Medical coding certifications play a critical role in the healthcare industry. They ensure accurate and efficient documentation of patient medical records, which ultimately impacts healthcare reimbursement and quality of care. In this article, you will explore the various types of medical coding certifications available and gain an understanding of their significance in the field. Whether you are a medical professional looking to expand your career prospects or an individual interested in pursuing a rewarding healthcare occupation, this article will provide valuable insights into the different pathways available to establish your expertise in medical coding.
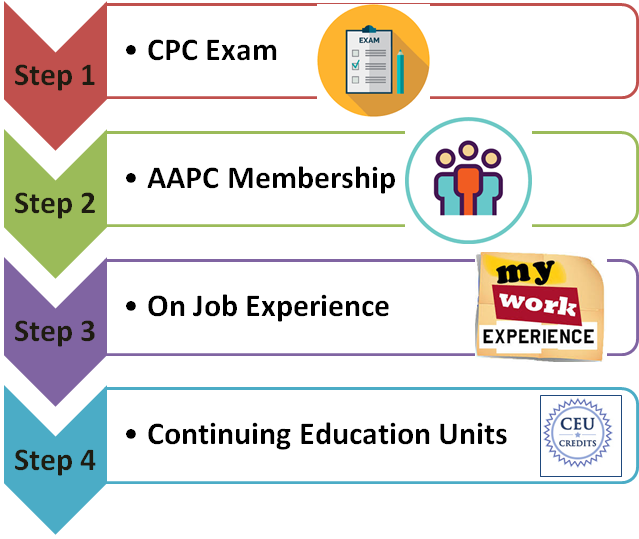
Certified Professional Coder (CPC)
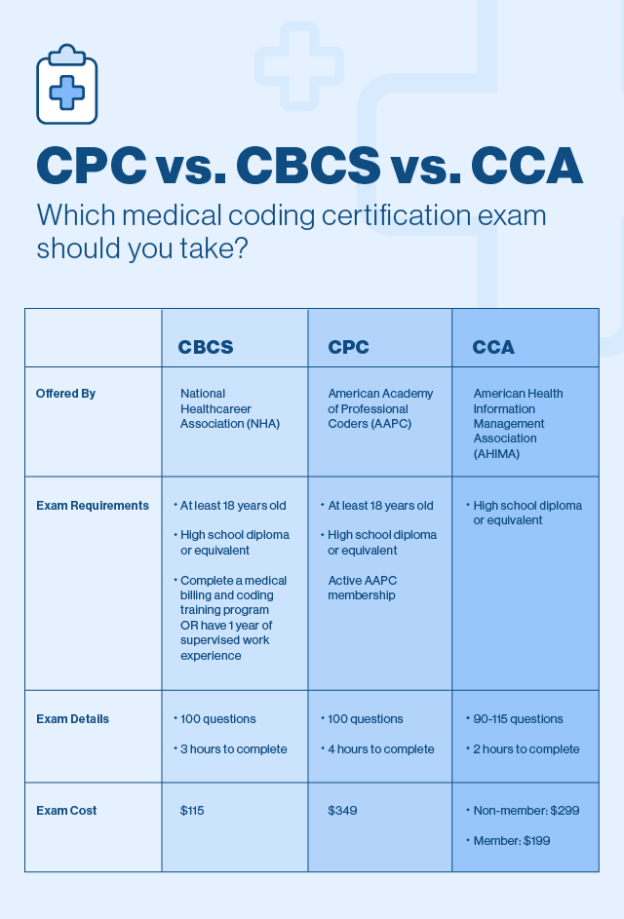
The Certified Professional Coder (CPC) certification is a widely recognized credential in the field of medical coding. This certification is offered by the American Academy of Professional Coders (AAPC) and signifies that an individual possesses a strong knowledge and understanding of medical coding practices.
Requirements for CPC certification
To be eligible for the CPC certification, you must meet certain requirements set by the AAPC. These requirements include having at least two years of professional coding experience, along with completing a coding education program.
Exam details for CPC certification
The CPC certification exam is a rigorous test that evaluates your knowledge of medical coding guidelines, procedures, and regulations. The exam consists of multiple-choice questions and covers various topics such as anatomy, medical terminology, and coding guidelines. To pass the exam, you must demonstrate a thorough understanding of these topics and achieve a minimum passing score.
Renewal process for CPC certification
Once you have obtained your CPC certification, you will need to renew it periodically to maintain your certified status. The renewal process involves completing continuing education units (CEUs) and submitting an application for renewal to the AAPC. By staying up to date with the latest coding practices, you can ensure that your CPC certification remains valid and relevant.
Certified Coding Specialist (CCS)
The Certified Coding Specialist (CCS) certification is offered by the American Health Information Management Association (AHIMA) and focuses on hospital inpatient coding. This certification demonstrates a high level of proficiency in coding for various medical conditions and treatments.
