Clinical coding is a crucial component of the healthcare system, as it ensures accurate and efficient record-keeping of patients’ medical information. However, the question arises: is clinical coding an easy task? In this article, we will explore the intricacies of clinical coding and shed light on the challenges and complexities associated with this profession. By examining the skills required, the ever-evolving nature of medical codes, and the growing demand for accurate coding, we aim to provide a comprehensive understanding of the true difficulty behind clinical coding.
The Basics of Clinical Coding
What is clinical coding?
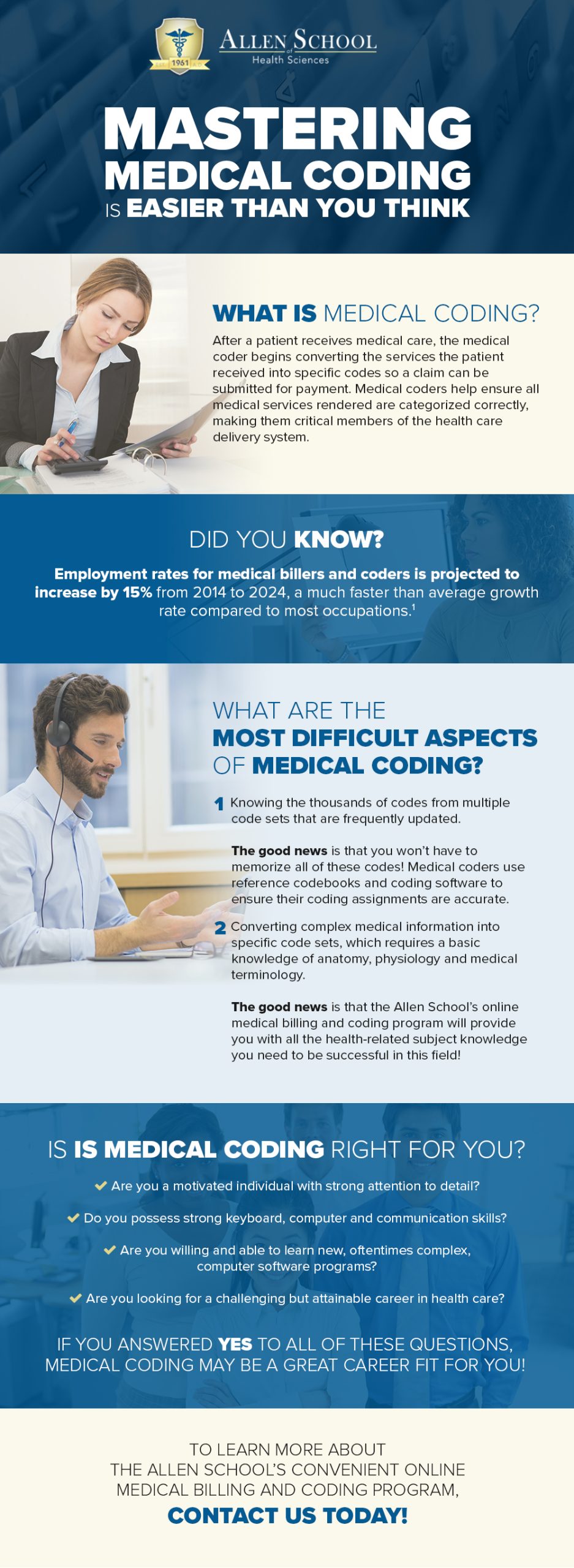
Clinical coding is the process of translating medical information into standardized numeric or alphanumeric codes. These codes are used to represent various diagnoses, procedures, and treatments in healthcare settings. By assigning codes to patient data, clinical coders ensure that accurate and consistent information is recorded and can be utilized for various purposes, such as billing, research, and analysis.
Why is clinical coding important?
Clinical coding plays a vital role in healthcare as it facilitates effective communication, data analysis, and decision-making. Accurate coding ensures that patient information is correctly documented, allowing for proper billing and reimbursement. It also enables healthcare providers to track and analyze health trends, identify areas for improvement, and make informed decisions for patient care and population health management.
What are the key goals of clinical coding?
