As an aspiring professional in the medical field, it is crucial to understand the intricacies of billing and coding. The comprehensive program “What Do You Learn In Billing And Coding?” offers a comprehensive curriculum designed to equip individuals with the knowledge and skills required for success in this rapidly growing industry. From mastering medical terminology and understanding insurance claims to efficiently managing patient data and ensuring compliance with regulations, this program covers all essential aspects of billing and coding. Embark on a transformative journey of learning, where you will gain the expertise necessary to excel in the world of medical billing and coding.
Medical Billing and Coding Basics

Introduction to Medical Billing and Coding
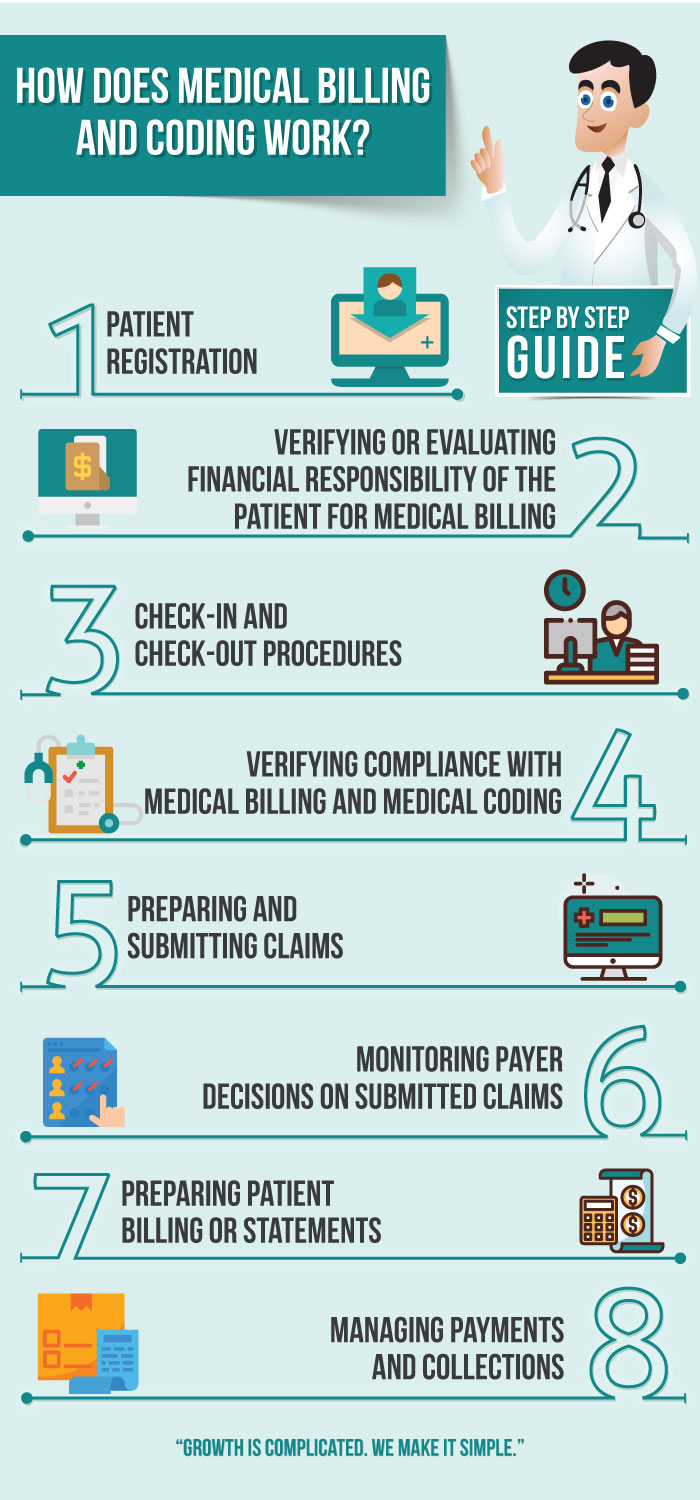
Medical billing and coding is a vital part of the healthcare industry, ensuring accurate reimbursement for healthcare services provided to patients. It involves translating medical procedures, diagnoses, and treatments into universally recognized alphanumeric codes. These codes are used by insurance companies, healthcare providers, and government agencies for reimbursement, statistical analysis, and research purposes. As a medical biller and coder, you will play a crucial role in the healthcare system by accurately coding and submitting claims, ensuring correct payment for healthcare services rendered.
Importance of Medical Billing and Coding
Accurate and efficient medical billing and coding are essential for multiple reasons. Firstly, it helps healthcare providers receive appropriate reimbursement for the services they provide, ensuring financial stability and the ability to continue delivering quality care. Additionally, medical billing and coding facilitate transparency and accountability by providing a standardized system for tracking and reporting healthcare services.
Medical billing and coding also aid in maintaining accurate medical records, which are crucial for patient care, research, and legal purposes. These records ensure that medical information is easily accessible and properly managed, leading to better patient outcomes and informed decision-making by healthcare professionals. Overall, the accurate and thorough documentation of medical procedures and diagnoses through billing and coding contributes to the efficiency and effectiveness of the healthcare system as a whole.
Role of a Medical Biller and Coder
As a medical biller and coder, your primary responsibility is to convert healthcare services into standardized codes for billing and reimbursement purposes. This involves reviewing medical records, assigning the appropriate codes, and ensuring compliance with coding guidelines and regulations. Additionally, you will handle insurance claims, verify patient information, and communicate with insurance companies and healthcare providers to resolve any billing discrepancies or issues.
Medical billers and coders also play a crucial role in ensuring accurate and timely payments by monitoring claim statuses, identifying and addressing claim denials, and initiating appeal processes when necessary. Your attention to detail, knowledge of coding systems, and understanding of medical terminology and procedures will be instrumental in efficiently managing the billing and coding processes.
Medical Terminology and Anatomy

