Is it difficult to acquire the knowledge of medical coding? This query often arises among those interested in pursuing a career in this field. Well, understanding medical coding can indeed be a challenging endeavor. The intricacies and vastness of medical terminology, along with the ever-evolving industry guidelines and regulations, may seem overwhelming at first. However, with dedication, patience, and a comprehensive study approach, you can certainly learn the ins and outs of medical coding.
Mastering medical coding requires a strong foundation in anatomy, physiology, and medical terminology. Familiarity with the various coding systems, such as ICD-10 and CPT, is crucial as well. Additionally, staying updated with the ever-changing healthcare landscape, including coding updates and industry standards, is essential. While the learning curve may prove steep, with the right resources, guidance, and commitment to continuous learning, you can develop the skills and knowledge necessary to succeed in medical coding. Remember, perseverance and a passion for accuracy are vital attributes in this profession. Learning medical coding can be challenging, but it is certainly not an impossible task. The difficulty of learning medical coding can vary from person to person, depending on several factors. Factors that can influence the difficulty of learning medical coding include your educational background and experience, the complexity of medical terminology, the amount of time and effort you devote to learning, and your individual learning style and preferences.
One of the key factors that can influence the difficulty of learning medical coding is your educational background and experience. If you have a background in healthcare or a related field, you may already have a basic understanding of medical terminology and concepts, which can make learning medical coding easier. On the other hand, if you have limited or no experience in the healthcare field, you may need to spend more time familiarizing yourself with medical terminology and concepts before diving into coding.
The complexity of medical terminology is another factor that can impact the difficulty of learning medical coding. Medical terminology is highly specialized and can be quite complex, with numerous terms, abbreviations, and acronyms to learn. It takes time and effort to become familiar with these terms and understand their meanings in the context of coding. However, with consistent practice and exposure to medical terminology, you can gradually build your knowledge and become proficient in coding.
The amount of time and effort you devote to learning medical coding also plays a significant role in determining the level of difficulty. Medical coding requires a substantial investment of time and effort, as it involves learning different coding systems, understanding coding guidelines, and staying updated with industry changes. The more time and effort you dedicate to studying and practicing medical coding, the faster you will grasp the concepts and develop your coding skills.
Individual learning styles and preferences can also influence the difficulty of learning medical coding. Some individuals may learn best through hands-on practice, while others may prefer more structured educational programs. Finding methods and resources that align with your learning style can enhance the learning experience and make it easier for you to understand and apply medical coding concepts.
Despite the challenges, there are several benefits to learning medical coding that make the effort worthwhile. One of the significant benefits is the promising job outlook in the field. With the increasing demand for healthcare services and the need for accurate medical coding, professionals in this field are in high demand. By learning medical coding, you can secure a stable and rewarding career with ample job opportunities.
Furthermore, medical coding offers great potential for growth and advancement. As you gain experience and expertise in coding, you can explore opportunities for career advancement, such as becoming a coding supervisor or a coding auditor. Continuous learning and professional development can open doors to higher-level positions and enhance your earning potential.
Another benefit of learning medical coding is the work flexibility it offers. Medical coders have the option to work in various healthcare settings, including hospitals, clinics, insurance companies, and consulting firms. Additionally, many coding professionals have the flexibility to work remotely, allowing for a better work-life balance.
