In the realm of medical billing, understanding the intricacies of the billing cycle is essential. During this time, healthcare providers and medical billing professionals work collaboratively to ensure accurate and timely payment for services rendered. From the submission of claims to the processing of payments, the billing cycle encompasses a series of crucial steps that directly impact the financial stability of healthcare organizations. This article aims to shed light on the significance of the billing cycle within the realm of medical billing and highlight the various stages involved in this intricate process. Whether you are an aspiring medical biller or a healthcare provider seeking insight into the financial operations of your practice, grasping the fundamentals of the billing cycle is paramount to navigating the ever-evolving landscape of healthcare reimbursement.
Understanding the Basics of Medical Billing
Definition of Medical Billing
Medical billing refers to the process of submitting and following up on claims with health insurance companies in order to receive payment for services provided by healthcare professionals. It involves generating accurate invoices, documenting patient records, and communicating with insurance providers to ensure reimbursement.
Importance of Medical Billing
Effective medical billing is crucial for healthcare providers and facilities as it serves as the financial backbone of the healthcare industry. It ensures the smooth flow of revenue by transforming healthcare services into monetary transactions. Proper medical billing not only helps healthcare providers maintain their financial stability but also enables them to continue delivering quality care to patients.
Key Elements of Medical Billing
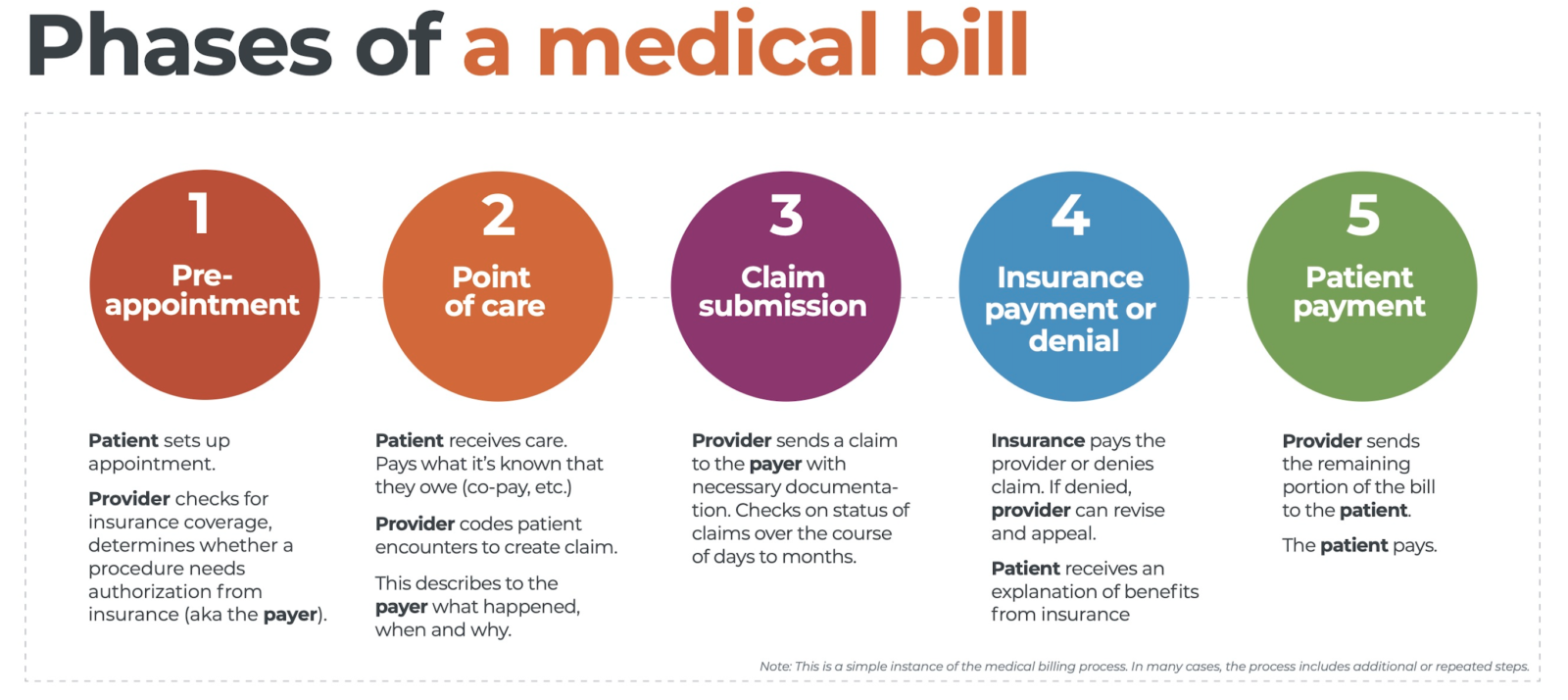
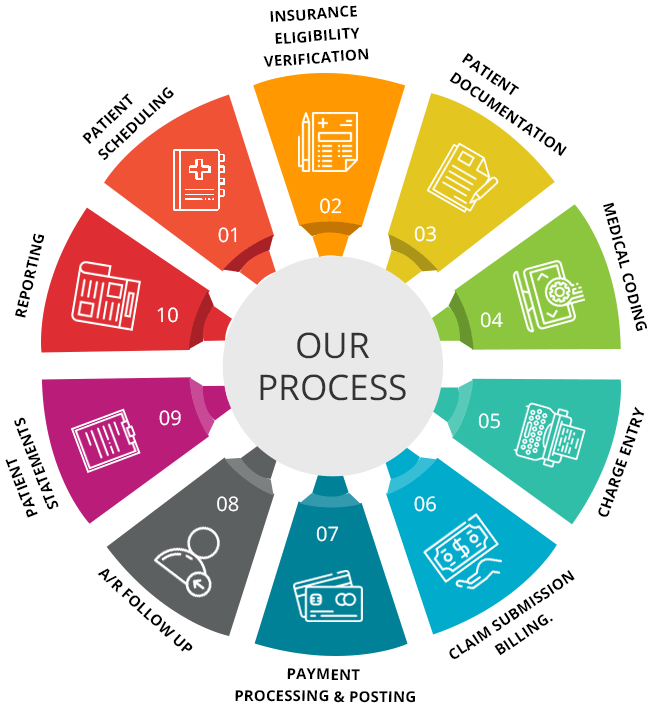
Several key elements are involved in medical billing. These include patient registration, insurance verification, coding and documentation, charge entry, claim submission, payment posting, denial management, patient statements, and follow-up and collections. Each element plays an important role in the overall billing process, contributing to a seamless and efficient revenue cycle.
