To become a medical coder, obtaining the right degree is crucial. As the healthcare industry continues to grow, so does the demand for professionals trained in accurately coding medical records. With the complex nature of the job, it is essential to possess a strong foundation in medical terminology, anatomy, physiology, and coding systems. While a degree in healthcare administration, health information management, or related fields can be beneficial, it is not always a strict requirement. In this article, we will explore the various educational paths available to aspiring medical coders, enabling you to make an informed decision about the degree that best suits your career aspirations.
Introduction
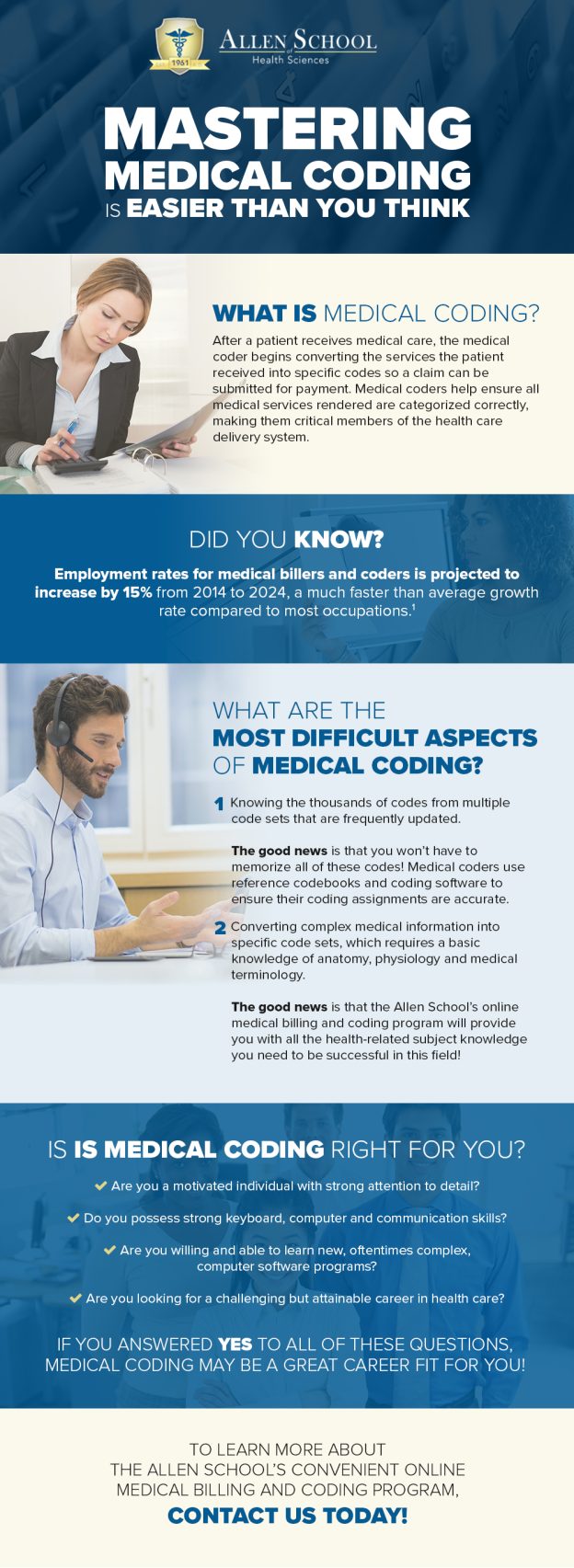
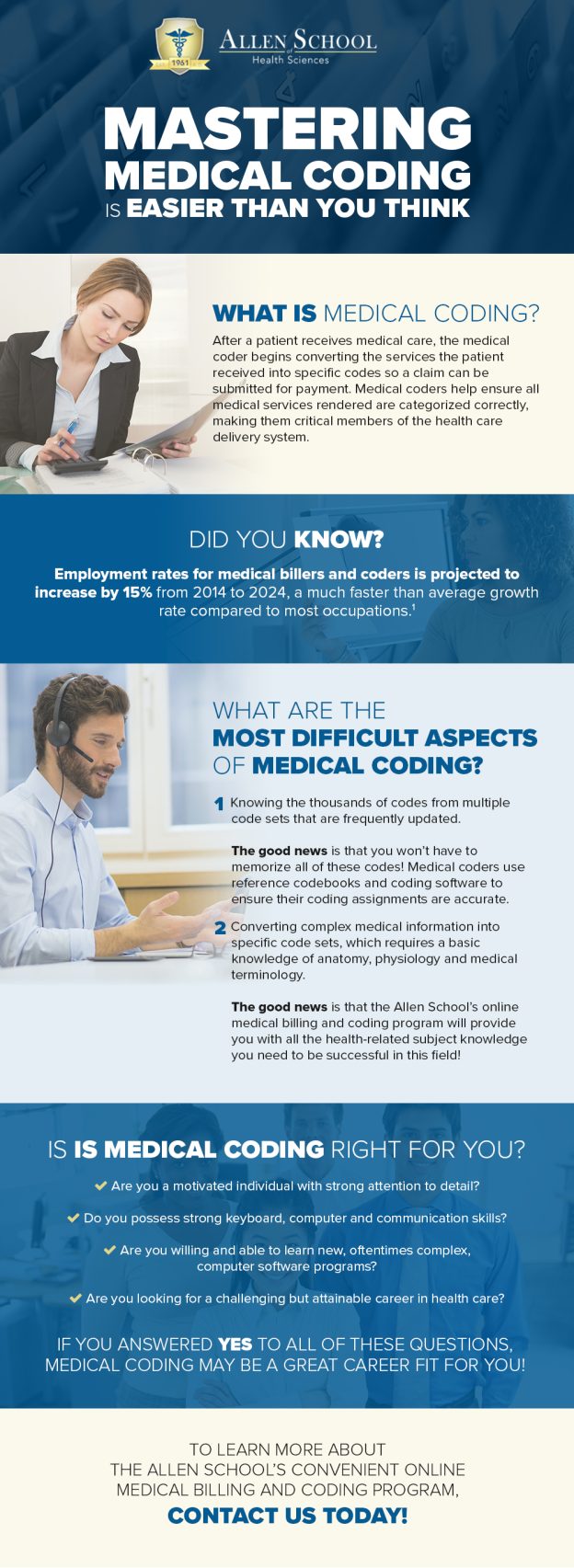
Medical coding is an essential component of the healthcare industry, serving as a universal language that translates complex medical procedures, diagnoses, and treatments into a standardized code. This coding system plays a crucial role in various aspects of healthcare, from billing and reimbursement to research and quality improvement. If you are interested in pursuing a career in medical coding, it is important to have a clear understanding of the educational requirements and certifications necessary for success in this field. This article will provide a comprehensive guide to the degrees and certifications needed to become a medical coder, as well as the benefits of higher education and the importance of practical experience.