Introduction to Medical Terminology
Medical terminology is the language used in the healthcare field to describe medical conditions, procedures, and anatomical structures. As a medical biller and coder, it is crucial to have a solid understanding of medical terminology to accurately interpret and assign the appropriate codes. By familiarizing yourself with medical prefixes, suffixes, and root words, you will be able to decipher complex medical terms and effectively navigate the coding process.
Anatomy and Physiology
A basic understanding of anatomy and physiology is essential for medical billers and coders. It allows you to comprehend the relationship between different body systems, understand the purpose and function of various medical procedures, and accurately assign codes based on the specific area of the body being treated. Knowledge of anatomy and physiology also helps in identifying potential errors or inconsistencies in medical documentation, ensuring the accuracy and integrity of the coding process.
Common Medical Terms and Abbreviations
In addition to medical terminology and anatomy, medical billers and coders must be familiar with common medical terms and abbreviations used in healthcare documentation. Understanding these terms is crucial for accurately assigning the correct codes and ensuring effective communication with healthcare professionals. By familiarizing yourself with commonly used medical abbreviations, you will be able to accurately interpret medical records and efficiently navigate the coding process.
ICD and CPT Coding
Overview of ICD Coding
ICD (International Classification of Diseases) coding is a standardized system used worldwide to classify and code diagnoses, symptoms, and medical conditions. It provides a comprehensive list of codes that healthcare providers use to document and report patients’ diagnoses. Familiarity with ICD coding is essential for medical billers and coders, as it enables accurate representation of patients’ medical conditions for billing and reimbursement purposes. Proper application of ICD codes ensures that healthcare services are appropriately reimbursed and facilitates accurate data analysis for research and planning.
Introduction to CPT Coding
CPT (Current Procedural Terminology) coding is a system developed by the American Medical Association (AMA) to standardize the reporting of medical procedures and services. It involves assigning specific codes to each service or procedure performed by healthcare providers. CPT codes provide detailed descriptions of medical procedures and services, allowing for accurate billing and reimbursement. As a medical biller and coder, it is crucial to understand CPT coding guidelines and accurately assign the appropriate codes to ensure proper reimbursement and compliance with insurance regulations.
Modifiers and Evaluation and Management (E&M) Coding
Modifiers are additional codes used to provide additional information or clarification to the primary CPT or ICD codes. They are used to indicate specific circumstances, such as multiple procedures performed during the same session or a service performed with unusual circumstances. Medical billers and coders need to understand the proper use of modifiers to accurately represent the services provided and ensure accurate billing and reimbursement.
Evaluation and Management (E&M) coding is a specific subset of CPT coding that focuses on the documentation and coding of patient encounters, including office visits, hospital visits, and consultations. E&M coding requires medical billers and coders to carefully review medical documentation and assign the appropriate code based on the complexity and intensity of the patient encounter. Accurate E&M coding is crucial for determining reimbursement levels and ensuring compliance with insurance regulations.
Health Insurance and Reimbursement