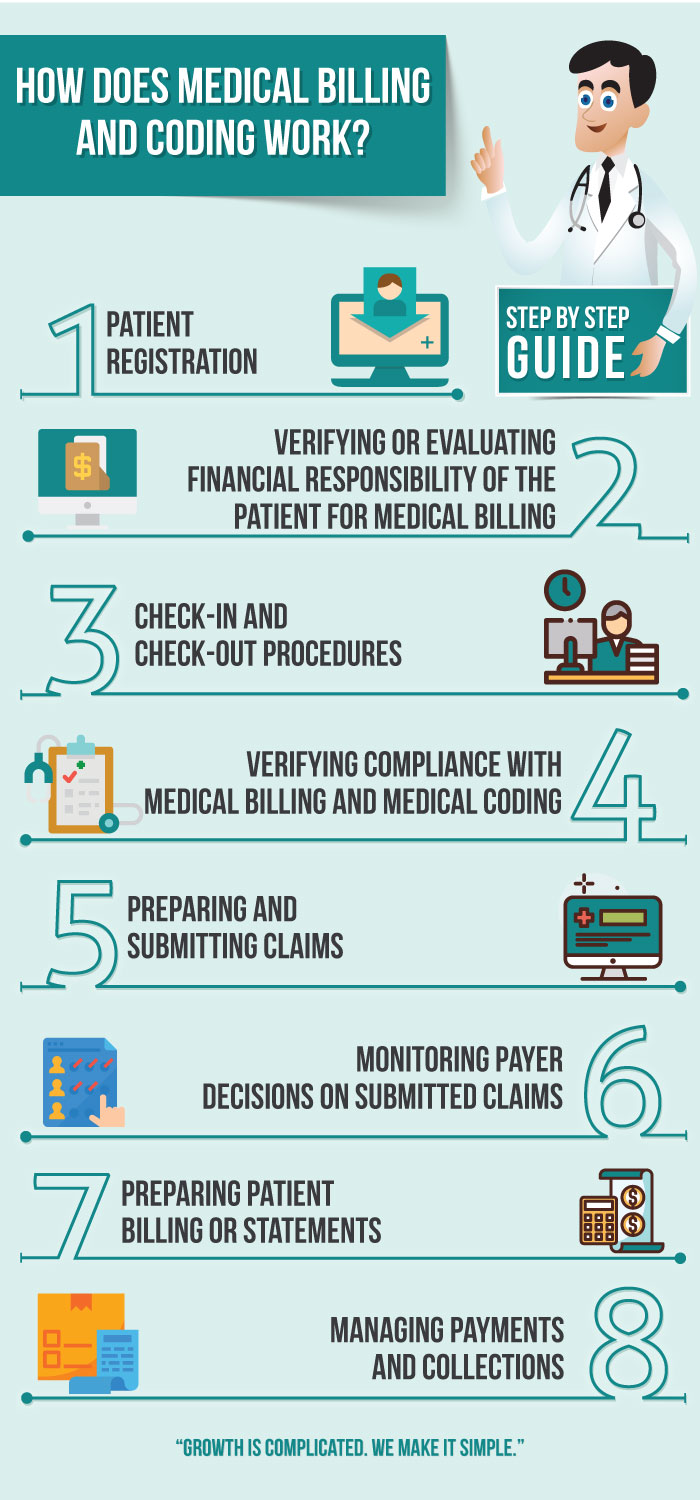
Learning medical coding also allows you to contribute to the healthcare industry in a meaningful way. Medical coding plays a crucial role in ensuring accurate billing, reimbursement, and records management. By mastering medical coding, you become an essential part of the healthcare system, supporting the delivery of quality patient care.
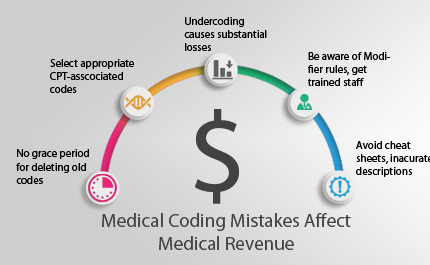
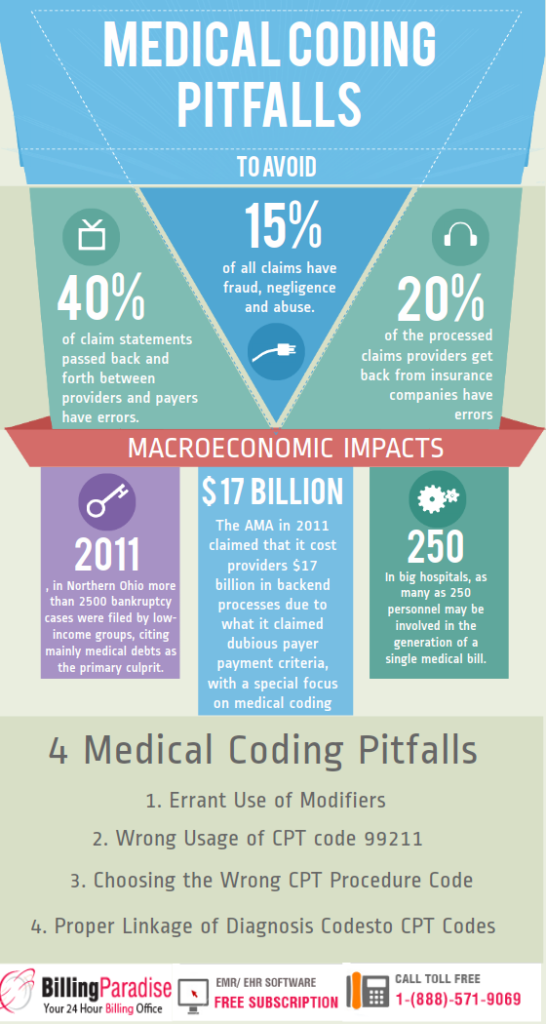
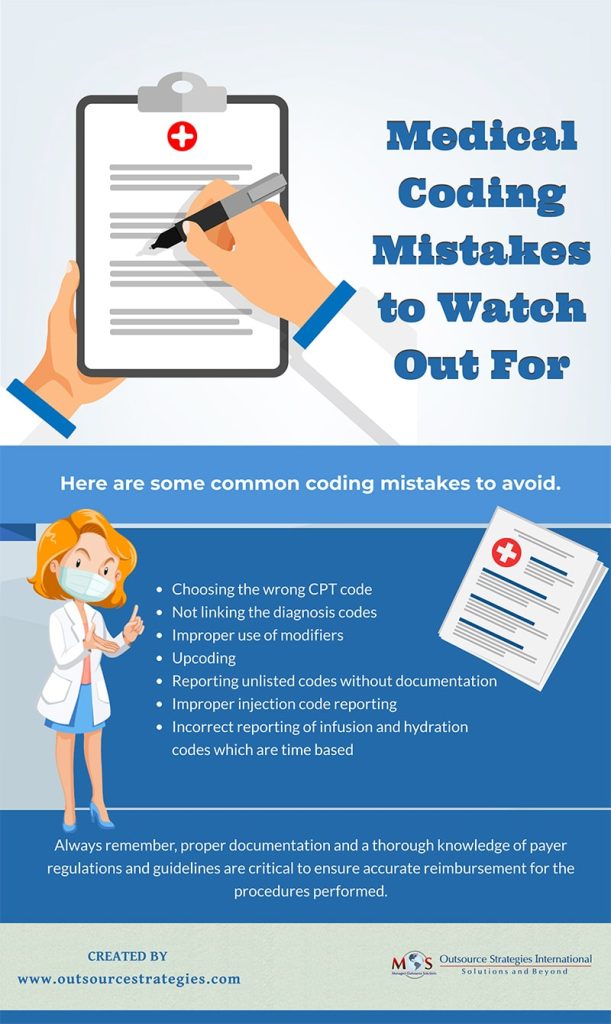
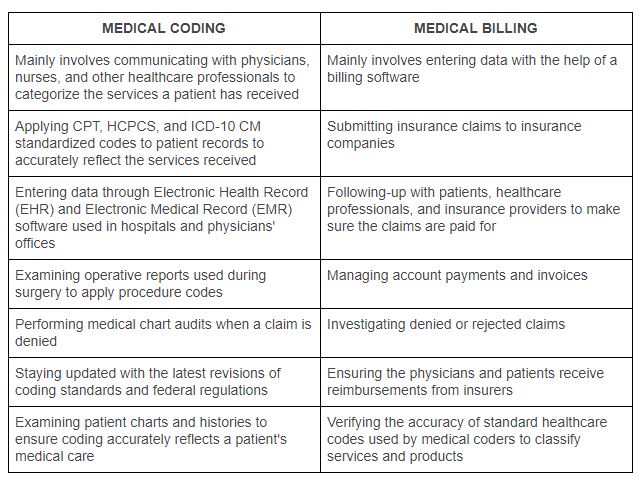
While there are benefits to learning medical coding, it is essential to acknowledge the challenges that come with it. One of the main challenges is the vast amount of information that needs to be absorbed. Medical coding involves learning different coding systems, such as ICD-10, CPT, and HCPCS, each with its own set of rules and guidelines. Additionally, medical coding guidelines are constantly evolving, requiring coding professionals to stay updated with the changes.
Accuracy and attention to detail are also crucial in medical coding. Even a small error or oversight in coding can have significant implications for patient care, reimbursement, and compliance. Medical coders must have a keen eye for detail and the ability to analyze complex medical records and documentation accurately.
