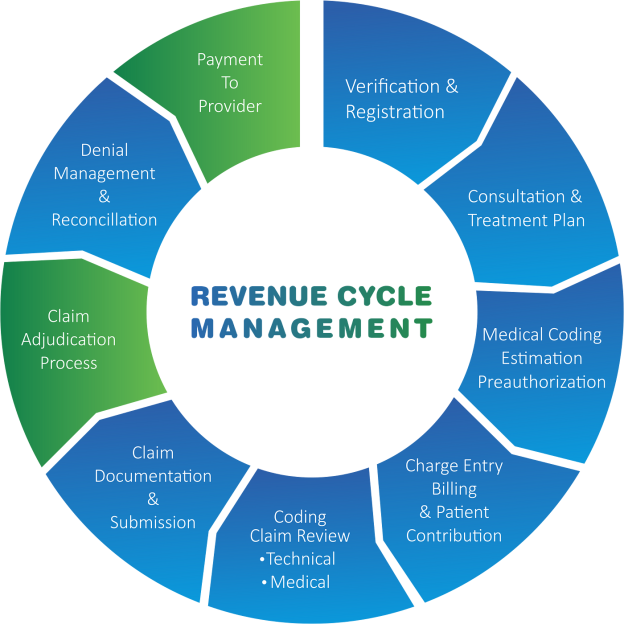
In the realm of medical billing, efficient revenue cycle management (RCM) is essential for the Financial success of healthcare providers. The process of RCM involves several intricately connected steps that ensure timely capture, submission, and reimbursement of medical claims. From patient registration and verification of insurance coverage to coding, billing, and collections, each stage plays a crucial role in maximizing revenue and minimizing errors. By understanding the intricate steps involved in RCM, healthcare organizations can streamline their billing processes, enhance cash flow, and ultimately provide better patient care.
Overview of RCM Medical Billing
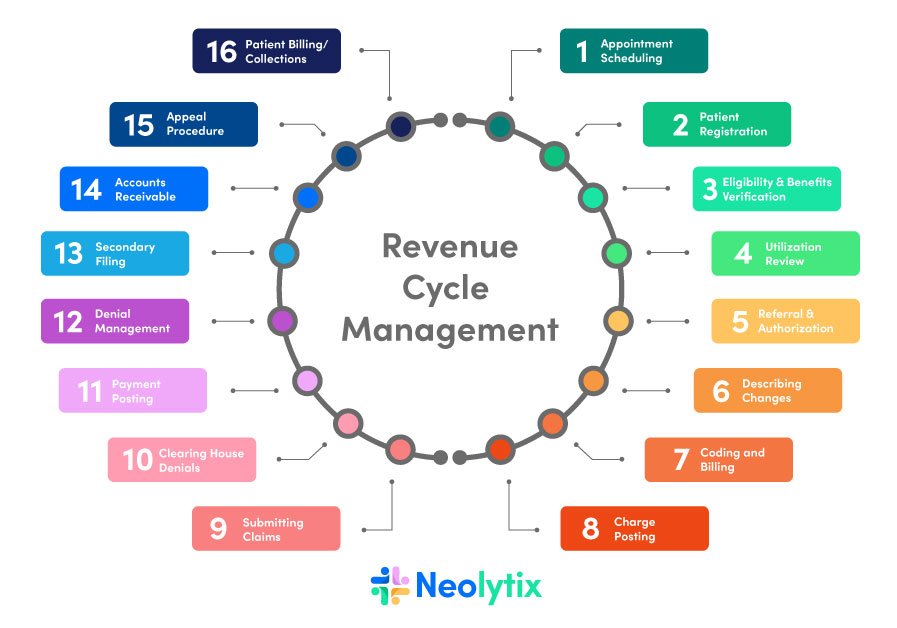
This image is property of neolytix.com.
What is RCM Medical Billing?
RCM Medical Billing, or Revenue Cycle Management Medical Billing, is a comprehensive process that healthcare organizations use to streamline the financial aspect of their services. It involves managing the entire patient billing and reimbursement cycle, from patient registration to claims submission, payment posting, and accounts receivable follow-up. RCM Medical Billing ensures that healthcare providers receive accurate and timely payments for the services they provide.
Importance of RCM Medical Billing
The importance of RCM Medical Billing cannot be understated in the healthcare industry. It plays a crucial role in ensuring the financial stability and success of healthcare organizations. By effectively managing the revenue cycle, healthcare providers can optimize their revenue, minimize claim denials, improve cash flow, and enhance overall operational efficiency. RCM Medical Billing also ensures compliance with coding standards, billing regulations, and insurance requirements, leading to reduced billing errors and improved reimbursement rates.
