In this article, we will explore the optimal number of claims that a biller should process on a daily basis. We will discuss the factors that can impact this number, such as the complexity of the claims, the efficiency of the billing system, and the skill level of the biller. By the end of this article, you will have a better understanding of how to determine the appropriate workload for a biller and ensure their productivity and effectiveness in the billing process.
Factors Affecting Claim Processing

Claim Complexity
The complexity of a claim is one of the key factors that can impact the number of claims a biller should process per day. Complex claims generally require more time and effort to process compared to simpler claims. Examples of complex claims include those involving multiple insurance policies, multiple providers, or complicated billing codes. When a biller has to deal with complex claims, the number of claims they can process per day may be significantly lower.
Staff Efficiency
The efficiency of the billing staff also plays a crucial role in determining how many claims a biller can process per day. Highly skilled and experienced billers are likely to be more efficient in processing claims compared to those who are less experienced or less familiar with the coding and reimbursement guidelines. Training and continuous education programs can help improve the efficiency of the billing staff and enable them to process more claims per day.
System Automation
The level of automation in the claim processing system can greatly affect the number of claims a biller can handle in a day. An automated system can streamline the process by reducing manual data entry and automating claim submission, thereby increasing the speed and efficiency of claim processing. A biller working with a highly automated system can handle a larger volume of claims compared to someone using a manual or less advanced system.
Claim Volume
The volume of claims received also has a direct impact on the number of claims a biller can process per day. When the claim volume is high, billers may need to prioritize and focus on processing a larger number of claims. On the other hand, when the claim volume is low, billers may have more time and resources to devote to each individual claim, potentially enabling them to process more complex or time-consuming claims.
Recommended Number of Claims per Day

Industry Standards
Industry standards can serve as a useful benchmark for determining the recommended number of claims a biller should process per day. Different specialties and healthcare organizations may have varying expectations for productivity and claim processing turnaround times. For example, in some specialties, a biller may be expected to process 30-40 claims per day, while in others, the expectation may be higher or lower.
Biller Experience
The experience and skill level of the biller can also influence the recommended number of claims they should process per day. More experienced billers who are familiar with the specific coding requirements for their specialty and have a deep understanding of the claim submission process may be able to handle a larger volume of claims compared to less experienced billers. It is important to consider the biller’s expertise and comfort level with different claim types when determining their workload.
Resource Availability
The availability of resources, such as staff and technology, can impact the number of claims a biller can handle in a day. A biller working with limited resources may have to work at maximum capacity to process a certain number of claims, while a biller with more resources at their disposal may be able to handle a higher volume. It is important to consider the availability of resources when determining the optimal number of claims a biller should process per day.
Impact of Excessive Claims Processing
Increased Errors
Processing a large number of claims in a day can increase the risk of errors. When billers are under pressure to meet high productivity targets, they may be more likely to make mistakes, such as coding errors or missing required documentation. These errors can lead to claim denials or delays in reimbursement, impacting the financial health of the healthcare organization.
Reduced Accuracy
When billers are overwhelmed with a high volume of claims, they may not have enough time to thoroughly review each claim for accuracy. This can result in inaccuracies in the claims submitted, leading to claim denials or underpayment. Maintaining a reasonable workload can help ensure that billers have the time and attention to detail required to accurately process claims.
Biller Burnout
Excessive claims processing can also contribute to biller burnout. Processing a large number of claims can be mentally and physically exhausting, especially when combined with other job responsibilities and tight deadlines. Burnout can lead to decreased productivity, increased errors, and a higher risk of turnover among billing staff. It is important to balance workload and provide support to billers to prevent burnout and maintain staff morale.
Strategies for Efficient Claim Processing

Prioritizing High-Value Claims
One strategy for efficient claim processing is to prioritize high-value claims, such as those with a higher reimbursement rate or those from top-paying insurance providers. By focusing on these claims first, billers can maximize revenue generation and ensure timely reimbursement for the healthcare organization. This approach allows billers to allocate their time and resources effectively, optimizing the number of claims processed per day.