Understanding Medical Coding

Definition of Medical Coding
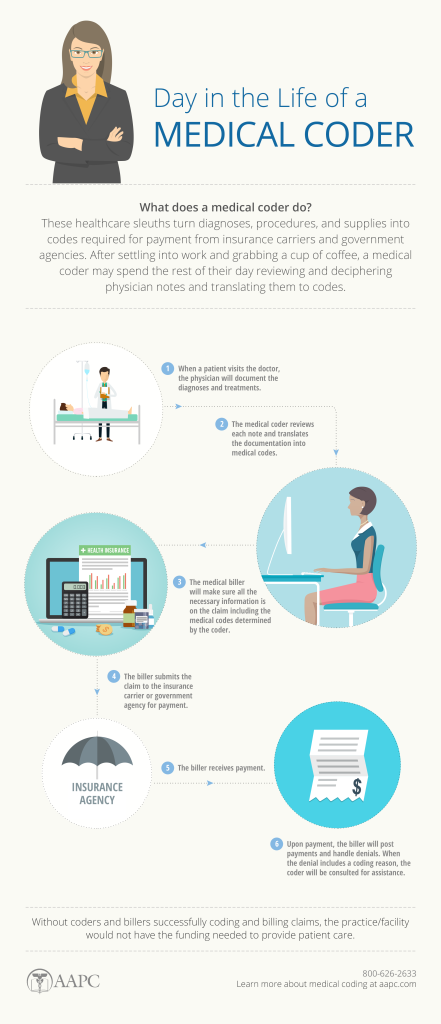
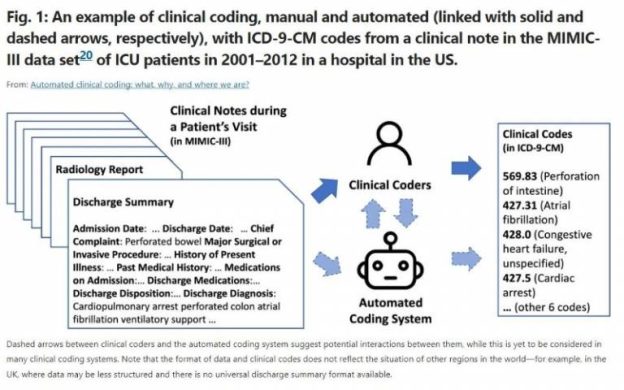
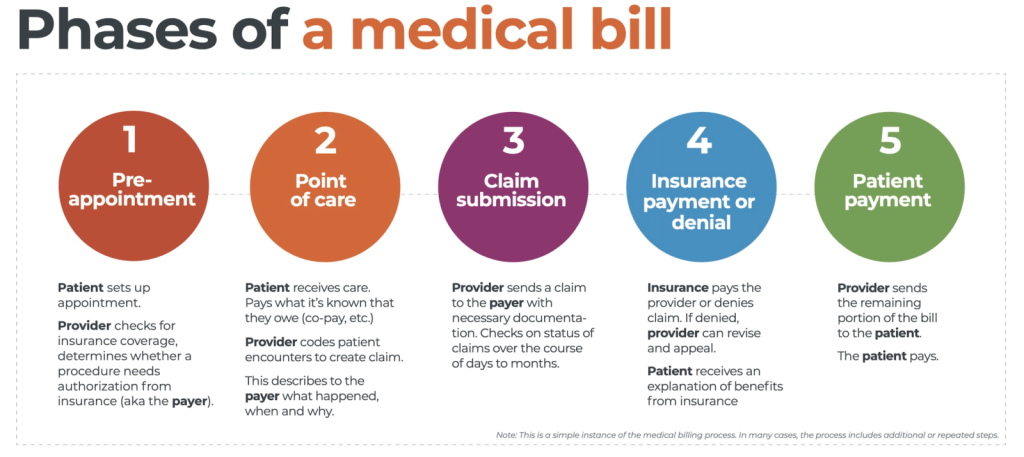
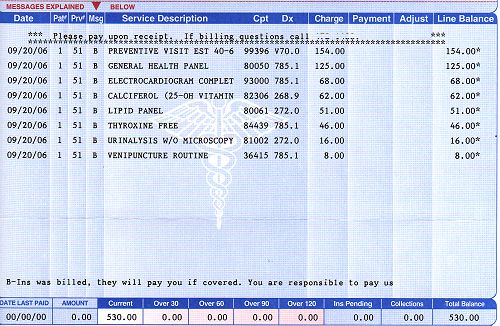
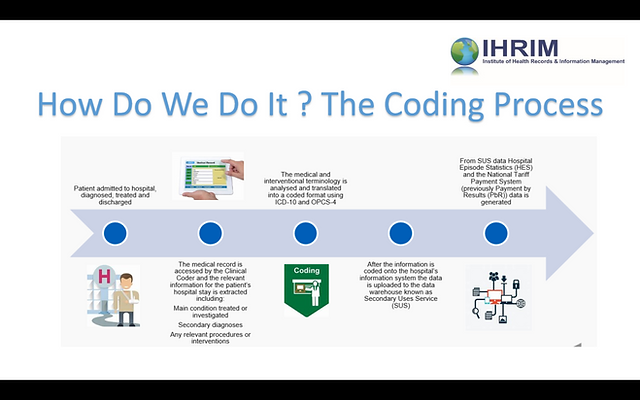
Medical coding involves the translation of medical records, such as physician’s notes, laboratory results, and radiology reports, into alphanumeric codes. These codes are standardized and used to identify diagnoses, procedures, and services provided in healthcare settings. The most commonly used coding system is the International Classification of Diseases (ICD), which is maintained by the World Health Organization (WHO). Other coding systems include Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS).