The primary goals of clinical coding are to ensure accuracy, consistency, and completeness of patient data. Coding professionals strive to assign codes that accurately reflect the diagnoses, procedures, and treatments documented in medical records. Consistency in coding practices is essential to enable meaningful comparisons and analysis of healthcare data. Completeness of coding ensures that no relevant information is missed, allowing for comprehensive patient care and accurate data analysis.
Common coding systems used in clinical coding
In clinical coding, several coding systems are commonly used, including the International Statistical Classification of Diseases and Related Health Problems (ICD), Current Procedural Terminology (CPT), and Healthcare Common Procedure Coding System (HCPCS). The ICD is primarily used for coding diagnoses, while CPT and HCPCS are used for coding procedures and services. These coding systems provide a standardized language for healthcare professionals to communicate and record patient information consistently.
The role of clinical coders
Clinical coders are highly skilled professionals who play a key role in the accurate and efficient coding of medical information. They possess in-depth knowledge of coding systems, guidelines, and medical terminology. Clinical coders review medical records, interpret documentation, and assign appropriate codes to ensure accurate representation of patient diagnoses, procedures, and treatments. Their expertise supports billing accuracy, data analysis, and research efforts, making them an essential part of the healthcare team.
The Complexity of Clinical Coding

Understanding the intricacies of medical terminology
One of the complexities of clinical coding is the need to have a deep understanding of medical terminology. Medical terms can be complex and specific, requiring a coder to accurately interpret and translate them into corresponding codes. Coders must be familiar with terms related to anatomy, physiology, diseases, and medical procedures to properly assign codes that reflect the patient’s condition and treatment.
Dealing with multiple coding systems
Clinical coders often face the challenge of working with multiple coding systems, each with its own set of guidelines and conventions. The transition between different coding systems can be challenging, requiring coders to continuously update their knowledge and adapt their coding practices accordingly. Familiarity with the different coding systems and their corresponding guidelines is crucial for accurate and consistent coding.
Navigating complex coding guidelines
Coding guidelines can be complex and extensive, making it necessary for clinical coders to have a thorough understanding of these guidelines to ensure accurate coding. Guidelines provide instructions on code selection, sequencing, and documentation requirements, among other aspects. Coders must be able to interpret and apply these guidelines correctly to avoid coding errors and ensure compliance with coding standards.
The impact of coding errors
Coding errors can have significant consequences, both for patients and healthcare providers. Inaccurate coding can result in incorrect billing, leading to financial losses for healthcare organizations and potential challenges for patients in terms of insurance coverage. Inaccurate coding also hinders data analysis and research efforts, potentially impacting population health management. Therefore, clinical coders must strive for accuracy and attention to detail to prevent coding errors.
The need for ongoing training and education for coders
Given the ever-changing nature of healthcare and coding practices, clinical coders must engage in continuous learning and professional development. Staying updated with coding updates, guidelines, and industry trends is essential to maintain proficiency in clinical coding. Ongoing training and education programs provide opportunities for coders to enhance their skills and expand their knowledge, ensuring they can effectively navigate the complexity of clinical coding.
Challenges Faced by Clinical Coders

Keeping up with frequent coding updates
Clinical coders face the challenge of staying updated with frequent changes in coding rules, guidelines, and systems. Coding systems evolve to accommodate new medical procedures, diagnoses, and treatments, necessitating regular updates in coding practices. Coders must be proactive in accessing and learning from industry updates and staying informed through professional networks and resources to ensure accurate and compliant coding.
Handling ambiguous or incomplete documentation
Clinical coders often encounter ambiguous or incomplete documentation, which can make coding challenging. In such cases, coders may need to seek clarification from healthcare professionals or consult coding guidelines and references to make accurate coding decisions. Effective communication and collaboration between coders and healthcare providers play a crucial role in ensuring accurate coding despite incomplete or unclear documentation.
Working with unstructured data
In some instances, clinical coders may face unstructured or disorganized data, which can pose challenges during the coding process. Coders need to carefully review and extract relevant information from medical records to assign appropriate codes. The ability to identify key details within unstructured data requires strong analytical skills and attention to detail, enabling coders to ensure accurate and comprehensive coding.