Understanding Health Insurance
A fundamental aspect of medical billing and coding is understanding health insurance and the various types of coverage available. Different insurance plans have specific rules, guidelines, and reimbursement rates, which medical billers and coders must be familiar with to accurately process insurance claims. Understanding the basics of health insurance terminology, such as deductibles, copayments, and out-of-pocket limits, enables you to effectively communicate with patients and insurance companies, ensuring accurate billing and reimbursement.
Claims Processing
Medical billers and coders are responsible for processing insurance claims, which involves preparing and submitting documentation to insurance companies for reimbursement. This requires a thorough understanding of the specific requirements and guidelines set forth by each insurance company. It is essential to accurately complete claim forms, attach necessary documentation, and adhere to filing deadlines to ensure timely and accurate reimbursement. Effective claims processing involves attention to detail, knowledge of insurance regulations, and the ability to communicate effectively with insurance companies to resolve any issues or claim denials.
Medical Billing and Reimbursement
Medical billing and reimbursement involve the process of accurately billing patients or insurance companies for healthcare services rendered and receiving payment for those services. This process encompasses verifying patient insurance coverage, determining deductibles and copayments, accurately coding and documenting services rendered, submitting claims, and following up on outstanding payments. Medical billers and coders must have a solid understanding of medical coding, billing guidelines, and insurance regulations to navigate the complex reimbursement process successfully.
Medical Coding Ethics and Compliance

Importance of Ethical Medical Coding
Ethical medical coding is crucial to maintain the integrity and credibility of the healthcare system. Medical billers and coders must prioritize accuracy and honesty in coding practices to ensure proper reimbursement, prevent fraud and abuse, and uphold professional standards. Ethical coding involves accurately reflecting the services provided, avoiding unbundling or upcoding (assigning codes that do not accurately represent the services performed), and maintaining patient confidentiality and privacy. By adhering to ethical coding practices, medical billers and coders contribute to patient safety, maintain trust within the healthcare system, and promote ethical standards within the profession.
HIPAA Regulations and Compliance
The Health Insurance Portability and Accountability Act (HIPAA) sets forth regulations and guidelines to protect the privacy and security of patients’ health information. Medical billers and coders must strictly adhere to HIPAA regulations when handling and transmitting patient data, both in paper and electronic forms. This includes maintaining the confidentiality of patient records, using secure communication channels, and implementing appropriate safeguards to protect patient information. Understanding HIPAA regulations and ensuring compliance is essential for medical billers and coders to maintain patient trust and avoid potential legal and financial consequences.
Coding Audits and Compliance Programs
Coding audits and compliance programs are essential components of the medical billing and coding process. Audits serve to evaluate the accuracy and compliance of coding practices, ensuring that medical services are correctly documented and coded. Compliance programs involve implementing policies and procedures to ensure adherence to coding guidelines, regulations, and ethical standards. Conducting regular audits and participating in compliance programs help identify any coding errors or inconsistencies, maintain accurate coding practices, and mitigate the risk of fraudulent activities. Medical billers and coders should actively participate in audit and compliance activities to promote accountability, accuracy, and integrity within the coding process.
Electronic Health Records (EHR)