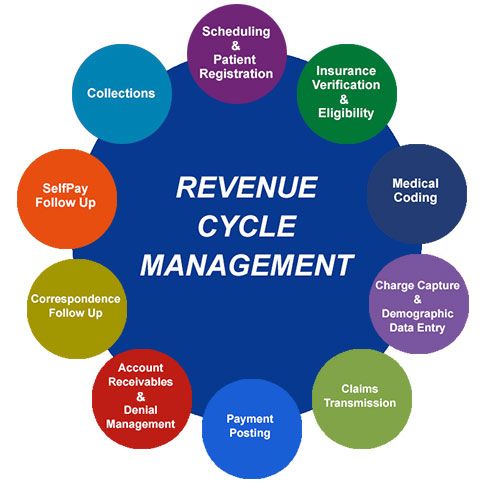
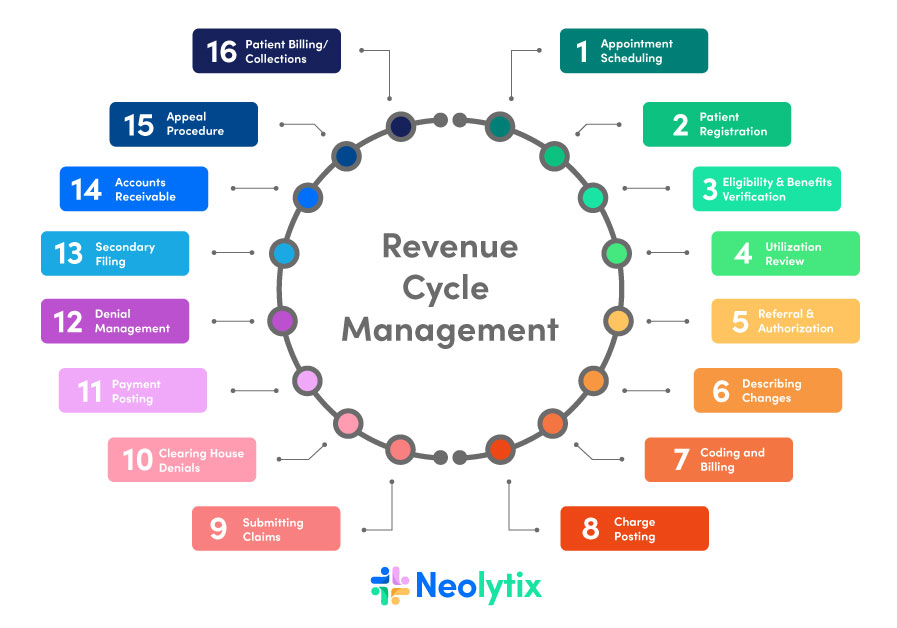
Importance of Medical Coding
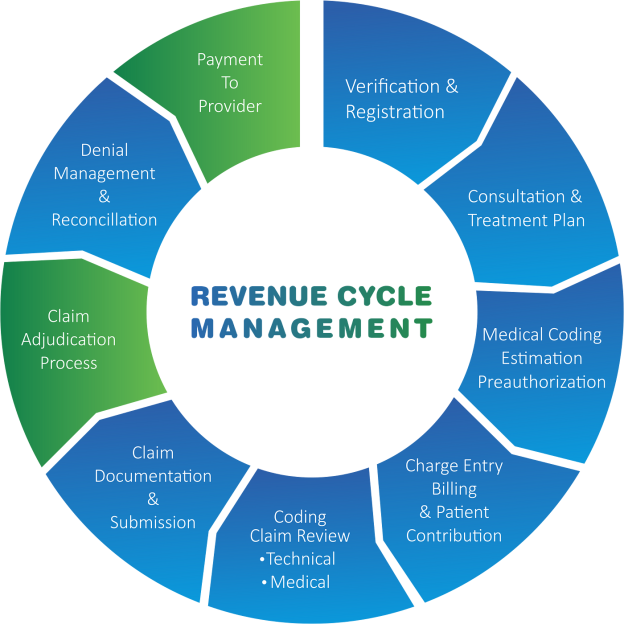
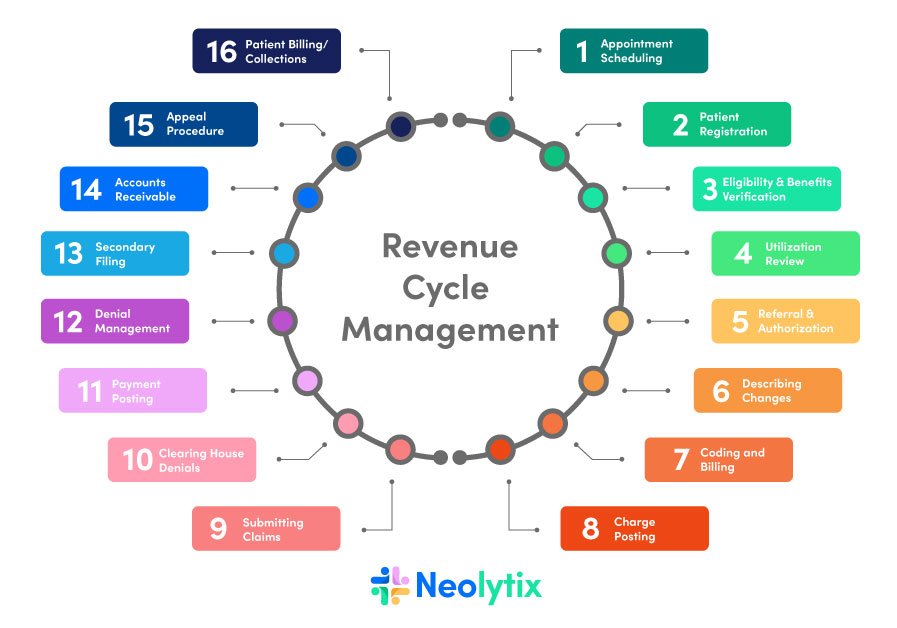
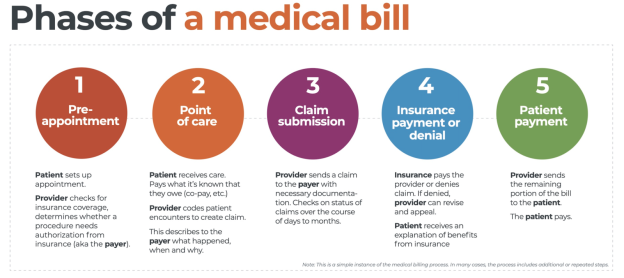
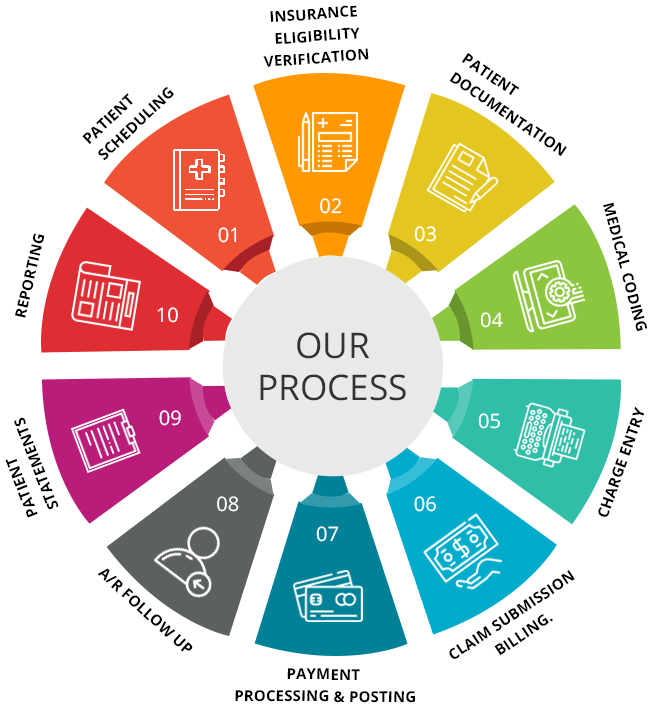
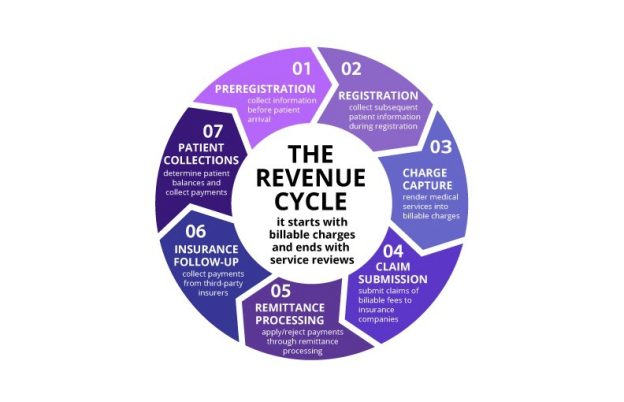
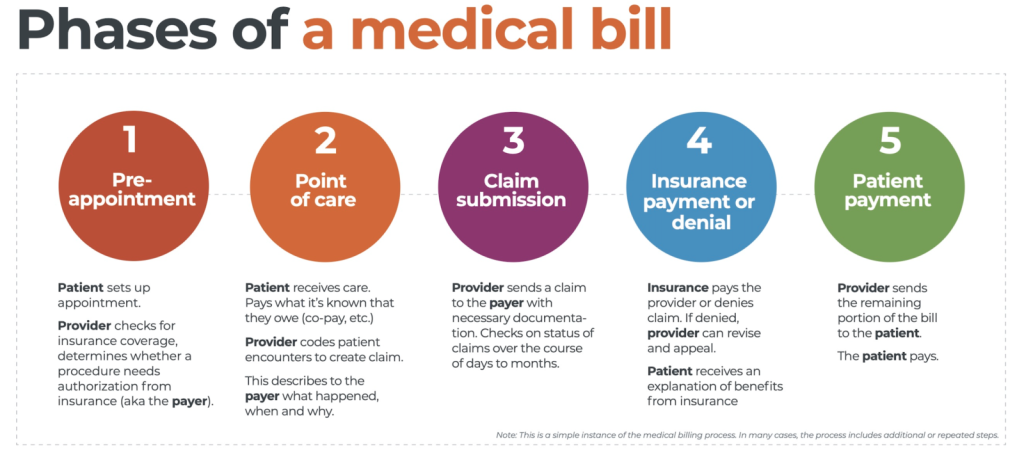
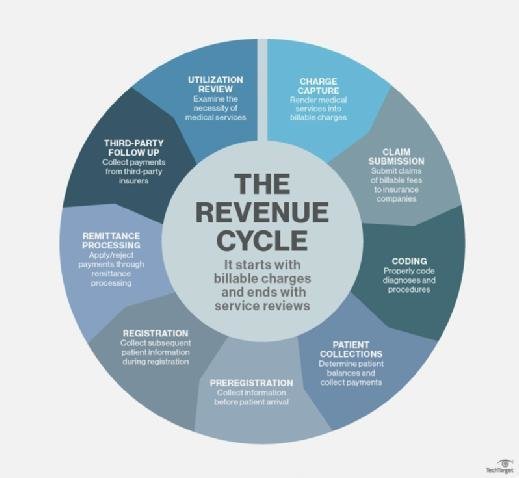
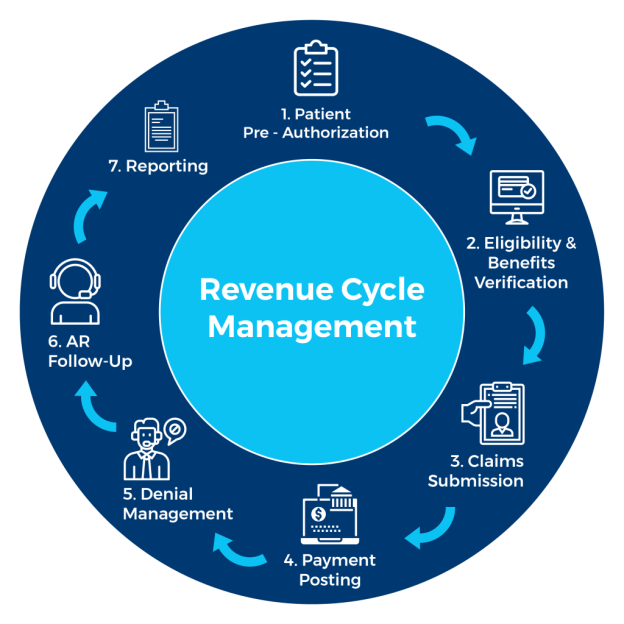
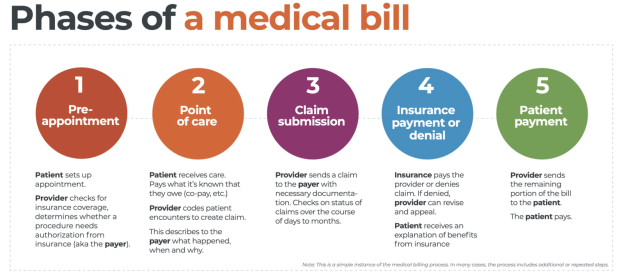
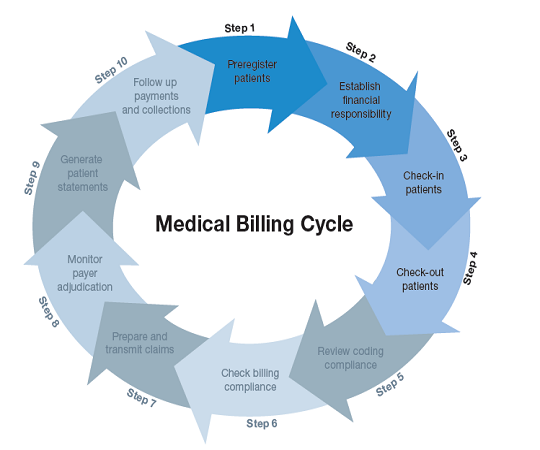
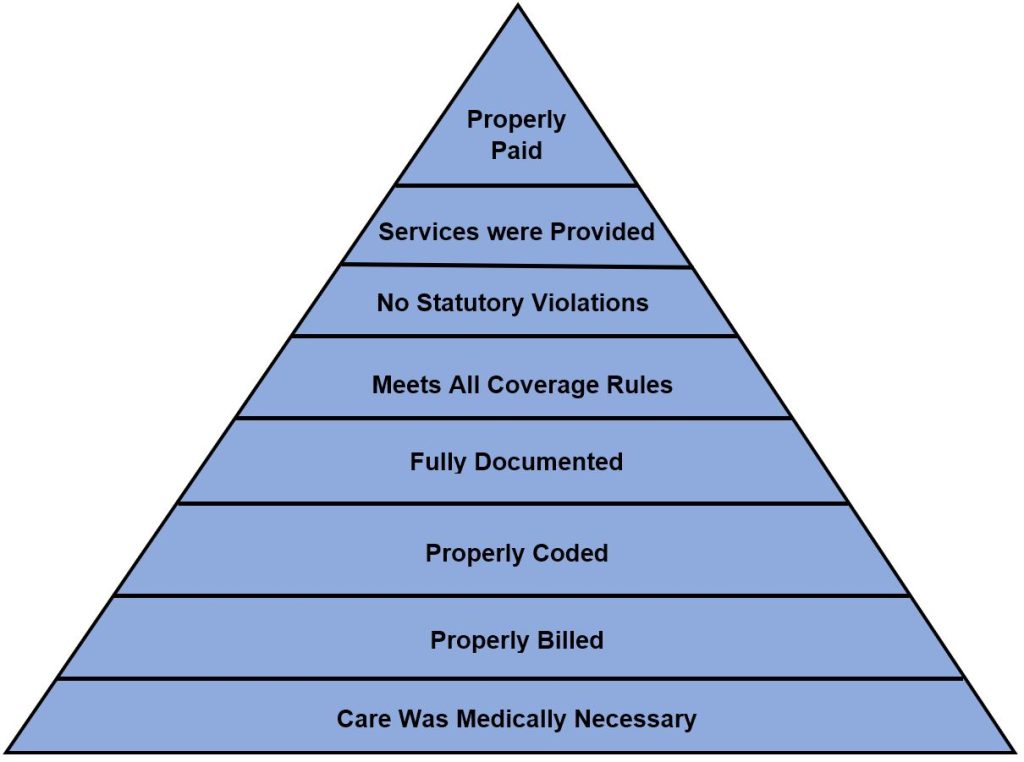
Accurate and comprehensive medical coding is crucial in healthcare for several reasons. Firstly, it is essential for proper billing and reimbursement. Insurance companies, including Medicaid and Medicare, require accurate coding to process claims and determine the appropriate payment for healthcare services. Medical coding also plays a vital role in healthcare analytics, research, and quality improvement initiatives. Coded data is used to analyze patient outcomes, identify trends, and support evidence-based decision making. Additionally, coding ensures compliance with regulatory requirements and facilitates the sharing of medical information between healthcare professionals.
Role of Medical Coders
