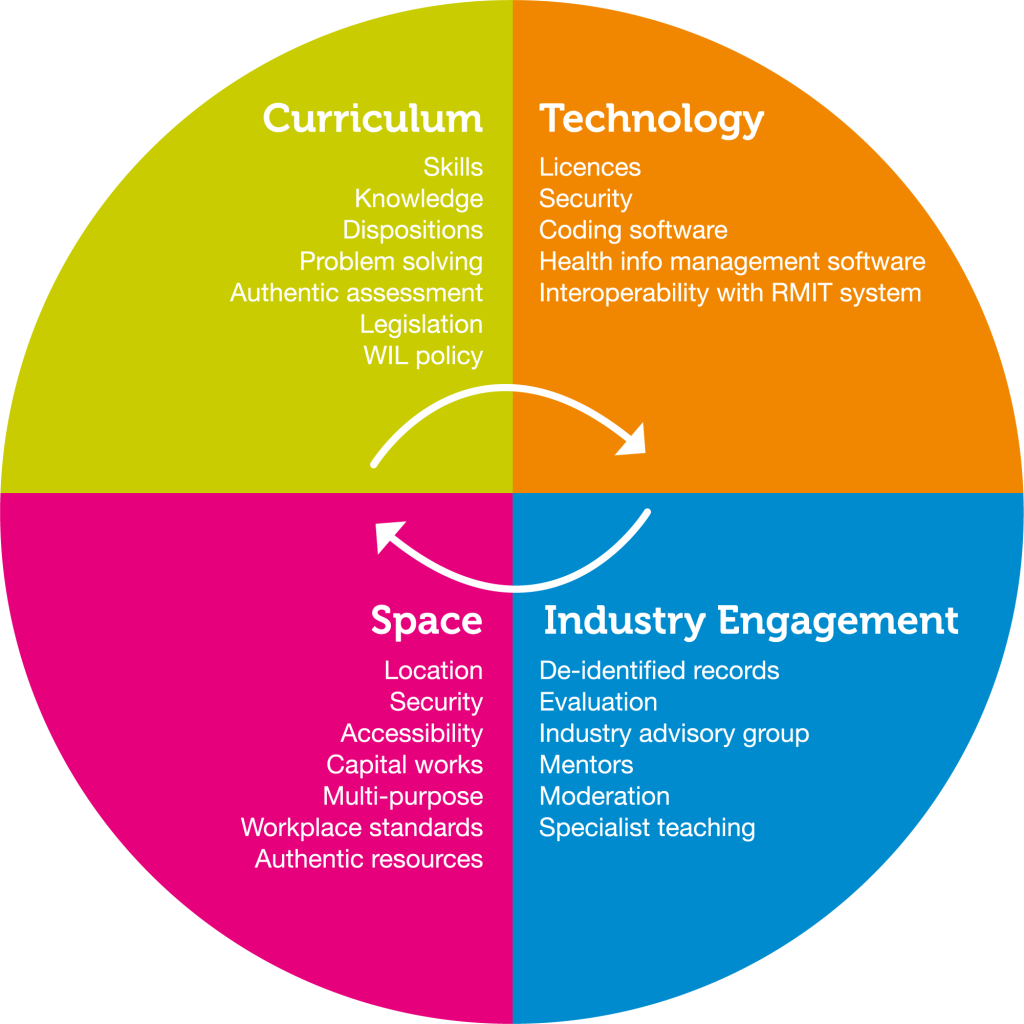
Using coding data for quality improvement
Clinical coding data can be utilized in quality improvement initiatives to enhance the overall quality and safety of patient care. Coded data provides valuable insights into healthcare processes and outcomes, allowing organizations to identify areas for improvement and implement evidence-based interventions.
By analyzing coded data, healthcare organizations can identify patterns of care variations, assess adherence to best practices, and identify potential gaps or opportunities for improvement. This analysis can guide the development of targeted quality improvement initiatives, such as clinical pathway optimization, workflow redesign, or the implementation of decision support systems.
Using coded data for quality improvement also enables healthcare organizations to measure the impact of these initiatives. By monitoring coded data before and after the implementation of interventions, organizations can assess if the intended improvements have been achieved and make further adjustments if necessary.
Clinical quality measures
Clinical quality measures (CQMs) are tools used to assess and measure the quality of healthcare delivery. CQMs enable healthcare organizations to monitor and evaluate their performance in specific areas, such as patient safety, effective clinical care, care coordination, and patient experience.
Clinical coding data is critical in the calculation and reporting of CQMs. Coded data provides the necessary information to measure adherence to evidence-based guidelines, track patient outcomes, and assess the efficiency and effectiveness of care delivery.
CQMs derived from coded data allow healthcare organizations to compare their performance against benchmarks and national standards. This comparison provides organizations with valuable insights into their performance relative to peers, identifies areas for improvement, and supports efforts to deliver high-quality, patient-centered care.
Clinical decision support systems
Clinical decision support systems (CDSS) utilize clinical coding data to provide timely and evidence-based recommendations to healthcare professionals at the point of care. These systems analyze coded data from patient records, guidelines, and clinical knowledge databases to offer insights and suggestions for decision-making.