Utilizing Technology Solutions
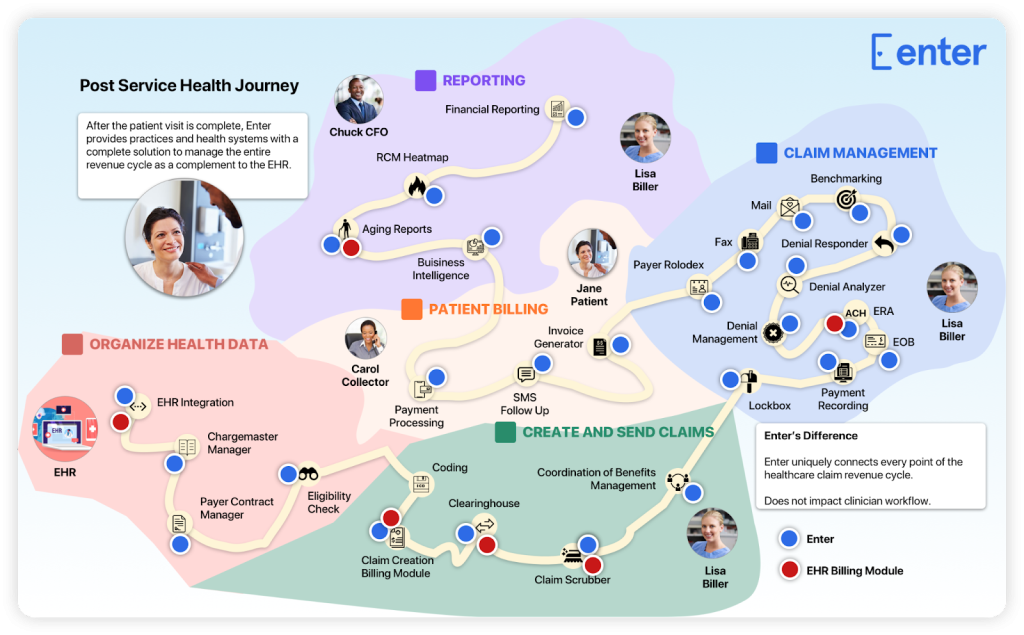
Technology solutions can significantly improve the efficiency of claim processing. Electronic health record (EHR) systems with integrated billing modules can automate many aspects of claim submission, reducing the time spent on manual data entry and paperwork. Claims scrubbing software can also help identify potential errors or inconsistencies in claims before submission, minimizing the risk of denials and rework. By utilizing technology solutions, billers can process a larger volume of claims per day with greater accuracy and speed.
Streamlining Workflows
Analyzing and streamlining workflows can help identify bottlenecks and inefficiencies in the claim processing process. By optimizing the workflow and eliminating unnecessary steps or redundancies, billers can save time and increase productivity. This can include streamlining the documentation collection process, standardizing coding practices, and implementing quality control measures. Streamlined workflows enable billers to process more claims per day while maintaining high accuracy rates.
Continuous Training
Providing ongoing training and education to billers is essential for keeping them up-to-date with the latest coding guidelines, regulations, and industry trends. Continuous training helps billers improve their knowledge and skills, enabling them to process claims more efficiently and accurately. Training programs can focus on areas where billers may need additional support, such as complex claim scenarios or changes in reimbursement policies. By investing in continuous training, healthcare organizations can ensure that their billing staff is equipped to handle a higher volume of claims with confidence.