Introduction to EHR Systems
Electronic Health Records (EHR) systems have transformed the way healthcare information is stored and accessed. EHRs provide a digital platform for managing patient records, including medical history, laboratory results, allergies, and medications. As a medical biller and coder, you will likely work with EHR systems to access relevant patient information, retrieve medical records for coding purposes, and submit claims electronically. Understanding EHR systems and being proficient in their use is crucial for efficient and accurate medical billing and coding processes.
Benefits and Challenges of EHR
EHR systems offer numerous benefits to medical billers and coders. They enhance accessibility and facilitate quick retrieval of patient information, reducing the time spent searching for and gathering medical records. EHRs also support seamless communication between healthcare providers and insurance companies, promoting efficient claims processing and reimbursement. Furthermore, EHRs facilitate coordination between different healthcare facilities, ensuring continuity of care and accurate documentation of patient encounters.
However, EHR systems also present challenges that medical billers and coders must navigate. These challenges include technical issues, such as system crashes or slow response times, and the need for ongoing training to stay updated on system upgrades and new features. Additionally, the increased reliance on electronic records necessitates a heightened focus on data security and privacy, as any breaches can have serious consequences for both patients and healthcare providers.
Documentation in EHR
Accurate documentation in EHRs is crucial for medical billers and coders. Thorough and detailed records ensure that healthcare services are appropriately coded, billed, and reimbursed. Medical billers and coders should review and verify the accuracy of information entered into EHRs, including diagnoses, procedures, and any additional relevant details. Effective communication with healthcare professionals is essential to resolve any discrepancies or missing information, ensuring that coding and billing processes are accurate and compliant.
Medical Billing Software and Tools

Overview of Medical Billing Software
Medical billing software is a technological solution designed to streamline and automate the billing and coding process. These software applications offer features such as automated coding, claims management, and reimbursement tracking. Medical billers and coders can leverage these tools to improve efficiency, accuracy, and productivity in their daily tasks. Familiarity with various medical billing software systems is crucial, as each may offer different functionalities and interfaces.
Using Electronic Billing Software
Electronic billing software enables medical billers and coders to efficiently manage the billing process by automating key tasks. This software allows for the electronic submission of claims, reducing administrative burdens and minimizing the risk of errors. By utilizing electronic billing software, medical billers and coders can track claim statuses, receive electronic remittance advice, and generate reports for analysis and reconciliation. It is essential for medical billers and coders to be proficient in using electronic billing software to maximize efficiency and accuracy in their daily workflow.
Automation and Productivity Tools for Medical Billers and Coders
Automation and productivity tools play a significant role in enhancing the efficiency and productivity of medical billers and coders. These tools can include automated code suggestion features in coding software, electronic claim scrubbing tools that identify errors or missing information, and electronic remittance advice (ERA) processing tools that automate the payment reconciliation process. Leveraging these tools allows medical billers and coders to streamline tedious manual tasks, reduce errors, and allocate more time to critical thinking and problem-solving. Staying updated with the latest automation and productivity tools can greatly benefit medical billers and coders in optimizing their workflow and improving overall performance.
Claim Denials and Appeals