Maintaining accuracy in fast-paced healthcare settings
Clinical coding often takes place in fast-paced healthcare settings, which adds another layer of complexity to the coder’s role. It is essential for coders to maintain accuracy and efficiency while working within time constraints. The pressure to code quickly can increase the risk of errors, underscoring the importance of coders’ ability to prioritize effectively and maintain focus on accurate coding practices.
Overcoming the pressure to code quickly
Clinical coders may face pressure to code quickly due to high patient volumes and time constraints. However, it is important to prioritize accuracy over speed to ensure the integrity and reliability of coded data. Organizations should encourage a supportive environment that emphasizes the significance of coding accuracy and provide resources, such as coding tools and workflow optimization, to help coders manage their workload efficiently without compromising accuracy.
Skills and Qualifications Required for Clinical Coding
In-depth knowledge of medical terminology and anatomy
Clinical coders must possess a strong foundation in medical terminology and anatomy to accurately assign codes. Understanding medical terms and their meanings enables coders to interpret documentation and identify the relevant codes that reflect the patient’s condition and treatment accurately. In-depth knowledge of anatomy helps coders understand the relationship between different body parts and systems, enabling comprehensive coding.
Proficiency in coding systems and guidelines
A key requirement for clinical coders is proficiency in coding systems such as ICD, CPT, and HCPCS, along with their respective guidelines. Coders need to be familiar with the code structures, coding conventions, and rules specific to each system to assign codes accurately. Staying updated with coding guidelines and best practices ensures consistent and compliant coding.
Analytical and critical thinking skills
Clinical coders must possess strong analytical and critical thinking skills to effectively analyze medical records and identify the appropriate codes. They must be able to interpret complex information, identify inconsistencies or ambiguities, and make informed coding decisions. Analytical skills also enable coders to identify potential coding errors or discrepancies and take corrective actions.
Attention to detail and accuracy
Attention to detail is crucial in clinical coding to ensure accurate coding and documentation of patient information. Coders must meticulously review medical records, identify relevant details, and assign codes accordingly. Even small errors can have significant consequences, emphasizing the importance of coders’ focus and precision in their work.
Ability to work well under pressure
Clinical coding often involves working in fast-paced healthcare settings, requiring clinical coders to perform under pressure. The ability to remain calm, focused, and efficient in demanding situations is essential. Coders must effectively manage their time, prioritize tasks, and maintain accuracy, even when faced with tight deadlines or high caseloads.
This image is property of www.rasmussen.edu.
Training and Education for Clinical Coders

Certification programs for clinical coding
Certification programs are available for individuals aspiring to become clinical coders. These programs offer comprehensive training and education in medical coding, including instruction in coding systems, guidelines, and documentation requirements. Certification provides formal recognition of an individual’s proficiency and can enhance employment opportunities in the field.
Degree programs in Health Information Management
Degree programs in Health Information Management (HIM) encompass a broader scope of healthcare information, including clinical coding. These programs provide a comprehensive understanding of healthcare systems, data management, coding, and regulatory compliance. A degree in HIM prepares individuals for various roles, including clinical coding, medical records management, and health informatics.
Continuing education and professional development opportunities
Continuing education and professional development are critical for clinical coders to stay updated with evolving coding practices and industry standards. Professionals can engage in workshops, seminars, webinars, and online courses to enhance their skills and knowledge. Professional organizations and associations also offer resources and networking opportunities for ongoing learning and staying current with industry trends.
Importance of practical coding experience
Practical coding experience is invaluable in developing coding skills and gaining confidence in the application of coding guidelines. Hands-on experience allows coders to encounter real-world coding scenarios, build familiarity with different medical specialties, and improve accuracy in coding decisions. Practical coding experience is often gained through internships, externships, or entry-level coding positions.
The role of mentors and supervisors in improving coding skills
Mentors and supervisors play a crucial role in the professional development of clinical coders. Mentors provide guidance, support, and knowledge-sharing opportunities, helping coders refine their skills and navigate coding challenges. Supervisors provide constructive feedback, assess performance, and identify areas for improvement, facilitating continuous growth and improvement in coding skills.