Measuring Claim Processing Performance

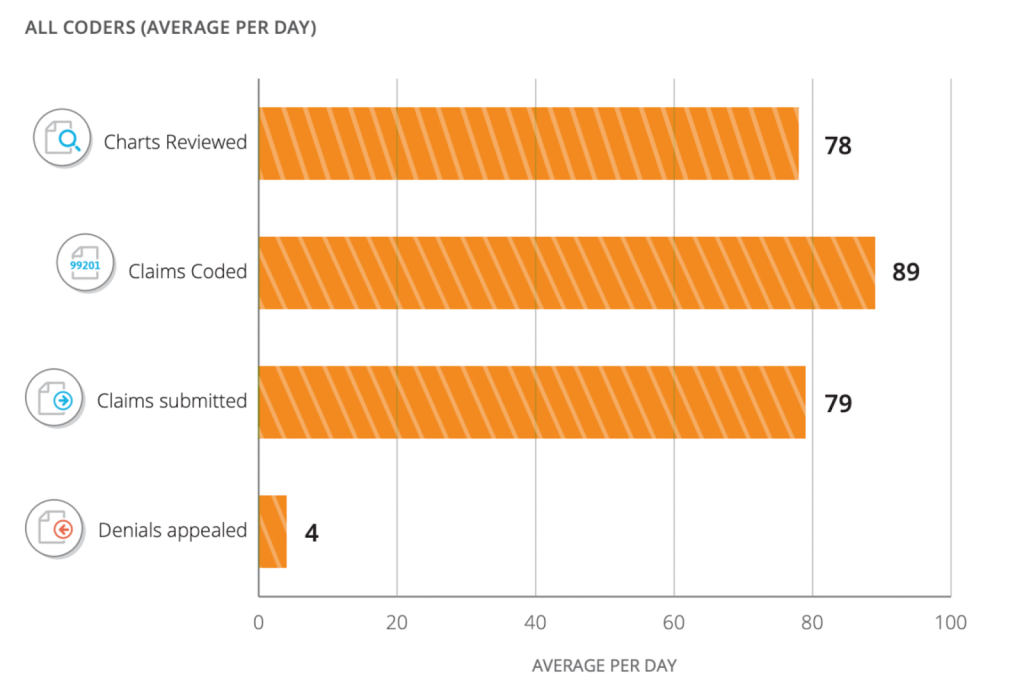
Claims Processed per Hour
One measure of claim processing performance is the number of claims processed per hour. This metric provides an indication of the biller’s productivity and efficiency in handling claims. Tracking claims processed per hour can help identify trends and variations in performance, allowing for targeted improvements and resource allocation.
Accuracy Rates
Another important measure of claim processing performance is the accuracy rate. This metric reflects the percentage of claims that are processed correctly the first time, without errors or rework. High accuracy rates indicate a biller’s ability to follow coding guidelines and submit clean claims, minimizing the risk of denials and payment delays.
Error Resolution Time
Error resolution time measures the time taken to identify and correct errors in claims. The quicker errors are identified and resolved, the faster claims can be resubmitted for reimbursement. Monitoring and reducing error resolution time can help optimize claim processing efficiency and minimize the impact of errors on revenue cycle management.
Potential Challenges in Claim Processing
Claim processing is the lifeblood of the healthcare revenue cycle, but it’s not without its challenges. In an ever-evolving healthcare landscape, professionals involved in claim processing must be prepared to address obstacles such as insurance policy changes, coding updates, and denial management. Staying ahead of these challenges is crucial for maintaining efficient and effective claim processing workflows.
Insurance Policy Changes
Changes in insurance policies, coverage requirements, or reimbursement guidelines can pose challenges for claim processing. Billers need to stay informed and adapt their practices to ensure compliance with the latest policy regulations. These changes may require additional training or updates to the billing system, potentially impacting the number of claims a biller can process per day.
Coding Updates
Medical coding is constantly evolving, with updates and revisions to coding guidelines and code sets. Billers need to stay abreast of these updates to accurately assign codes to diagnoses, procedures, and services. Coding updates may require additional research or training, potentially impacting the biller’s productivity and the number of claims processed per day.
Denial Management
Managing claim denials and rejections is an ongoing challenge in claim processing. Denied claims need to be reviewed, corrected, and resubmitted in a timely manner to ensure optimal reimbursement. Denial management processes can be time-consuming and resource-intensive, potentially slowing down the overall claim processing workflow.
Outsourcing Options for Claim Processing

Third-Party Billing Services
Outsourcing claim processing to a third-party billing service can be an effective solution for healthcare organizations looking to streamline their operations and increase efficiency. Third-party billing services specialize in claim processing and revenue cycle management, utilizing advanced technology systems and experienced billing staff to optimize the claim submission process. Outsourcing can free up internal resources and enable billers to focus on other critical tasks, potentially improving the number of claims processed per day.