Requirements for CCS certification
To qualify for the CCS certification, you must meet certain requirements outlined by AHIMA. These requirements include having a strong foundation in medical coding, completion of an accredited coding program, and a minimum of two years of coding experience in a hospital setting.
Exam details for CCS certification
The CCS certification exam covers a wide range of topics related to hospital inpatient coding. The exam consists of multiple-choice questions and medical scenario-based questions that assess your ability to accurately assign diagnosis and procedure codes. Passing the CCS exam requires a deep understanding of coding guidelines, coding systems, and medical terminology specific to inpatient coding.
Renewal process for CCS certification
Similar to other certifications, the CCS certification needs to be renewed periodically to maintain its validity. To renew your CCS certification, you must complete a certain number of continuing education credits related to medical coding. AHIMA provides various resources and educational opportunities to help certified professionals fulfill their renewal requirements.
Certified Coding Associate (CCA)
The Certified Coding Associate (CCA) certification, also offered by AHIMA, is an entry-level certification for individuals who are starting their career in medical coding. This certification validates the foundational coding skills necessary for accurate code assignment.
Requirements for CCA certification
The requirements for CCA certification are relatively less rigorous compared to other certifications. However, you must still possess a basic understanding of medical coding and complete a coding education program to be eligible for the CCA exam.
Exam details for CCA certification
The CCA certification exam assesses your proficiency in basic coding skills, such as assigning diagnosis codes, procedure codes, and applying coding guidelines. The exam includes multiple-choice questions and covers topics such as medical terminology, anatomy, and coding guidelines. It is designed to test your ability to accurately code medical records.
Renewal process for CCA certification
To maintain your CCA certification, you will need to renew it periodically. The renewal process for CCA certification involves earning a certain number of CEUs related to medical coding. By keeping up with ongoing education and advancements in coding practices, you can ensure that your CCA certification remains valid.
Certified Professional Biller (CPB)
The Certified Professional Biller (CPB) certification, offered by AAPC, focuses specifically on medical billing. This certification validates your expertise in understanding the complex billing processes involved in healthcare reimbursement.
Requirements for CPB certification
To be eligible for the CPB certification, you must have at least two years of professional experience in medical billing or coding. Additionally, completing a billing education program is required to meet the certification requirements.
Exam details for CPB certification
The CPB certification exam evaluates your knowledge of medical billing practices, healthcare reimbursement systems, and various regulations related to billing and coding. The exam consists of multiple-choice questions that assess your understanding of different billing scenarios and your ability to accurately navigate billing guidelines.
Renewal process for CPB certification
To maintain your CPB certification, you need to renew it periodically through the AAPC. This involves completing a certain number of CEUs related to medical billing and submitting a renewal application. By staying updated with the evolving regulations and practices in medical billing, you can demonstrate your commitment to excellence in this field.
Certified Outpatient Coder (COC)
The Certified Outpatient Coder (COC) certification, offered by AAPC, is specifically focused on outpatient coding. This certification demonstrates your competence in accurately assigning codes for procedures and services provided in outpatient settings.
Requirements for COC certification
To be eligible for the COC certification, you must have at least two years of professional experience coding in an outpatient setting. Additionally, you are required to complete a coding education program to meet the necessary certification requirements.
Exam details for COC certification
The COC certification exam evaluates your proficiency in outpatient coding, with a focus on coding guidelines and rules specific to outpatient procedures and services. The exam includes multiple-choice questions and task-based scenarios that test your ability to accurately assign codes for various outpatient encounters.
Renewal process for COC certification
To maintain your COC certification, you must renew it periodically through the AAPC. The renewal process involves completing a certain number of CEUs in the field of outpatient coding and submitting a renewal application. This ensures that your knowledge and skills in outpatient coding remain up to date.
Certified Inpatient Coder (CIC)
The Certified Inpatient Coder (CIC) certification, also offered by AAPC, focuses on the specialized skillset required for accurate inpatient coding. This certification demonstrates your expertise in assigning codes for diagnoses and procedures in a hospital inpatient setting.
Requirements for CIC certification
To be eligible for the CIC certification, you must have at least two years of professional experience coding in a hospital inpatient setting. Additionally, you are required to complete a coding education program to meet the necessary certification requirements.
Exam details for CIC certification
The CIC certification exam evaluates your knowledge and skills in inpatient coding, with a particular focus on coding guidelines, documentation requirements, and medical terminology specific to hospital inpatient procedures. The exam includes multiple-choice questions and case scenarios that test your ability to accurately assign codes and capture information from complex medical records.
Renewal process for CIC certification
To maintain your CIC certification, you must renew it periodically through the AAPC. This involves completing a certain number of CEUs focused on inpatient coding and submitting a renewal application. By staying updated with the latest advancements and guidelines in hospital inpatient coding, you can ensure the continued validity of your certification.