Benefits of Effective Clinical Coding

Accurate patient records and data analysis
Effective clinical coding ensures accurate and standardized documentation of patient information. Accurate coding allows for detailed and comprehensive patient records, enabling healthcare providers to make informed decisions for patient care. Additionally, coded data supports meaningful analysis and research efforts, facilitating population health management and identification of health trends.
Improved patient care and outcomes
Accurate clinical coding contributes to improved patient care and outcomes. Proper documentation and coding of diagnoses and treatments enable healthcare organizations to track patients’ conditions, monitor treatment effectiveness, and identify opportunities for intervention or improvement. Coded data also supports care coordination across healthcare settings, ensuring seamless transitions and continuity of care.
Streamlined healthcare operations and billing processes
Efficient clinical coding streamlines healthcare operations, particularly in billing and reimbursement processes. Accurate coding enables prompt and accurate billing, reducing delays and revenue loss for healthcare organizations. Streamlined billing processes also enhance patient satisfaction by minimizing billing errors and facilitating efficient claims processing.
Support for healthcare research and population health management
High-quality coded data is essential for healthcare research, population health management, and public health initiatives. Accurate and consistent coding enables comprehensive data analysis, facilitating research in areas such as disease prevalence, treatment effectiveness, and healthcare utilization. Coded data also supports population health management strategies by identifying health trends, targeting interventions, and monitoring health outcomes.
Effective communication between healthcare providers and payers
Accurate clinical coding ensures effective communication between healthcare providers and payers, such as insurance companies or government agencies. Clear and standardized documentation of diagnoses and procedures facilitates accurate reimbursement and reduces the likelihood of claim denials or delays. Accurate coding also helps providers demonstrate medical necessity and support appropriate utilization of healthcare resources.
Tools and Technology for Clinical Coders

Electronic Health Record (EHR) systems
Electronic Health Record (EHR) systems are commonly used in healthcare settings to store and manage patient information. EHR systems often include features that support clinical coding, such as integrated coding modules or tools that facilitate code selection and documentation. These systems streamline coding processes, enhance accuracy, and improve communication between coders and other healthcare professionals.
Coding software and applications
Specific coding software and applications are available to assist clinical coders in their work. These tools offer functionalities such as code lookup, screening for edits or errors, and integration with coding guidelines. Coding software and applications can enhance coding efficiency, accuracy, and compliance with coding standards.
Medical reference resources and coding books
Medical reference resources and coding books are essential references for clinical coders. These resources provide detailed information on coding guidelines, conventions, and coding principles. They also include code descriptions, sequencing instructions, and documentation requirements. Coders rely on these references to ensure accurate coding and compliance with coding standards.
Utilizing artificial intelligence and natural language processing
Artificial intelligence (AI) and natural language processing (NLP) are emerging technologies that have the potential to enhance clinical coding. AI algorithms can analyze large volumes of patient data, identify patterns, and assist in selecting appropriate codes. NLP technology can process unstructured data, such as free-text medical notes, and extract relevant information for coding purposes. These technologies have the potential to improve coding accuracy and efficiency.
The role of automation in clinical coding
Automation plays a growing role in clinical coding, particularly in tasks that can be standardized and repetitive. Automated coding tools can assist coders in code selection, suggest codes based on documentation, and identify potential errors or discrepancies. Automation can streamline coding processes, reduce the risk of human error, and enhance productivity. However, the expertise and judgment of clinical coders remain crucial in ensuring accurate and compliant coding.
Opportunities and Career Outlook in Clinical Coding

Growing demand for skilled clinical coders
The demand for skilled clinical coders is expected to grow as healthcare organizations strive to improve data accuracy, compliance, and reimbursement. The increasing adoption of electronic health records and data-driven healthcare further emphasizes the need for proficient clinical coders. Individuals with coding expertise and relevant certifications can expect favorable employment prospects and potential career advancement opportunities.
Career paths and job opportunities in coding
Clinical coding offers diverse career paths and job opportunities. Clinical coders can work in various healthcare settings, including hospitals, physician practices, ambulatory care centers, and insurance companies. They may also pursue specialized roles in specific medical specialties, such as coding for cardiology, orthopedics, or oncology. Additionally, clinical coders can explore opportunities in coding auditing, compliance, or management roles.