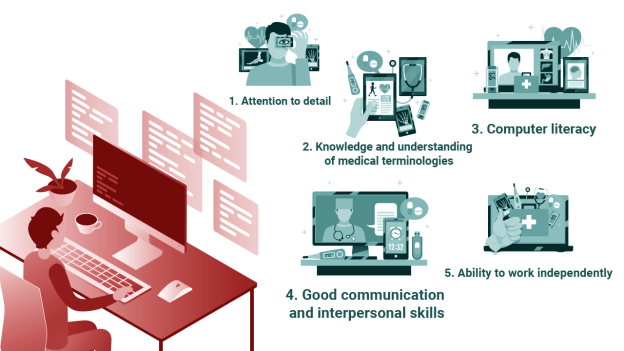
Medical coders are professionals who specialize in assigning codes to medical diagnoses, procedures, and services. These codes are derived from patients’ medical records using specialized coding manuals and software. The primary responsibility of medical coders is to ensure that the codes accurately reflect the information documented by healthcare providers. They must possess a strong understanding of anatomy, medical terminology, and coding guidelines to complete this task efficiently. Medical coders work in various healthcare settings, including hospitals, clinics, physician’s offices, and insurance companies.
Educational Requirements for Medical Coders
This image is property of 150033344.v2.pressablecdn.com.
High School Diploma or GED
To pursue a career in medical coding, a high school diploma or General Educational Development (GED) certificate is typically the minimum educational requirement. It is essential to have a solid foundation in subjects such as English, mathematics, biology, and computer science.
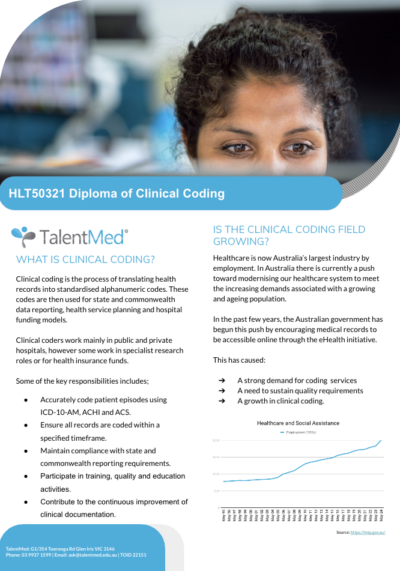
Medical Coding Certificate or Diploma
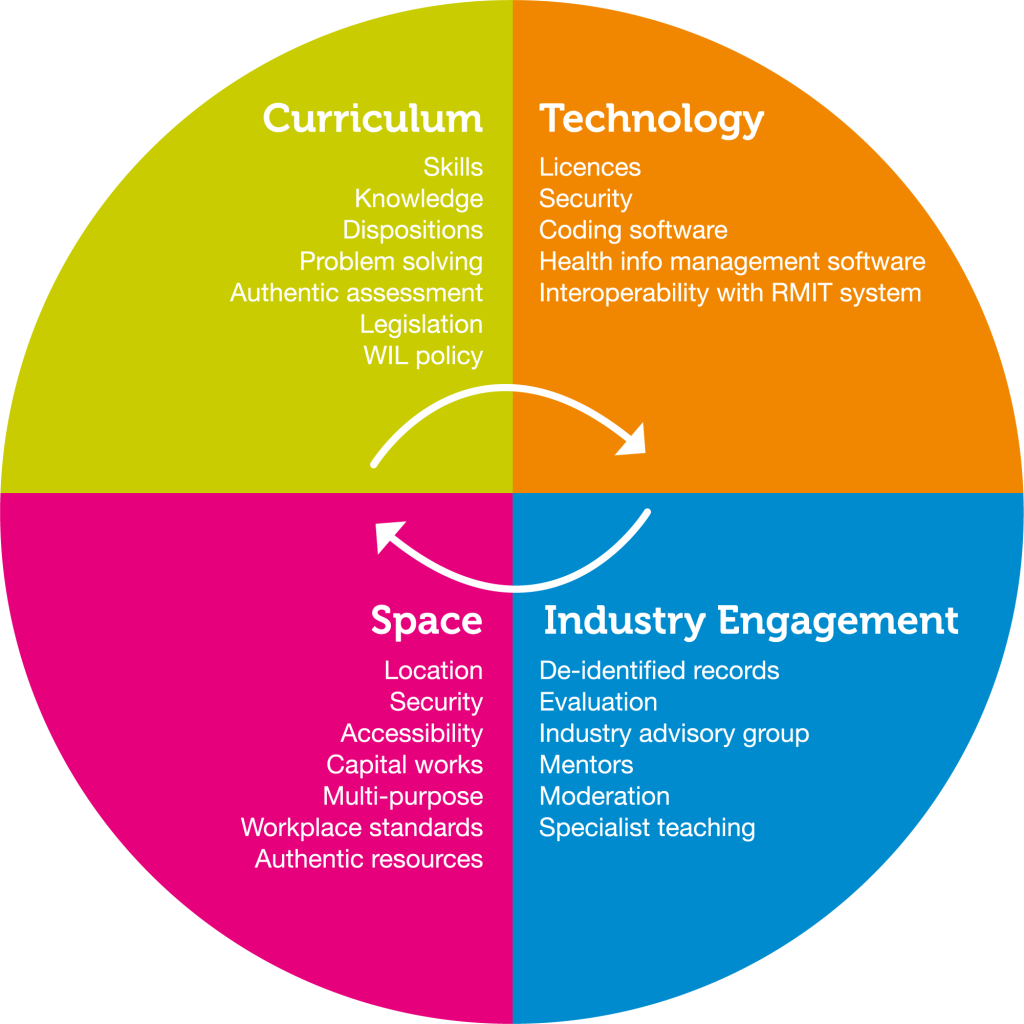
