In the realm of healthcare documentation and billing, the terms “medical coding” and “clinical coding” are often used interchangeably. However, it is crucial to understand whether these two terms are indeed synonymous. This article aims to explore the similarities and differences between medical coding and clinical coding, shedding light on their distinctive roles and functions within the healthcare industry. By providing a comprehensive understanding of these coding practices, healthcare professionals can enhance their knowledge and contribute to the efficient and accurate processing of vital medical information.
Definition of Medical Coding
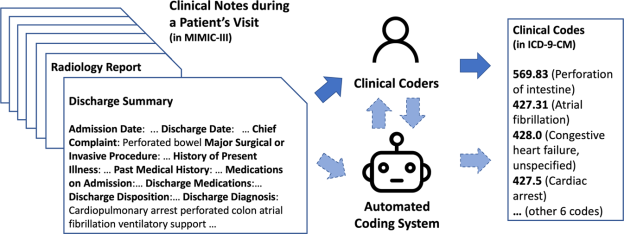
Medical coding is the process of translating medical procedures, diagnoses, and other pertinent healthcare services into universally recognized alphanumeric codes. These codes are used for various purposes, including reimbursement, tracking of diseases and healthcare trends, and statistical analysis. Medical coders play a crucial role in the healthcare system by ensuring accurate and consistent coding, which is essential for effective communication and management of patient care.
Definition of Clinical Coding
Clinical coding, on the other hand, refers to the process of translating clinical information, such as diagnoses and treatments, into alphanumeric codes. These codes are used primarily for clinical and research purposes, including clinical audits, healthcare planning, and epidemiological studies. Clinical coders work closely with healthcare professionals to ensure that the documentation is complete and accurately reflects the patient’s condition and the care provided.
Differences Between Medical Coding and Clinical Coding

Scope and Focus
Medical coding encompasses a broader range of healthcare services, including procedures, diagnoses, laboratory tests, medications, and more. It focuses on coding for administrative and financial purposes, such as insurance claims and billing. Clinical coding, on the other hand, is more focused on documenting the clinical aspects of patient care, including diagnoses, treatments, and outcomes. Its primary aim is to provide accurate and reliable information for clinical decision-making and healthcare management.
Purpose
The purpose of medical coding is mainly related to reimbursement and financial transactions. The codes assigned to medical services help determine the amount of payment that healthcare providers receive from insurance companies or government programs. In contrast, clinical coding serves a broader purpose beyond financial transactions. It aims to facilitate clinical research, improve patient outcomes, support epidemiological studies, and enhance overall healthcare quality and safety.
Healthcare Setting
Medical coding is primarily performed in healthcare administrative settings, such as hospitals, clinics, and insurance companies. Medical coders analyze the documentation from healthcare providers and assign appropriate codes to the services provided. Clinical coding, on the other hand, is usually done within the clinical setting, such as hospitals and other healthcare facilities. Clinical coders work closely with healthcare professionals, including doctors and nurses, to translate clinical information accurately.
Skills and Training
Medical coding requires proficiency in medical terminology, anatomy, and physiology, as well as knowledge of healthcare coding systems, such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT). Medical coders typically undergo specific training programs or obtain certification to develop the necessary skills. Clinical coding also requires strong knowledge of medical terminology and coding systems but places more emphasis on understanding clinical concepts and healthcare processes. Clinical coders usually have a healthcare background, such as nursing or health information management, and receive specialized training in clinical coding.
Coding Systems Used
Both medical coding and clinical coding rely on standardized coding systems to translate healthcare information into codes. The International Classification of Diseases (ICD), developed by the World Health Organization (WHO), is used worldwide for coding diagnoses and diseases. Current Procedural Terminology (CPT), developed by the American Medical Association (AMA), is commonly used for coding medical procedures and services. Additionally, there are other coding systems specific to certain specialties, such as the Healthcare Common Procedure Coding System (HCPCS) used for Medicare billing in the United States. The choice of coding systems may vary depending on the purpose and context of coding.