Reasons for Claim Denials
Claim denials occur when an insurance company determines that a claim cannot be reimbursed based on coverage restrictions, coding errors, or insufficient documentation. Common reasons for claim denials include incorrect coding, lack of medical necessity, duplicate billing, and timely filing issues. Denials can cause delays in reimbursement and impact the cash flow of healthcare providers. It is important for medical billers and coders to understand the common reasons for claim denials and take proactive measures to prevent them by accurately coding and thoroughly documenting services rendered.
Appealing Denied Claims
When a claim is denied, medical billers and coders play a critical role in the appeals process. This involves conducting a thorough review of the denial reason, gathering additional supporting documentation if necessary, and effectively communicating with insurance companies to resolve the denial. The appeals process requires strong communication skills, attention to detail, and perseverance. By advocating for the healthcare provider and providing sufficient evidence to support the claim, medical billers and coders can increase the likelihood of a successful appeal and ensure appropriate reimbursement.
Utilization Review and Appeals Process
Utilization review is a process conducted by insurance companies to assess the medical necessity, appropriateness, and efficiency of healthcare services. Medical billers and coders may be involved in the utilization review process by providing additional documentation, justification, or clarification to support the medical necessity of certain procedures or treatments. Understanding the utilization review process can help medical billers and coders proactively address potential issues, ensure accurate reimbursement, and minimize claim denials. Additionally, being familiar with the appeals process allows medical billers and coders to navigate claim denials effectively and maximize reimbursement for healthcare services rendered.
Career Opportunities in Billing and Coding

Job Roles and Responsibilities
A career in medical billing and coding offers various job roles and responsibilities within the healthcare industry. Medical billers and coders can be employed in hospitals, clinics, physician offices, specialty practices, insurance companies, and government agencies. In these roles, medical billers and coders are responsible for accurately coding medical procedures, ensuring compliance with coding guidelines and regulations, processing insurance claims, and communicating with healthcare providers and insurance companies. They play a vital role in the financial stability of healthcare organizations by facilitating proper reimbursement and efficient claims processing.
Salary and Job Outlook
The salary of a medical biller and coder can vary based on factors such as location, level of experience, and job responsibilities. According to the United States Bureau of Labor Statistics (BLS), the median annual wage for medical records and health information technicians, which includes medical billers and coders, was $44,090 in May 2020. The job outlook for this profession is favorable, with a projected growth rate of 8% from 2019 to 2029, faster than the average for all occupations. The increasing demand for healthcare services and the transition to electronic health records contribute to the positive job outlook for medical billers and coders.
Professional Development and Certifications
Continued professional development is essential for medical billers and coders to stay updated with advancements in medical coding, billing regulations, and industry best practices. Many professional associations and organizations offer specialized certifications, such as the Certified Professional Coder (CPC) or Certified Coding Specialist (CCS), which validate an individual’s knowledge and expertise in medical coding and billing. These certifications provide opportunities for career advancement, higher earning potential, and increased professional credibility. Pursuing continuing education courses, attending industry conferences, and staying informed about industry updates are also important for professional growth and maintaining competence in the evolving field of medical billing and coding.
Continuing Education in Billing and Coding

Importance of Continuing Education
Continuing education is crucial for medical billers and coders to remain current with changes in healthcare regulations, coding guidelines, and industry standards. Healthcare practices, coding systems, and reimbursement rules are constantly evolving, necessitating ongoing education to ensure accurate and compliant coding practices. Continuing education not only enhances professional competence but also demonstrates a commitment to lifelong learning and professional growth. By actively participating in continuing education programs, medical billers and coders can stay ahead of industry changes, adapt to emerging trends, and maintain the highest standards of coding accuracy and compliance.
Industry Updates and Changes
The healthcare industry experiences frequent updates and changes, including new coding guidelines, policy revisions, and regulatory updates. Medical billers and coders must stay informed about these changes to ensure accurate coding and compliant billing. Professional associations, industry publications, and online resources provide valuable information on the latest updates and changes in the field. Regularly reviewing updates and monitoring industry changes allows medical billers and coders to promptly adapt their practices, maintain compliance, and effectively contribute to the financial stability and success of healthcare organizations.
Continuing Education Options
Medical billers and coders have various options for continuing education, including attending seminars, workshops, and conferences offered by professional associations and organizations. These events provide opportunities to learn from industry experts, expand knowledge in specific coding areas, and network with colleagues. Online courses and webinars are also available, offering flexibility and convenience for those seeking to enhance their skills remotely. Additionally, professional certifications often require a certain number of continuing education credits to maintain certification status, providing structured and focused educational opportunities. Medical billers and coders can choose from a wide range of continuing education options to suit their learning preferences and professional goals.