Basic Steps in RCM Medical Billing
RCM Medical Billing consists of several basic steps that are essential for the successful management of the revenue cycle. These steps include patient registration, insurance verification, coding and documentation, charge entry, claims submission, payment posting, accounts receivable follow-up, denial management, appeals process, and reporting and analysis. Each step plays a critical role in the overall process and requires meticulous attention to detail and adherence to industry regulations and standards.
Understanding RCM Medical Billing Process
Patient Registration
Patient registration is the initial step in RCM Medical Billing. It involves collecting comprehensive patient information, such as demographic details, insurance information, and contact details. Accurate patient registration ensures that the subsequent steps in the billing process are conducted smoothly and without errors. This information is used to create a unique patient account and assign a patient identifier, which is vital for tracking the patient’s billing and healthcare records.
Insurance Verification
The insurance verification step is crucial to determine the patient’s insurance coverage and eligibility for the services they require. It involves confirming the patient’s insurance coverage, verifying their eligibility and benefits, and obtaining pre-authorization for any services that require prior approval. Insurance verification helps healthcare providers avoid claim denials and ensures that services rendered are covered by the patient’s insurance policy and plan.
Coding and Documentation
Coding and documentation are essential in RCM Medical Billing to ensure accurate billing and reimbursement. Healthcare providers must assign appropriate diagnosis codes (ICD) and procedure codes (CPT/HCPCS) to reflect the services provided accurately. Compliance with medical coding standards is imperative to avoid claim denials and regulatory penalties. Adequate medical record documentation is also crucial for supporting the codes assigned, ensuring accurate billing, and preventing potential audit findings.
Charge Entry
Charge entry involves accurately recording the charges for the services provided by healthcare providers. This step ensures that the fees and charges are correctly entered into the billing system and linked to the corresponding procedure codes assigned during the coding and documentation process. Proper charge entry is crucial for accurate claims submission and ensures that healthcare providers are reimbursed appropriately for the services rendered.
Claims Submission
The claims submission step involves preparing and submitting claims to insurance companies or government payers for reimbursement. This step can be done electronically or via mail, depending on the payer’s requirements. It is essential to complete and submit the necessary documents accurately and promptly to avoid claim denials or delays in reimbursement. Tracking the status of submitted claims is crucial to identify any rejections or issues that need to be addressed promptly.
Payment Posting
Payment posting involves receiving and processing payments from insurance companies or patients. This step requires meticulous attention to detail to ensure accurate payment application to the patient’s account. Healthcare providers must identify any underpayments or overpayments and take appropriate action to reconcile discrepancies. Accurate payment posting is vital for maintaining accurate financial records and improving cash flow.
Accounts Receivable Follow-Up
The accounts receivable follow-up step involves monitoring and managing outstanding claims and payments. It includes investigating claim denials, rejections, or unpaid balances and taking necessary actions to resolve any issues. Healthcare providers must follow up with insurance companies, patients, or third-party payers to ensure timely collection of outstanding payments. Efficient accounts receivable follow-up is essential to minimize revenue leakage and improve overall financial performance.
Denial Management
Denial management is a critical component of RCM Medical Billing that focuses on identifying and resolving claim denials. It involves analyzing denied claims, determining the reasons for denial, and taking necessary actions to appeal or resubmit the claims. Effective denial management helps healthcare providers recover lost revenue and minimize the impact of denied claims on their financial performance. It also provides valuable insights into potential areas for improvement in coding, documentation, or claims submission processes.
Appeals Process
The appeals process is an important step in RCM Medical Billing to challenge claim denials and seek a favorable resolution. It involves gathering all relevant documentation and evidence to support the appeal, drafting a comprehensive appeal letter, and following the payer’s guidelines and deadlines for submission. An effective appeals process increases the chances of overturning claim denials and maximizing reimbursement for healthcare services provided.
Reporting and Analysis
Reporting and analysis are critical components of RCM Medical Billing that help healthcare providers evaluate their financial performance and identify areas for improvement. Generating financial and performance reports allows healthcare organizations to monitor key metrics, such as average reimbursement rates, claim denial rates, and accounts receivable turnover. Analyzing these metrics helps identify trends, identify potential areas for improvement, and implement strategies to optimize RCM and enhance overall financial outcomes.
In conclusion, RCM Medical Billing is a comprehensive process that encompasses a series of steps aimed at streamlining the financial aspect of healthcare services. From patient registration to claims submission, payment posting, and accounts receivable follow-up, each step plays a vital role in ensuring accurate and timely reimbursement for healthcare providers. By understanding and effectively implementing RCM Medical Billing, healthcare organizations can optimize their revenue, minimize claim denials, and improve overall financial performance.