While a high school diploma or GED is the basic requirement, specialized training in medical coding is necessary to develop the skills and knowledge needed for this profession. Many vocational schools, community colleges, and online institutions offer certificate or diploma programs in medical coding. These programs typically cover essential topics such as medical terminology, anatomy and physiology, coding guidelines, and healthcare reimbursement systems.
Associate Degree in Medical Coding
An associate degree in medical coding is a higher level of education that can provide more comprehensive knowledge and skills in this field. This degree program typically includes coursework in advanced medical coding, health information management, healthcare law and ethics, and healthcare statistics. An associate degree may also offer opportunities for hands-on experience through internships or practicum placements.
Bachelor’s Degree in Health Information Management
While not specifically focused on medical coding, a bachelor’s degree in health information management (HIM) can provide a broader understanding of healthcare administration and technology. This degree program often covers topics such as healthcare data analysis, healthcare finance, privacy and security of health information, and leadership in healthcare. A bachelor’s degree can enhance career prospects and open doors to advanced roles in healthcare, including management positions.
Certified Professional Coders (CPC) Credential

Importance of CPC Credential
obtaining the Certified Professional Coders (CPC) credential is highly valued in the medical coding profession. CPC certification demonstrates proficiency in medical coding and validates the coder’s expertise in accurately assigning codes to medical diagnoses, procedures, and services. Employers often prefer to hire certified coders as it assures them of the coder’s competence and adherence to industry standards.
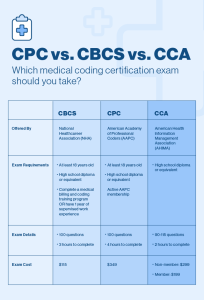
Eligibility Criteria for CPC Credential
To be eligible for the CPC credential, candidates must have at least two years of professional coding experience or an equivalent combination of education and experience. The experience requirement can be fulfilled through practical coding work, coding courses, or a combination of both. Additionally, candidates must pass the CPC examination, which evaluates their knowledge of coding guidelines, medical terminology, anatomy, and coding practices.
Examination Process
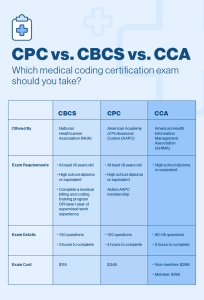
The CPC examination is administered by the American Academy of Professional Coders (AAPC) and consists of multiple-choice questions that assess various aspects of medical coding knowledge and skills. The examination covers topics such as ICD-10-CM, CPT, HCPCS Level II coding, anatomy, and medical terminology. Candidates have five hours and 40 minutes to complete the exam, which totals 150 questions. Achieving a passing score is necessary to obtain the CPC credential.
Maintaining CPC Certification
To maintain the CPC certification, certified coders must fulfill certain requirements set by the AAPC. This includes earning a specified number of continuing education units (CEUs) within a specific time frame. CEUs can be obtained through participation in workshops, conferences, webinars, and other educational activities related to medical coding. Maintaining CPC certification demonstrates an ongoing commitment to professional development and staying updated with industry changes.
Other Relevant Degrees/ Certifications
The journey to mastering this intricate field demands consistency, effective time management, and a willingness to seek support and mentorship. In this discussion, we’ll delve into the significance of these factors and how they contribute to a fruitful learning experience and a promising career in medical billing and coding.
