In this article, we will explore various strategies and tools that can help streamline your medical billing process. By implementing these techniques, you will be able to save time and resources, reduce errors, and improve efficiency in your medical practice. From utilizing electronic billing software to staying up-to-date with coding changes, you’ll learn practical tips to simplify your medical billing tasks and enhance overall practice management. Join us as we dive into the world of medical billing and discover ways to make it easier for you.
Overview of Medical Billing
Medical billing is a crucial aspect of healthcare administration that involves the process of submitting and following up on claims with health insurance companies in order to receive payment for services provided. It plays a vital role in the revenue cycle management of healthcare practices, as accurate and efficient medical billing ensures timely reimbursement.
In this article, we will discuss various strategies and practices that can help simplify the medical billing process, making it easier for healthcare providers to manage their billing operations.
Understanding the Basics of Medical Billing
Before diving into the ways to make medical billing easier, it is essential to have a basic understanding of how the process works. Medical billing involves several critical steps, including:
- Patient Check-in: The first step in the medical billing process is capturing accurate patient information during the check-in process. This includes demographic details, insurance coverage, and contact information.
- Coding: Once the patient’s visit is completed, medical coders assign specific codes to the services rendered during the visit. These codes reflect the diagnosis and the procedures performed, ensuring accurate billing.
- Claim Submission: After the coding process, healthcare providers submit claims to the insurance companies for reimbursement. This involves preparing and sending the necessary documentation, such as a claim form and supporting medical records.
- Claim Processing: The insurance company reviews the submitted claims to determine the validity and accuracy of the information provided. They then process the claim and make a payment to the healthcare provider accordingly.
- Denials and Appeals: In cases where claims are denied, healthcare providers need to identify the reasons for denial and submit an appeal with additional documentation or clarification to support the claim.
- Reimbursement: Once the claim is approved, the insurance company reimburses the healthcare provider for their services.
Now that we have a basic understanding of the medical billing process, let’s explore some strategies to make it easier and more efficient.

Organizing Medical Billing Documents
Proper organization of medical billing documents is essential to ensure smooth and efficient billing operations. Here are some steps you can take to create a proper system for document organization:
Creating a Proper System for Document Organization
Investing in a robust document management system can significantly streamline your medical billing process. This system should have the capability to store and retrieve electronic documents quickly and efficiently. It should also include features such as document indexing, search functionality, and security measures to protect patient information.
By maintaining a centralized repository for all billing-related documents, you can eliminate the hassle of searching for paper documents and reduce the chances of misplacing important paperwork. This organized approach saves time and improves productivity, allowing you to focus on other critical aspects of your healthcare practice.
Utilizing Electronic Health Record (EHR) Systems
Electronic Health Record (EHR) systems also play a vital role in simplifying medical billing processes. These systems not only provide a comprehensive view of a patient’s medical history but also offer built-in billing functionalities.
By using an EHR system that integrates billing capabilities, you can streamline the entire billing process. These systems automate coding, claim submission, and even denial management, reducing human error and improving efficiency.
Additionally, EHR systems can help you stay updated with changes in insurance policies, fee schedules, and regulatory requirements automatically. This eliminates the need for manual updates and ensures that your billing practices remain compliant with the latest industry standards.
Streamlining Medical Coding
Accurate medical coding is crucial for proper billing and reimbursement. The following strategies can help streamline your medical coding process and make it easier to manage:
Importance of Proper Medical Coding
Proper medical coding ensures that the services provided to patients are accurately documented and billed. It is essential to assign the correct codes for diagnoses, procedures, and treatments to avoid claim denials and delays in reimbursement.
To ensure accuracy in medical coding, it is crucial to provide adequate training to your coding staff. Certified coding professionals with up-to-date knowledge of coding guidelines can make a significant difference in the accuracy of your billing process.
Using Coding Software to Expedite the Process
Coding software can be a game-changer when it comes to simplifying and expediting the medical coding process. These software solutions automate the coding process by suggesting codes based on entered information, minimizing errors and improving efficiency.