Responsibilities
Medical coders are responsible for reviewing medical documentation, assigning appropriate codes, and ensuring accuracy and compliance with coding guidelines and regulations. They also play a vital role in identifying and reporting coding errors or inconsistencies. In contrast, clinical coders focus more on the clinical aspects of coding, including verifying the accuracy and completeness of clinical documentation, coding complex cases, and providing feedback to healthcare professionals to improve documentation quality and coding practices.
Career Opportunities
Both medical coding and clinical coding offer various career opportunities within the healthcare industry. Medical coders can work in hospitals, clinics, insurance companies, or as independent consultants or auditors. They may also specialize in specific coding areas, such as professional fee coding or outpatient coding. Clinical coders, on the other hand, typically work within the clinical setting, collaborating closely with healthcare professionals. They may also contribute to clinical research projects or work as coding educators or consultants.
Importance in Healthcare
Accurate and consistent coding is critical for effective healthcare management and decision-making. Both medical coding and clinical coding contribute to the quality of healthcare data, which is essential for research, clinical audits, and healthcare planning. Proper coding ensures that healthcare services are appropriately reimbursed, facilitates accurate statistical analysis, and enables tracking and monitoring of diseases and healthcare trends. It also supports the exchange of information between healthcare providers, insurance companies, and government agencies, allowing for better coordination and continuity of care.
Regulatory Requirement
Medical coding is heavily regulated, particularly in the United States, where coding accuracy directly impacts reimbursement from government programs, such as Medicare and Medicaid. Coding guidelines and regulations are set by various organizations, including the Centers for Medicare and Medicaid Services (CMS) and the American Health Information Management Association (AHIMA). Clinical coding may also have regulatory requirements, depending on the country or healthcare system. Compliance with coding standards and guidelines is crucial to ensure accurate and consistent coding practices and to avoid penalties or legal issues.
Coding Accuracy and Compliance
Both medical coding and clinical coding require a high level of accuracy and compliance with coding guidelines and regulations. Inaccurate coding can have significant consequences, including incorrect billing, compromised patient care, and potential legal ramifications. Healthcare organizations strive to achieve coding accuracy through regular audits, education and training programs, and the use of coding compliance tools. Additionally, ongoing communication between coders, healthcare providers, and clinical documentation improvement specialists helps enhance coding accuracy and ensures the integrity of healthcare data.
Similarities Between Medical Coding and Clinical Coding

Coding Terminology
Both medical coding and clinical coding rely on a standardized terminology to describe medical conditions, procedures, and other healthcare services. This ensures consistency and clarity in communication and facilitates the accurate translation of clinical information into codes. Common medical terminology, such as anatomical terms, disease names, and medically accepted abbreviations, is used in both coding disciplines. This shared use of coding terminology allows for interoperability and seamless data exchange between medical and clinical coding systems.
Healthcare Documentation
Both medical coding and clinical coding heavily depend on accurate and comprehensive healthcare documentation. Clear and detailed documentation is essential to capture the necessary information for coding and to ensure that the coded data accurately represents the patient’s condition and the care provided. Incomplete or ambiguous documentation can lead to coding errors, inaccurate reimbursement, and compromised patient care. Both medical coders and clinical coders work closely with healthcare professionals to clarify documentation and ensure its accuracy and completeness.
Conclusion
In conclusion, while medical coding and clinical coding share certain similarities, they have distinct differences in scope, purpose, setting, skills required, and career opportunities. Medical coding focuses more on administrative and financial aspects of coding, such as reimbursement and insurance claims. Clinical coding, on the other hand, centers on translating clinical information for research, healthcare planning, and clinical decision-making. Both coding disciplines contribute to the accuracy and integrity of healthcare data and play crucial roles in the management and improvement of healthcare services. Compliance with coding guidelines and regulations, as well as ongoing education and communication, are paramount to ensure accurate and reliable coding practices in both medical coding and clinical coding.