Furthermore, medical coding entails understanding and navigating different coding systems. Each coding system has its own structure, conventions, and terminology, which can be overwhelming for beginners. It takes time and practice to develop fluency in using these coding systems effectively.
Fortunately, there are various learning resources available to support your journey in learning medical coding. Formal education programs, such as community college courses or vocational schools, can provide a comprehensive foundation in medical coding. These programs often cover subjects like anatomy, medical terminology, and coding principles.
Online courses and training modules are also valuable resources for learning medical coding. These self-paced courses allow you to study at your convenience and offer interactive exercises and assessments to test your understanding.
Professional associations, such as the American Academy of Professional Coders (AAPC) or the American Health Information Management Association (AHIMA), provide certifications and educational resources to support your learning and professional development. These associations also offer networking opportunities, allowing you to connect with experienced coding professionals and seek mentorship.
Mentorship and networking opportunities are invaluable for learning medical coding. Connecting with experienced coding professionals can provide guidance, insights, and practical tips for mastering the coding process. Additionally, networking can help you stay updated with industry trends and job opportunities.
To ensure successful learning, it is important to establish a solid foundation in anatomy and medical terminology. Understanding these foundational concepts is essential for accurate coding. Taking the time to study and review anatomy and medical terminology will enable you to better comprehend medical records and accurately assign codes.
Utilizing effective study techniques can also enhance your learning experience. Breaking down complex information into manageable parts, creating flashcards, and using mnemonic devices can help you retain and recall coding concepts.
Practicing hands-on coding exercises is crucial for developing coding skills. Analyzing real medical records and assigning accurate codes will strengthen your coding abilities and help you become more confident in your coding accuracy.
Seeking guidance from experienced coding professionals can greatly benefit your learning journey. They can provide feedback on your coding work, answer your questions, and offer insights and tips for improvement.
Continuous learning and professional development are vital in the medical coding field. The healthcare industry is constantly evolving, with new coding guidelines, regulations, and technologies emerging. Staying updated with industry changes through continuous learning ensures that your coding skills remain relevant and accurate.
Engaging in continuing education programs, attending coding conferences, and subscribing to industry publications can help you stay current with the latest coding trends and developments. These activities provide opportunities to expand your knowledge, learn new coding techniques, and network with other coding professionals.
Networking and collaboration with other coding professionals are also essential for professional growth. Engaging with coding communities, participating in coding forums, and joining professional associations allow you to connect with peers, share knowledge and experiences, and learn from each other.
Seeking advanced certifications is another way to demonstrate your expertise and commitment to continuous learning. Advanced certifications, such as Certified Coding Specialist (CCS) or Certified Professional Coder (CPC), validate your coding skills and can lead to greater career opportunities and higher earning potential.
Having a supportive work environment and collaborative teams can greatly contribute to your success in learning medical coding. Access to experienced mentors and colleagues who can provide guidance and support is invaluable. Regular feedback and performance reviews can help you identify areas for improvement and guide your professional development.
Opportunities for peer learning, such as coding team meetings or coding roundtables, can allow you to learn from the experiences of others and gain insights into different coding methodologies and approaches.
Overcoming self-doubt and maintaining persistence are crucial in the journey of learning medical coding. Building confidence through practice and repetition is key. The more coding exercises you complete and the more familiar you become with coding principles, the more confident you will become in your coding abilities.
Setting realistic goals and celebrating milestones along the way can keep you motivated. Learning medical coding is a gradual process, and acknowledging your progress can boost your confidence and drive to continue learning.
Seeking support from peers and mentors can also help you overcome challenges and self-doubt. Sharing your concerns, asking for assistance, and learning from the experiences of others can provide valuable insights and encouragement.
In conclusion, learning medical coding can be challenging, but with the right resources, strategies, and support, it is an attainable goal. The factors that influence the difficulty of learning medical coding include your educational background and experience, the complexity of medical terminology, the amount of time and effort you dedicate to learning, and your individual learning style and preferences.
While there are challenges in learning medical coding, there are also numerous benefits, such as a promising job outlook, potential for growth and advancement, work flexibility, and the opportunity to contribute to the healthcare industry. By utilizing available learning resources, implementing effective learning strategies, and continuously investing in your professional development, you can overcome the challenges and thrive in your medical coding career. Remember to stay persistent, seek support when needed, and celebrate your achievements along the way.