In this article, you will learn about the various types of CPT codes used in medical billing. CPT codes, or Current Procedural Terminology codes, are a standardized way to describe specific medical procedures and services. By understanding the different types of CPT codes, you will have a better understanding of the billing process and how medical services are classified.
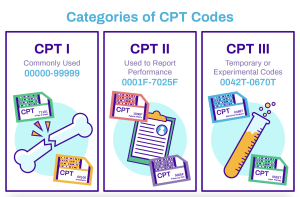
There are three main types of CPT codes in medical billing: Category I, Category II, and Category III. Category I codes are the most common and are used to report procedures and services such as office visits, surgeries, and diagnostic tests. These codes are regularly updated to incorporate new techniques and technology. Category II codes are optional and used to track performance measures. They are used to report additional information about a service or procedure, such as patient history, follow-up care, or patient outcomes. Category III codes are temporary codes used to report emerging technology, procedures, or services. These codes are used for data collection and research purposes, and are often replaced with Category I codes once they become more established.
Introduction
CPT codes, or Current Procedural Terminology codes, are a fundamental aspect of medical billing and coding. They are used to identify and communicate medical procedures and services performed by healthcare professionals. CPT codes play a crucial role in ensuring accurate reimbursement and efficient healthcare operations. In this article, we will explore the different types of CPT codes and their significance in medical billing.
Overview of CPT Codes
What are CPT codes?
CPT codes are a standardized set of codes developed and maintained by the American Medical Association (AMA). These codes consist of five digits and are used to describe medical procedures, services, and supplies provided by healthcare providers. CPT codes are recognized and utilized globally and are an essential tool in medical billing and coding.
Importance of CPT codes in medical billing
CPT codes provide a common language for healthcare professionals, insurance companies, and government agencies involved in medical billing. These codes serve as a means of transparent communication, ensuring that the services provided are accurately documented and billed. They also facilitate claims processing, reimbursement, and data analysis, making them vital for accurate financial management and healthcare decision-making.
Role of CPT codes in healthcare reimbursement
CPT codes play a critical role in healthcare reimbursement. Insurance companies and government payers utilize these codes to determine payment amounts for medical procedures and services. Each CPT code corresponds to a specific reimbursement rate, allowing for accurate and fair reimbursement based on the complexity and nature of the provided healthcare services. CPT codes also serve as a reference point for auditing and compliance purposes, ensuring that healthcare providers are appropriately reimbursed.
Category I CPT Codes
Definition of Category I CPT codes
Category I CPT codes represent the most common and widely accepted medical services and procedures. These codes cover a broad range of healthcare specialties and are regularly updated by the AMA. Category I codes are used to report procedures and services that have been proven to be effective and have widespread application in the medical field.
Examples of Category I CPT codes
Category I CPT codes encompass various medical procedures across different specialties. Examples of Category I codes include:
- 99213: Office or other outpatient visits for the evaluation and management of an established patient.
- 70553: Magnetic resonance imaging (MRI) of the brain without contrast material.
- 29788: Arthroscopic repair of a torn meniscus in the knee.
These examples highlight the diversity of medical procedures that fall under Category I CPT codes.
Purpose of Category I CPT codes
Category I CPT codes serve as the foundation for medical billing and coding. They ensure consistency and accuracy in reporting healthcare services, allowing for effective communication among healthcare providers, insurance companies, and government agencies. Category I codes also facilitate research, analysis, and billing processes, making them crucial for the healthcare industry.
Category II CPT Codes
Category II CPT codes consist of optional tracking codes that supplement the Category I codes. These codes are used to collect data for performance measurement and quality improvement purposes. They allow healthcare providers to report additional information relevant to patient care, such as patient demographics, risk factors, and outcomes.
Use of Category II CPT codes
Category II CPT codes are not required for reimbursement, but their utilization can enhance the quality of healthcare delivery. Healthcare providers may choose to report these codes to provide additional data that contributes to research and quality improvement efforts. Insurance companies and government agencies may also use this data to evaluate healthcare performance and outcomes.
Benefits of Category II CPT codes
Category II CPT codes offer several benefits to the healthcare industry. By collecting additional data, these codes support evidence-based medicine, quality improvement initiatives, and research. They enable healthcare providers to track outcomes and measure the effectiveness of specific interventions. Category II codes also promote transparency and accountability, as they encourage the reporting of important patient information beyond what is captured by Category I codes.
Category III CPT Codes
Category III CPT codes are temporary codes used to report emerging technologies, procedures, and services that are still under evaluation. These codes facilitate data collection, research, and tracking of new and innovative healthcare practices. Category III codes include services and procedures that may not yet have sufficient clinical evidence to qualify for Category I codes.
When to use Category III CPT codes
Healthcare providers use Category III CPT codes when performing new, experimental, or emerging procedures or services. These codes allow for tracking and monitoring the outcomes and effectiveness of these innovative practices. Category III codes are particularly useful in fields such as telemedicine, genomics, and emerging surgical techniques.