This image is property of www.pharmaknowledgecentre.com.
Certified Professional Medical Auditor (CPMA)
The Certified Professional Medical Auditor (CPMA) certification, offered by AAPC, is designed for professionals who specialize in medical auditing. This certification validates your expertise in evaluating and assessing compliance with coding and billing regulations.
Requirements for CPMA certification
To be eligible for the CPMA certification, you must have at least two years of professional experience in medical auditing or a related field. Additionally, completing a medical auditing education program is required to meet the certification requirements.
Exam details for CPMA certification
The CPMA certification exam evaluates your understanding of auditing principles, medical coding regulations, and compliance guidelines related to medical billing and coding. The exam includes multiple-choice questions and case scenarios that test your ability to identify inaccuracies or discrepancies in coding and billing practices.
Renewal process for CPMA certification
To maintain your CPMA certification, you must renew it periodically through the AAPC. This involves completing a certain number of CEUs focused on medical auditing and submitting a renewal application. By staying informed about the changing regulatory environment and best practices in medical auditing, you can demonstrate your ongoing commitment to maintaining the highest standards in this field.
Certified Risk Adjustment Coder (CRC)
The Certified Risk Adjustment Coder (CRC) certification, offered by AAPC, specializes in coding for risk adjustment models in healthcare. This certification demonstrates your ability to accurately assign diagnosis codes based on the complexity of patients’ medical conditions.
Requirements for CRC certification
To be eligible for the CRC certification, you must have at least one year of experience in medical coding with a focus on risk adjustment coding. Additionally, completing a risk adjustment coding education program is required to meet the certification requirements.
Exam details for CRC certification
The CRC certification exam evaluates your proficiency in assigning diagnosis codes based on risk adjustment models, such as the Hierarchical Condition Category (HCC) system. The exam includes multiple-choice questions that test your knowledge of medical conditions, coding guidelines, and documentation requirements specific to risk adjustment coding.
Renewal process for CRC certification
To maintain your CRC certification, you must renew it periodically through the AAPC. This involves completing a certain number of CEUs focused on risk adjustment coding and submitting a renewal application. By staying up to date with the evolving risk adjustment models and coding guidelines, you can ensure the continued validity of your certification.
This image is property of lh6.googleusercontent.com.
Certified Professional Compliance Officer (CPCO)
The Certified Professional Compliance Officer (CPCO) certification, offered by AAPC, is designed for professionals who specialize in healthcare compliance. This certification demonstrates your expertise in ensuring adherence to legal and ethical standards in medical coding and billing practices.
Requirements for CPCO certification
To be eligible for the CPCO certification, you must have at least two years of professional experience in healthcare compliance or a related field. Additionally, completing a compliance officer education program is required to meet the certification requirements.
Exam details for CPCO certification
The CPCO certification exam evaluates your understanding of healthcare compliance regulations, audit and investigation processes, and ethical standards in medical coding and billing. The exam includes multiple-choice questions that assess your knowledge of laws and regulations, risk assessment techniques, and compliance program implementation.
Renewal process for CPCO certification
To maintain your CPCO certification, you must renew it periodically through the AAPC. This involves completing a certain number of CEUs focused on healthcare compliance and submitting a renewal application. By staying informed about the latest regulatory changes and best practices in healthcare compliance, you can effectively contribute to maintaining ethical and compliant coding and billing processes.
Certified Professional Medical Coding Instructor (CPC-I)
The Certified Professional Medical Coding Instructor (CPC-I) certification, offered by AAPC, is designed for professionals who have extensive experience in medical coding and wish to impart their knowledge through teaching and instruction.
Requirements for CPC-I certification
To be eligible for the CPC-I certification, you must possess a minimum of five years of coding experience and hold a current AAPC certification, such as the CPC. Additionally, you must demonstrate teaching experience or completion of a teaching program to meet the certification requirements.
Exam details for CPC-I certification
The CPC-I certification requires completion of a detailed application and submission of supporting documentation to AAPC. This certification does not involve a specific exam, but rather focuses on evaluating your experience, teaching qualifications, and commitment to professional development.
Renewal process for CPC-I certification
To maintain your CPC-I certification, you must renew it periodically through the AAPC. This involves meeting specific requirements related to teaching experience, continuing professional development, and adherence to the AAPC Code of Ethics. By continually expanding your knowledge and refining your teaching skills, you can effectively contribute to the development and advancement of future medical coders.
In conclusion, the field of medical coding offers a variety of certifications that cater to different specialties and job roles. Whether you are interested in outpatient or inpatient coding, medical billing, auditing, compliance, or teaching, there are certifications available to validate your expertise and enhance your career prospects. By obtaining and maintaining these certifications, you can demonstrate your commitment to professional growth and excellence in the field of medical coding.
This image is property of medsitnexus.com.