Investing in coding software that integrates seamlessly with your practice management system or EHR can significantly streamline the coding process. These software solutions often come with features such as code lookup, compliance checking, and real-time updates to ensure accurate coding.
With the assistance of coding software, your coding team can work more efficiently and focus on handling complex coding scenarios, rather than spending excessive time on routine coding tasks.
Improving Accuracy in Billing
Accurate billing is critical to ensure timely payment and avoid claim denials. Here are some essential practices that can help improve accuracy in your medical billing process:
Double-checking Patient Information
Before submitting a claim, it is crucial to double-check patient information to ensure accuracy. This includes verifying demographic details, insurance coverage, and any changes in contact information.
By implementing a standardized process for checking patient information at every visit, you can minimize errors and reduce the chances of claim rejections due to incorrect or outdated information.
Regularly Updating Fee Schedules and Insurance Policies
Insurance policies and fee schedules are subject to changes over time. To avoid billing errors, it is essential to stay updated with the latest changes in insurance policies and fee schedules.
Frequent updates to your practice management system or billing software can help you stay on top of these changes. Regularly reviewing and updating your fee schedules ensures accurate billing, reduces claim denials, and improves reimbursement rates.
By implementing these practices, you can minimize billing errors, improve accuracy, and ensure seamless reimbursement for your healthcare services.
Automating Insurance Claim Submission
Automating the insurance claim submission process can significantly simplify medical billing operations and expedite reimbursement. Here are two effective ways to automate the claim submission process:
Implementing Electronic Claims Submission
Electronic claims submission involves submitting claims electronically to insurance companies instead of using paper forms. This method eliminates the need for manual paperwork, reduces errors, and accelerates the claims process.
To implement electronic claims submission, you must ensure that your practice management system or billing software is capable of generating electronic claims. This typically involves using standardized electronic formats such as the HIPAA-compliant 837 Professional or Institutional claims.
By electronically submitting claims, you can speed up the reimbursement process, reduce administrative costs, and improve overall efficiency in your medical billing operations.
Utilizing Clearinghouses for Efficient Claim Processing
Clearinghouses act as intermediaries between healthcare providers and insurance companies for claim processing. These organizations receive claims, validate them for errors, and perform checks for compliance before forwarding them to the appropriate insurance companies.
Utilizing a clearinghouse for claim processing can streamline your billing operations by ensuring that claims are submitted accurately and with the necessary supporting documentation. Clearinghouses often provide services such as claim scrubbing, which helps identify and rectify potential errors before submission.
By leveraging the expertise and capabilities of clearinghouses, you can enhance the efficiency of your claim processing, reduce denials, and improve the success rate of your reimbursement.

Managing Denials and Appeals
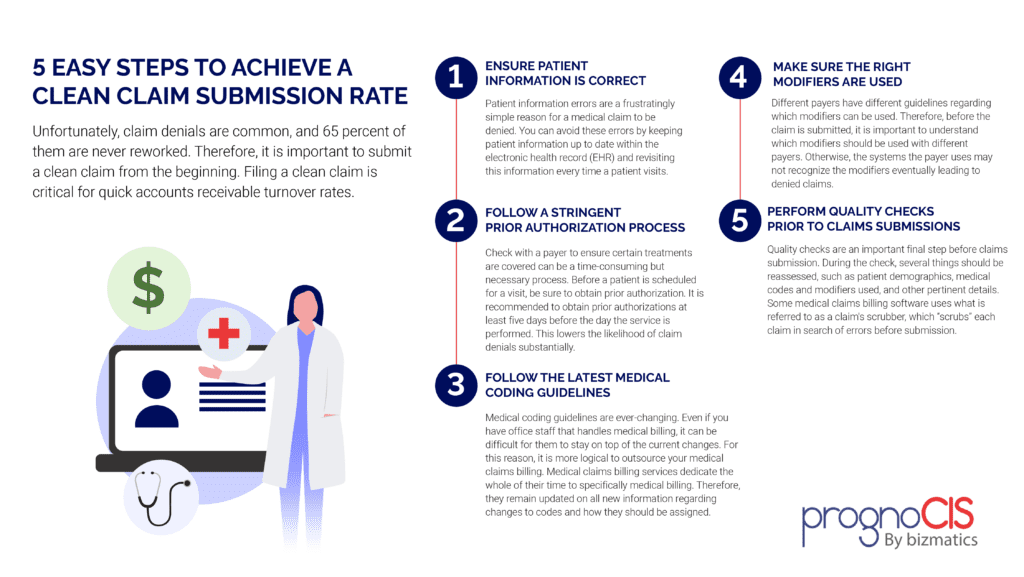
Despite taking all necessary precautions, claim denials are inevitable in the medical billing process. Effective denial management and appeals processes are crucial to ensure maximum reimbursement. Here are some strategies to manage denials and improve your appeal success rate:
Understanding Common Denial Reasons
To effectively manage denials, it is essential to understand the common reasons behind claim denials. These reasons can vary from incorrect coding and missing documentation to eligibility issues and timely filing limitations.