Advantages of Category III CPT codes
Category III CPT codes provide several advantages to the healthcare industry. They enable healthcare professionals to report and document new and emerging technologies, assisting in the evaluation and research of these practices. Category III codes also facilitate communication and understanding between providers, payers, and regulatory bodies regarding these experimental procedures. Using Category III codes promotes transparency, improves patient care, and contributes to future advancements in healthcare.
Evaluation and Management CPT Codes
Evaluation and Management (E/M) codes are a set of CPT codes specifically designed to report encounters between patients and healthcare providers for evaluation, diagnosis, and treatment management. These codes cover a wide range of medical services, including office visits, consultations, hospital visits, and emergency department encounters.
Different levels of E/M codes
E/M codes are categorized into different levels based on the complexity of the encounter and the amount of time spent with the patient. The levels include:
- Level 1: 99201-99205 – Office or other outpatient visits for new patients.
- Level 2: 99211-99215 – Office or other outpatient visits for established patients.
- Level 3: 99241-99245 – Consultations for new or established patients.
- Level 4: 99251-99255 – Hospital inpatient consultations.
- Level 5: 99281-99285 – Emergency department visits.
These levels allow for accurate reporting and reimbursement based on the complexity and intensity of the medical encounter.
Coding guidelines for E/M codes
Coding for E/M services requires careful consideration of documentation guidelines and medical decision-making. The level of history, examination, and medical complexity must be accurately documented to determine the appropriate E/M code. Adhering to coding guidelines and accurately reporting E/M services ensures proper reimbursement and compliance with regulations.
Surgical CPT Codes

Definition of surgical CPT codes
Surgical CPT codes are used to report procedures that involve cutting, altering, or manipulating body tissues. These codes cover a wide range of surgical interventions, from minor procedures to complex surgeries. Surgical CPT codes provide a standardized method of reporting surgical services across medical specialties.
Modifiers and surgical CPT codes
Modifiers are additional codes used to provide additional information regarding the surgical procedure. They can indicate various aspects of the surgery, such as multiple procedures performed during the same operative session, the use of physician assistants, or the modified approach used. Modifiers provide more specific details regarding the surgical procedure and help ensure accurate reimbursement.
Coding rules for surgical CPT codes
When coding surgical procedures, healthcare professionals must consider the specific details of the surgery, including the body part involved, the type of approach used, and any additional procedures performed during the same operative session. Accurate coding ensures proper reimbursement and avoids errors or discrepancies in claims processing.
Anesthesia CPT Codes
Overview of anesthesia CPT codes
Anesthesia CPT codes are used to report the administration of anesthesia during surgical or medical procedures. These codes identify the type and level of anesthesia provided and allow for accurate reimbursement to anesthesia providers. Anesthesia CPT codes are categorized based on the type, complexity, and duration of anesthesia administered.
Anesthesia modifiers and CPT codes
Anesthesia modifiers are additional codes used to provide specific information related to anesthesia services. These modifiers may indicate factors such as the patient’s physical status, the use of monitored anesthesia care, or the involvement of multiple anesthesia providers. Anesthesia modifiers ensure precise reporting and help determine appropriate reimbursement for anesthesia services.
Common challenges in coding anesthesia CPT codes
Coding for anesthesia services can be complex due to the varying levels and types of anesthesia provided. Accurate documentation is crucial to determine the appropriate anesthesia code. Additionally, coding for anesthesia in combination with other surgical or medical procedures requires careful consideration of coding rules and guidelines. Healthcare professionals must stay updated with coding changes and guidelines to ensure accurate coding and billing.
Radiology CPT Codes

Explanation of radiology CPT codes
Radiology CPT codes are used to report various imaging procedures and diagnostic tests performed to assess and diagnose medical conditions. These codes cover a wide range of radiology services, including X-rays, ultrasounds, CT scans, MRIs, and nuclear medicine procedures. Radiology CPT codes provide a standardized method of reporting and billing for these imaging services.
Different types of radiology procedures
Radiology procedures encompass a wide range of diagnostic imaging techniques. Some examples of radiology procedures include:
- 74177: CT scan of the abdomen and pelvis with contrast material.
- 76856: Transvaginal ultrasound.
- 71045: X-ray of the chest, two views.
These codes represent a small sample of the multitude of radiology procedures covered by CPT codes.
Documentation requirements for radiology CPT codes
Accurate documentation is essential for coding and billing radiology procedures. The documentation should include specific details regarding the procedure performed, the body part imaged, and any additional findings or complications. Proper documentation allows for accurate coding, reimbursement, and communication among healthcare providers.
Conclusion
In conclusion, CPT codes are an integral part of medical billing and coding. Understanding the different types of CPT codes, such as Category I, II, and III codes, Evaluation and Management codes, surgical codes, anesthesia codes, and radiology codes, is essential for accurate reporting, reimbursement, and communication within the healthcare industry. Adhering to coding guidelines, documenting procedures correctly, and staying up-to-date with coding changes are crucial for effective medical billing and coding practices.