Exploring the Billing Cycle in Medical Billing
This image is property of assets.website-files.com.
Definition of Billing Cycle
The billing cycle in medical billing refers to the complete series of steps involved in processing and managing healthcare claims from the initiation of services to the receipt of payment or resolution of any disputes. It encompasses various stages, each with its specific tasks and responsibilities, to ensure accurate billing and prompt reimbursement.
Role of Billing Cycle in Medical Billing
The billing cycle is essential in medical billing as it outlines the systematic flow of information and actions required to complete the billing process. It helps healthcare providers maintain financial stability by ensuring accurate invoicing, timely submissions, and efficient follow-up on claims. By following the billing cycle, healthcare providers can maximize their revenue potential and minimize potential delays or denials in the reimbursement process.
Typical Duration of Billing Cycle
The duration of the billing cycle in medical billing varies depending on several factors, including the size of the healthcare facility, the complexity of services provided, and the efficiency of the billing system. On average, the billing cycle can range from a few weeks to a couple of months. However, it is important to note that the duration may vary significantly based on external factors such as insurance company policies and claim review processes.
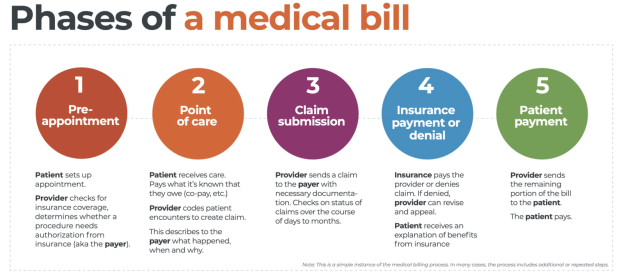
Different Stages of the Billing Cycle

Patient Registration
The first stage of the billing cycle is patient registration. During this process, accurate and comprehensive patient data is collected, including personal information, medical history, insurance coverage, and contact details. This information is crucial for verifying eligibility, determining insurance coverage, and ensuring proper billing and reimbursement.
Insurance Verification
Insurance verification is a vital step in the billing cycle as it ensures that the patient’s insurance coverage is active and verifies their benefits and eligibility for specific medical services. This stage involves contacting the insurance provider, providing necessary patient information, and obtaining pre-authorization if required for certain services. Insurance verification helps prevent claim denials and reduces the risk of non-payment or delayed reimbursement.
Coding and Documentation
Coding and documentation play a critical role in accurately representing the services provided by healthcare professionals. Medical coders assign specific procedure and diagnosis codes based on the patient’s medical records, ensuring compliance with coding standards and regulations. Accurate coding and comprehensive documentation not only facilitate claims processing but also enable healthcare providers to demonstrate the medical necessity of the services rendered.
Charge Entry
Charge entry involves the submission of charges for the services provided by healthcare professionals. This stage requires careful verification of charge information, such as the type of service, the date of service, and the corresponding codes. Accuracy in charge entry ensures that the billed services align with the services delivered, and it enables proper reimbursement from insurance providers.
Claim Submission
Claim submission involves preparing and transmitting claims to the appropriate insurance companies. This stage requires attaching necessary supporting documentation, such as medical records, test results, and invoices, to substantiate the services rendered. Proper claim submission ensures that all relevant information is provided to insurance companies, expediting the processing and reimbursement of claims.
Payment Posting
Payment posting involves the recording and allocation of payments received from insurance companies or patients’ out-of-pocket payments. It also includes applying adjustments or write-offs as necessary. Accurate payment posting helps healthcare providers track their revenues, identify any discrepancies, and reconcile accounts, ensuring that payments are appropriately allocated and documented.
Denial Management
Denial management refers to the process of addressing and resolving claim denials or rejections. This stage involves investigating the reasons for denial, rectifying any errors or discrepancies, and resubmitting claims for reconsideration. Effective denial management is crucial for maximizing reimbursement rates and preventing unnecessary revenue loss.
Patient Statements
Patient statements are an essential part of the billing cycle as they inform patients about their financial responsibilities. These statements provide a breakdown of services rendered, insurance coverage, and any outstanding balances. Clear and timely patient statements promote transparency, allowing patients to understand their financial obligations and make payments promptly.
Follow-up and Collections
Follow-up and collections involve monitoring outstanding balances, contacting patients for payment, and utilizing collection agencies if necessary. This stage ensures that unpaid or partially paid claims are pursued and resolved, maximizing the chances of receiving the full payment for services rendered. Effective follow-up and collections significantly contribute to the financial stability of healthcare providers and facilitate the management of accounts receivable.
In conclusion, understanding the basics of medical billing is crucial for healthcare providers and facilities to ensure accurate and timely reimbursement for the services they provide. By comprehending the various stages of the billing cycle and their significance, healthcare professionals can establish efficient billing practices, minimize claim denials, and maintain their financial stability while delivering quality care to their patients.