Remote coding opportunities
Advancements in technology have enabled remote coding opportunities for clinical coders. Remote coding allows coders to work from home or other locations, providing flexibility and work-life balance. Remote coding positions may be available through healthcare organizations, coding companies, or as independent contractors. However, remote coding requires self-discipline, effective communication, and adherence to coding guidelines and privacy regulations.
Potential for specialization in specific areas of coding
Clinical coders often have the opportunity to specialize in specific areas of coding based on their interest and expertise. Specialization can involve in-depth knowledge of coding guidelines, procedures, and diagnoses specific to a medical specialty. For example, coders can specialize in coding for pediatrics, obstetrics, or mental health. Specialization enhances career prospects and allows coders to develop niche expertise in their chosen field.
Continued learning and advancement in the field
Clinical coding provides opportunities for continued learning and professional growth. Coders can pursue advanced certifications, attend conferences or workshops, and engage in professional networking to stay updated with coding advancements. Advancement within the field can involve positions such as coding supervisors, coding educators, or coding consultants. Continued learning and skill development are key to staying competitive and thriving in the dynamic field of clinical coding.
Tips and Strategies for Learning Clinical Coding

This image is property of www.northwestcareercollege.edu.
Understanding the coding guidelines and conventions
To become proficient in clinical coding, it is essential to thoroughly understand the coding guidelines and conventions of the coding systems used. Familiarize yourself with the structure of the coding systems, the rules for code selection and sequencing, and any specific documentation requirements. Regularly refer to coding guidelines and conventions to ensure accurate coding practices.
Practicing coding scenarios and case studies
Practical application is a valuable method for learning clinical coding. Practice coding scenarios and case studies that encompass a variety of diagnoses, procedures, and treatments. This hands-on approach helps develop coding skills, enhances familiarity with different coding concepts, and reinforces understanding of coding guidelines and conventions.
Seeking guidance from experienced coders
Experienced coders can provide valuable guidance and insights into the intricacies of clinical coding. Seek mentorship opportunities or engage in discussions with experienced coders to learn from their expertise. Their experiences and practical knowledge can help you navigate coding challenges, clarify coding concepts, and provide valuable tips for accurate and efficient coding.
Utilizing coding textbooks and online resources
Utilize coding textbooks and online resources as references and study materials. Coding textbooks provide comprehensive coverage of coding guidelines, conventions, and principles. Online resources, websites, and forums dedicated to clinical coding also offer valuable information, coding tips, and discussion forums. These resources can supplement your learning and provide additional insights into clinical coding.
Participating in coding workshops and training programs
Participating in coding workshops and training programs provides structured learning opportunities and access to coding experts. These programs often offer hands-on training, coding exercises, and opportunities for interaction with instructors and fellow coders. Workshops and training programs can enhance your coding skills, expand your knowledge, and keep you updated with the latest coding practices.
Conclusion

Clinical coding requires dedicated effort and continuous learning
Clinical coding is a fundamental process in healthcare that translates medical information into standardized codes. It involves a comprehensive understanding of coding systems, guidelines, medical terminology, and anatomy. Clinical coders play a critical role in ensuring accurate and reliable patient documentation, supporting effective communication, data analysis, and decision-making.
While it may present challenges, it offers rewarding career opportunities
Clinical coding may be complex, requiring coders to navigate multiple coding systems, understand intricate guidelines, and overcome various challenges. However, it offers rewarding career opportunities in healthcare, with a growing demand for skilled coders. With in-depth knowledge, attention to detail, and ongoing training, clinical coders can excel in their careers and contribute to improved patient care and healthcare outcomes.
The importance of accurate and efficient clinical coding cannot be underestimated
Accurate and efficient clinical coding is essential for healthcare organizations, payers, researchers, and policymakers. It ensures accurate billing, supports data analysis and research efforts, and enables effective communication between healthcare providers and payers. The integrity and reliability of coded data are vital for informed decision-making, improved patient outcomes, and the overall delivery of quality healthcare services.