By analyzing claim denial patterns, you can identify recurring issues and take proactive measures to address them. This may include additional training for coding staff, improved documentation practices, or enhanced claim scrubbing processes.
Developing Effective Appeal Strategies
When a claim is denied, promptly initiate the appeals process. This involves gathering all supporting documentation, providing additional information, and submitting a formal appeal to the insurance company.
To improve your appeal success rate, ensure that your appeals include well-documented medical necessity, clear explanations of previously submitted information, and any additional evidence required to support the claim.
By developing effective appeal strategies, you can increase the likelihood of reimbursement for denied claims, ensuring optimal revenue management for your healthcare practice.
Ensuring Proper Reimbursement
To ensure proper reimbursement for your medical services, focus on implementing the following strategies:
Implementing Medical Billing Audits
Regular medical billing audits can help identify any billing errors or compliance issues that may impact your reimbursement. These audits involve a comprehensive review of your billing processes, coding accuracy, documentation practices, and adherence to compliance guidelines.
By conducting routine audits, you can detect and rectify any errors or deficiencies in your billing practices, ensuring accurate reimbursement and minimizing the risk of audits or penalties.
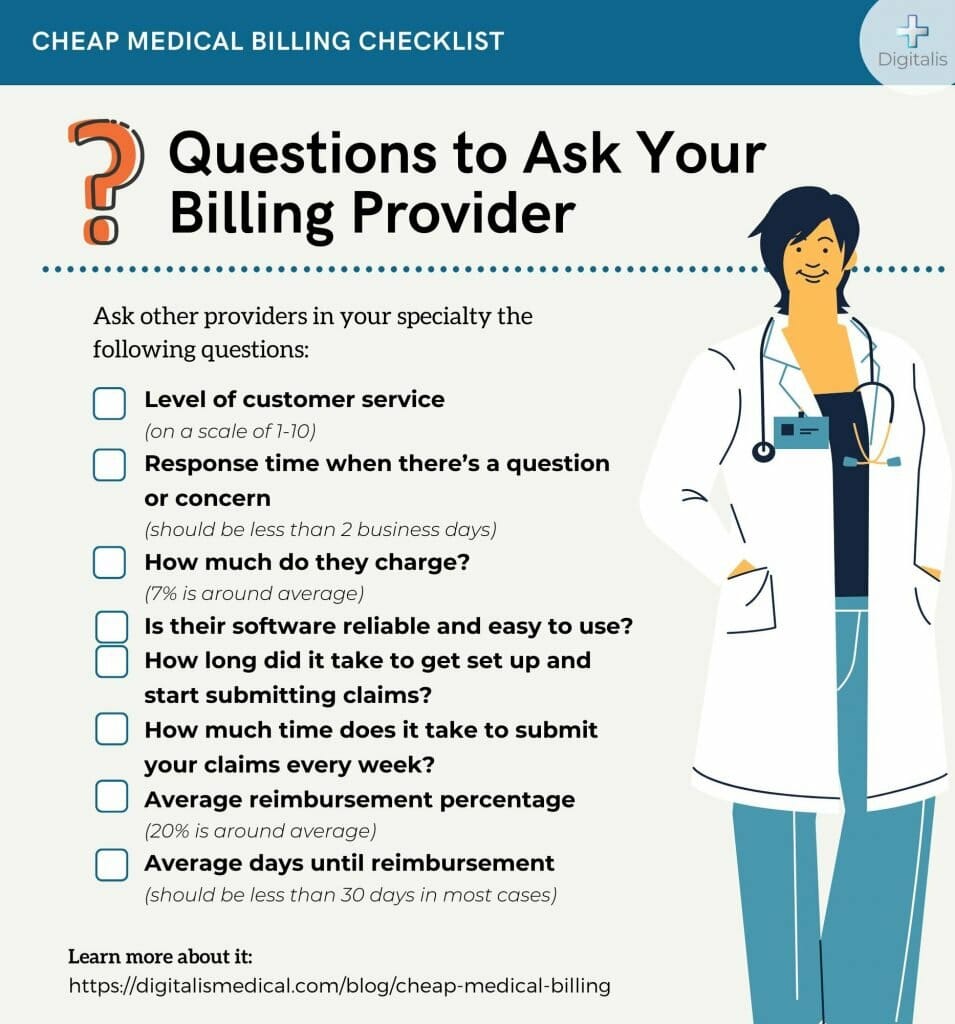
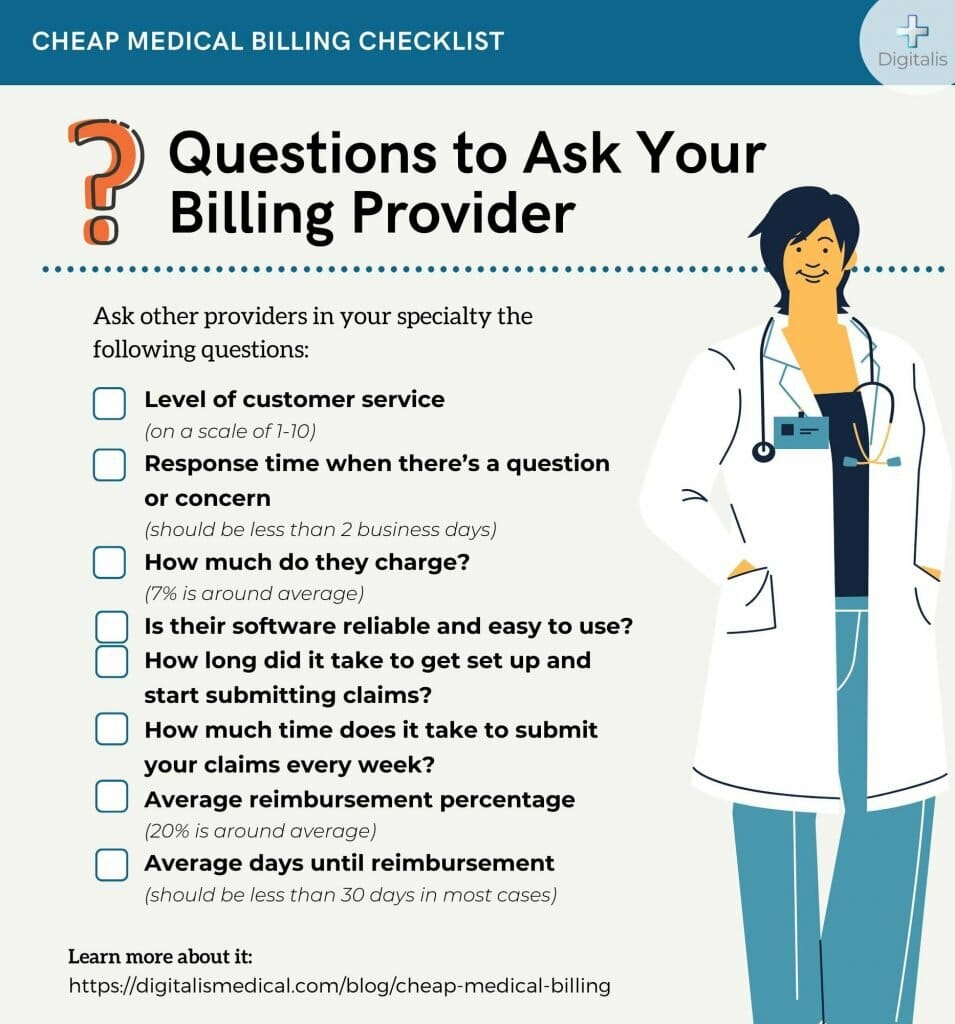
Negotiating Contracts with Insurance Companies
Negotiating favorable contracts with insurance companies can significantly impact your reimbursement rates. Take the time to review existing contracts and analyze reimbursement rates compared to the industry standard.