By leveraging coded data, CDSS can provide alerts and reminders for preventive care, suggest appropriate treatment options, and facilitate the identification of potential drug interactions or adverse reactions. This enables healthcare professionals to make informed and patient-specific decisions, leading to improved clinical outcomes and patient safety.
CDSS can also aid in coding accuracy and compliance. By incorporating coding guidelines and automated code suggestion functionalities, CDSS can assist clinical coders in assigning accurate and specific codes, minimizing the risk of coding errors and supporting compliance with coding standards.
Future Trends in Clinical Coding Systems

Advancements in natural language processing
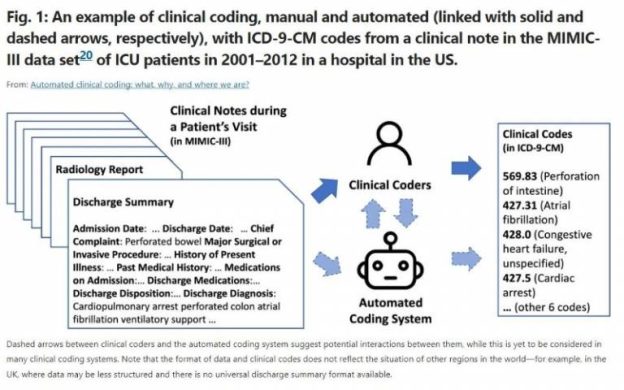
Natural language processing (NLP) is a field of technology that focuses on the interaction between computers and human language. In the context of clinical coding, NLP has the potential to revolutionize the coding process by automating code assignment based on clinician-entered narrative documentation.
Advanced NLP algorithms can analyze unstructured clinical narratives and extract relevant information to generate coded data. This technology eliminates the need for manual coding in many cases, reducing the burden on clinical coders and enhancing coding speed and efficiency.
NLP-powered coding solutions are continuously evolving and maturing, with ongoing efforts to improve accuracy and increase the range of clinical scenarios that can be effectively coded using this technology. As NLP technologies continue to advance, the coding process may become more streamlined and standardized, ultimately leading to improved coding accuracy and reduced coding workload.
Artificial intelligence and machine learning
Artificial intelligence (AI) and machine learning (ML) have the potential to transform clinical coding by leveraging powerful algorithms to analyze vast amounts of healthcare data. AI and ML models can be trained using coded data to identify patterns, predict missing codes, and suggest accurate codes based on clinical documentation.
By leveraging AI and ML technologies, healthcare organizations can improve coding accuracy, efficiency, and compliance. These technologies can learn from historical coded data and adapt to changing coding guidelines, making them valuable tools that coders can rely on for efficient and accurate code assignment.
AI and ML models can also enhance coding audits by automating the identification of potential coding errors or discrepancies. Through continuous learning and feedback loops, these systems can improve the accuracy of coding audits, ensuring a higher level of compliance and quality in coded data.
Utilizing big data analytics for coding
The integration of clinical coding systems with big data analytics capabilities presents immense opportunities for healthcare organizations. Big data analytics involves mining and analyzing large volumes of clinical and administrative data to extract meaningful insights and drive evidence-based decision-making.
By combining coded data with other healthcare data sources, such as clinical notes, laboratory results, and claims data, healthcare organizations can gain a comprehensive understanding of patient populations, treatment outcomes, and healthcare utilization patterns. This holistic view of healthcare data can inform policy-making, resource allocation, and the design of preventive interventions.
The integration of big data analytics with clinical coding systems can also enhance predictive modeling and risk stratification. By leveraging coded data, organizations can develop models to predict disease progression, identify high-risk patient cohorts, and allocate resources strategically to mitigate potential adverse outcomes.
As healthcare organizations continue to adopt and utilize clinical coding systems, the adoption of big data analytics and advanced analytical techniques will become increasingly essential. The combination of coded data and big data analytics holds the potential to revolutionize population health management, support precision medicine initiatives, and improve overall healthcare quality and outcomes.
In conclusion, clinical coding systems play a critical role in accurately documenting and communicating medical data in the healthcare industry. These systems, such as ICD-10, ICD-11, SNOMED CT, and HCPCS, provide standardized codes that enable consistent and uniform classification of diagnoses, procedures, and other medical information.
Clinical coding systems are vital for reimbursement processes, healthcare data analysis, and improving care coordination. Accurate coding is essential for appropriate reimbursement, while coding audits help maintain coding integrity. The integration of coding systems in EHRs enhances documentation, interoperability, and clinical decision-making.
Clinical coders have significant responsibilities in accurately representing healthcare data through coding. Ongoing education, training, and skills in medical terminology and coding systems are crucial for clinical coders. Coding accuracy and compliance impact reimbursement, billing, and healthcare data analysis, supporting evidence-based decision-making and quality improvement initiatives.
The future of clinical coding systems holds promise, with advancements in natural language processing, AI, ML, and big data analytics. These technologies can automate code assignment, improve accuracy, and provide valuable insights for improving healthcare delivery and patient outcomes. As the healthcare landscape evolves, clinical coding systems will continue to play a crucial role in ensuring accurate data capture and analysis, ultimately enhancing patient care and driving healthcare improvements.