Certified Coding Specialist (CCS) Credential
The Certified Coding Specialist (CCS) credential is offered by the American Health Information Management Association (AHIMA) and focuses on inpatient coding. This credential validates proficiency in assigning accurate codes for diagnoses, procedures, and services performed in hospitals and other inpatient settings. The CCS examination assesses a candidate’s knowledge of ICD-10-CM/PCS coding guidelines, medical terminology, pharmacology, and healthcare reimbursement systems.
Certified Coding Associate (CCA) Credential
The Certified Coding Associate (CCA) credential, also offered by AHIMA, is an entry-level certification that validates basic coding skills. This credential is suitable for individuals who are new to the field of medical coding or have minimal coding experience. The CCA examination covers topics such as ICD-10-CM coding, medical terminology, anatomy, and coding guidelines.
Registered Health Information Technician (RHIT) Certification
While not specific to medical coding, the Registered Health Information Technician (RHIT) certification offered by AHIMA can be valuable for individuals seeking advanced roles in health information management. This certification validates expertise in managing and analyzing healthcare data, implementing health information systems, and ensuring compliance with privacy and security regulations. RHIT-certified professionals are well-equipped to handle the data management aspects of medical coding.
Benefits of Higher Education in Medical Coding

Enhanced Job Opportunities
Obtaining a higher degree or certification in medical coding can significantly enhance job opportunities in this field. While a high school diploma or certificate program can provide a foundation, higher education demonstrates a deeper understanding of medical coding concepts and may make candidates more competitive in the job market. Employers often prioritize candidates with additional education, especially for roles that require more advanced coding knowledge and skills.
Higher Salary Potential
Higher education in medical coding can also lead to increased earning potential. According to the Bureau of Labor Statistics (BLS), individuals with a higher level of education tend to earn higher salaries in the healthcare industry. The additional knowledge and skills gained through an associate or bachelor’s degree can make coders more valuable to employers, resulting in better salary opportunities.
Expanded Knowledge and Skills
Higher education programs in medical coding provide a comprehensive curriculum that goes beyond the basics covered in entry-level programs. Associate and bachelor’s degree programs cover advanced coding topics, healthcare management principles, legal and ethical considerations, and healthcare technology. This broader knowledge base can enhance the coder’s ability to analyze complex medical records, identify coding discrepancies, and ensure accurate code assignment.
Career Advancement Opportunities
Advanced degrees or certifications can open doors to higher-level positions in the healthcare industry. With a bachelor’s degree in health information management or related fields, certified coders can pursue roles such as coding supervisor, coding manager, or health information manager. These positions often involve leadership responsibilities, decision-making authority, and involvement in strategic initiatives. Higher education provides the necessary skills and knowledge to take on these advanced roles.
Importance of Practical Experience

This image is property of www.allenschool.edu.
Internships and Externships
While formal education provides valuable theoretical knowledge, practical experience is equally important in the field of medical coding. Many educational programs offer internships or externships that allow students to gain hands-on experience in medical coding settings. These opportunities provide valuable real-world exposure and help students apply their knowledge in a practical environment. Internships and externships also provide networking opportunities and may lead to job offers upon completion.
On-the-Job Training
For individuals who enter the field of medical coding without formal education, on-the-job training can be essential for gaining practical experience and knowledge. Employers often offer training programs that allow individuals to learn coding skills while working under the supervision of experienced coders. This approach provides valuable hands-on learning and allows individuals to develop their coding proficiency over time.
Continuing Education and Professional Development
Medical coding is a dynamic field with evolving guidelines and regulations. To stay up-to-date with industry changes, medical coders must engage in continuing education and professional development activities. Attending workshops, webinars, and conferences, as well as pursuing advanced certifications and credentials, can enhance coding skills and keep coders current with the latest coding practices. Continuing education demonstrates a commitment to ongoing professional growth and ensures that coders are well-equipped to handle new coding challenges.
Career Prospects for Medical Coders

Job Settings for Medical Coders
Medical coders work in various healthcare settings, including hospitals, outpatient clinics, physician’s offices, insurance companies, government agencies, and consulting firms. The demand for medical coders exists in both the private and public sectors, providing a wide range of opportunities in diverse work environments. Some coders may also choose to work remotely as independent contractors or telecommute for healthcare organizations.
Job Growth and Demand
According to the BLS, the employment of medical records and health information technicians, which includes medical coders, is projected to grow 8% from 2019 to 2029, much faster than the average for all occupations. This growth is driven by an aging population, which leads to an increased need for healthcare services and subsequent medical coding. The demand for skilled medical coders is expected to remain high, presenting favorable job prospects for individuals in this field.
Potential Career Paths
A career in medical coding can be a stepping stone to various career paths within the healthcare industry. With experience and continued education, medical coders can progress to managerial or supervisory roles, overseeing coding departments or health information management teams. Coders with an interest in data analysis and informatics may pursue careers as healthcare data analysts or health information systems specialists. Additionally, medical coding can serve as a foundation for further specialization in areas such as medical billing, auditing, or compliance.
This image is property of www.rasmussen.edu.
Conclusion
In conclusion, a career in medical coding offers numerous opportunities for individuals interested in healthcare, technology, and data analysis. While a high school diploma or GED is the minimum requirement, obtaining a specialized certificate, diploma, associate degree, or bachelor’s degree in medical coding or related fields can significantly enhance job prospects and earning potential. Additionally, pursuing certifications such as the CPC, CCS, CCA, or RHIT credentials can further validate coding proficiency and provide a competitive edge in the job market. Practical experience through internships, on-the-job training, and continuing education is crucial for refining coding skills and staying updated with industry changes. With the demand for skilled medical coders on the rise, a career in medical coding offers stability, growth opportunities, and an integral role in the healthcare industry.