Remote Billers
Remote billers offer another outsourcing option for claim processing. With remote billers, healthcare organizations can tap into a pool of experienced billing professionals who work remotely and provide billing services remotely. Remote billers can handle a high volume of claims from various locations, allowing healthcare organizations to benefit from their expertise without the need for physical office space or additional staff.
Cost Considerations
When considering outsourcing options for claim processing, it is important to weigh the costs associated with outsourcing against the potential benefits. Outsourcing may involve additional fees or contractual agreements, which need to be evaluated in terms of the value provided. The impact on the number of claims processed per day should be a key consideration when assessing the cost-effectiveness of outsourcing options.
Improving Claim Processing Efficiency

Automation Tools
Automation tools can significantly enhance claim processing efficiency. These tools can automate repetitive tasks, such as data entry and claim submission, reducing the time and effort required for manual processing. Advanced automation tools, such as artificial intelligence and machine learning algorithms, can also help identify potential errors or inconsistencies in claims, enabling billers to make timely corrections. By leveraging automation tools, billers can process a higher volume of claims per day with greater accuracy and efficiency.
Process Optimization
Optimizing the claim processing workflow is essential for achieving maximum efficiency. This can involve analyzing the existing processes, identifying bottlenecks, and implementing improvements to streamline the workflow. Process optimization may include standardizing coding practices, implementing quality control measures, and automating manual tasks. By optimizing the workflow, billers can process claims more quickly and accurately, potentially increasing the number of claims processed per day.
Effective Communication
Clear and effective communication among various stakeholders is crucial for efficient claim processing. This includes effective communication between billers and healthcare providers, as well as with insurance companies and patients. A streamlined communication process, supported by technology solutions such as secure messaging platforms or electronic claim status tracking, can minimize delays in claims processing and ensure timely resolution of any issues or questions that may arise during the process.
Regular Performance Evaluation
Regular performance evaluation is essential for identifying areas of improvement and ensuring ongoing efficiency in claim processing. By monitoring key performance indicators, such as claims processed per hour, accuracy rates, and error resolution time, healthcare organizations can track the performance of their billing staff and identify opportunities for optimization. Performance evaluations can also help identify training needs or additional support required by billers to improve their productivity and effectiveness.
Addressing Increased Claim Volumes
Scaling Up Resources
When faced with an increased claim volume, healthcare organizations may need to consider scaling up their resources to ensure timely and accurate claim processing. This can involve hiring additional billing staff, investing in advanced technology systems, or outsourcing claim processing to third-party services. Scaling up resources can help alleviate the workload on individual billers and enable them to handle a larger volume of claims per day.
Queue Management
Implementing effective queue management strategies can help billers handle increased claim volumes more efficiently. This can involve prioritizing claims based on urgency, complexity, or reimbursement potential. By effectively managing the claim queue, billers can allocate their time and resources more effectively, ensuring that high-priority claims are processed in a timely manner while addressing lower-priority claims as capacity allows.
Workflow Analysis
Analyzing the existing claim processing workflow can help identify opportunities for streamlining and optimizing the process. By conducting a thorough workflow analysis, healthcare organizations can identify potential bottlenecks, redundancies, or inefficiencies that may be impeding the claim processing efficiency. Workflow analysis can help highlight areas for improvement and guide the implementation of measures to handle increased claim volumes more effectively.
Conclusion
Finding the right balance in the number of claims a biller should process per day is crucial for maintaining productivity and accuracy in claim processing. Factors such as claim complexity, staff efficiency, system automation, and claim volume should be considered when determining the optimal workload for billers. By following recommended industry standards, prioritizing high-value claims, utilizing technology solutions, and investing in continuous training, healthcare organizations can improve claim processing efficiency and maximize reimbursement. It is important to adapt to industry changes, continuously evaluate performance, and strive for continuous improvement in claim processing practices. By finding the right balance and implementing effective strategies, healthcare organizations can ensure efficient claim processing while maintaining high accuracy rates and minimizing errors and burnout among billing staff.