Consider engaging in contract negotiations to secure better reimbursement rates and favorable terms. This may involve presenting data on your practice’s patient volume, quality outcomes, and the value of services provided.
By negotiating contracts that reflect the true value of your services, you can ensure optimal reimbursement and improve the financial health of your healthcare practice.
Staying Updated with Industry Changes
The field of medical billing is constantly evolving, with changes in regulations, coding guidelines, and reimbursement policies. Staying updated with these changes is essential to ensure compliance and maximize revenue. Here are some strategies to stay informed:
Continuing Education for Medical Billing Professionals
Encourage your billing staff to engage in ongoing professional development and continuing education programs. These programs help them stay abreast of the latest industry changes, including regulatory updates and coding guideline revisions.
Investing in the professional growth of your billing team ensures that they are equipped with the knowledge and skills necessary to navigate complex billing scenarios and adapt to evolving requirements.
Networking with Peers and Industry Associations
Networking with peers and participating in industry associations can provide valuable insights into industry trends and best practices. In addition, these networks offer opportunities for learning from experienced professionals and sharing knowledge and experiences.
Attending industry conferences and workshops, participating in online forums, and joining professional associations can help you stay connected with the broader medical billing community and stay updated with the latest industry news.
Understanding Compliance and Regulatory Requirements
Compliance with healthcare regulations, particularly the Health Insurance Portability and Accountability Act (HIPAA), is essential for protecting patient privacy and avoiding costly penalties. In addition, staying up-to-date with the International Classification of Diseases, 10th Revision (ICD-10) coding guidelines is crucial. Here are some key considerations for compliance:
Complying with HIPAA Regulations
Ensure that your medical billing practices are fully compliant with HIPAA regulations. This includes safeguarding patient information, accessing and transmitting data securely, and adhering to the requirements for electronic transactions.
Regular training and education on HIPAA regulations for your billing staff can help prevent breaches and maintain compliance with the law. Additionally, conducting periodic audits and risk assessments can help identify any potential vulnerabilities and address them proactively.
Staying Up-to-date with ICD-10 Coding Guidelines
ICD-10 coding guidelines determine the codes used to describe diagnoses and procedures for medical billing purposes. Staying updated with these guidelines is crucial for accurate coding and compliant billing practices.
Regularly review and update your coding manuals and resources to reflect the latest revisions in ICD-10 guidelines. Provide your coding staff with ongoing training to ensure their proficiency in accurate coding and adherence to the latest coding guidelines.
By prioritizing compliance and staying up-to-date with regulatory requirements, you can minimize the risk of penalties, maintain patient trust, and ensure the financial stability of your healthcare practice.
Conclusion
In conclusion, simplifying medical billing is essential for healthcare providers to save time, reduce errors, and improve revenue management. By implementing efficient systems, staying updated with industry changes, and prioritizing accuracy in billing practices, healthcare professionals can make their medical billing process easier and more effective.
Investing in proper document organization, utilizing electronic health record (EHR) systems, streamlining medical coding, improving accuracy in billing, automating insurance claim submission, managing denials and appeals, ensuring proper reimbursement, staying updated with industry changes, understanding compliance and regulatory requirements, and continuing education are all critical steps in making medical billing easier.
By adopting these practices, healthcare providers can optimize their billing operations, enhance financial performance, and focus on delivering high-quality patient care.