Introduction
In the world of healthcare, medical billing is a crucial process that ensures healthcare providers receive proper compensation for their services. Understanding the process of medical billing is important for both healthcare professionals and patients alike. This article will provide an overview of the medical billing process and highlight the importance of this system in the healthcare industry.
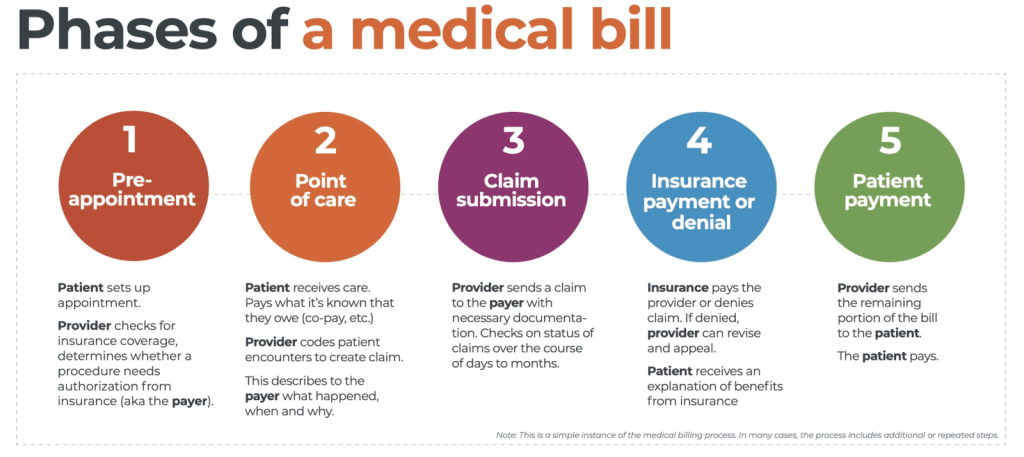
Overview of Medical Billing Process
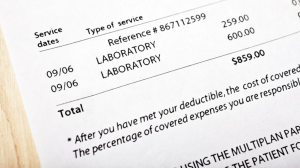
Medical billing is the process of submitting and following up on claims with health insurance companies in order to receive payment for healthcare services provided. It involves various steps such as gathering patient information, verifying insurance coverage, coding procedures, and submitting claims to insurance companies. Once submitted, the claims are reviewed by insurance companies, who then determine the amount of reimbursement for the services rendered.
Importance of Medical Billing
Medical billing plays a vital role in the healthcare industry for several reasons. Firstly, it ensures that healthcare providers receive timely and accurate payment for their services. Without proper billing, healthcare organizations would struggle to cover their expenses and continue providing quality care. Additionally, medical billing helps patients understand the costs associated with their healthcare services and navigate the complexities of insurance coverage. It also helps to maintain accurate records and documentation, which is crucial for legal and regulatory compliance.
Understanding the process of medical billing is essential for healthcare professionals and patients to ensure smooth and efficient operations within the healthcare system. By familiarizing yourself with this process, you can better navigate the financial aspects of healthcare and ensure proper reimbursement for services rendered.
This image is property of www.waystar.com.
Understanding the Process of Medical Billing
Medical billing is an essential part of the healthcare system, ensuring that healthcare providers receive payment for their services while patients navigate the complex world of insurance coverage. To grasp the process of medical billing, it is important to understand the key players involved and their respective roles.
Key Players in Medical Billing

Role of Healthcare Providers
As a patient, you play a significant role in the medical billing process. To begin, you receive medical services from healthcare providers such as doctors, nurses, and specialists. These providers document the services rendered, including treatments, procedures, and medications, in medical codes. Accurate and detailed documentation is crucial for proper billing.
Role of Insurance Companies
Insurance companies are another crucial player in medical billing. Once the healthcare provider submits the documentation, the insurance company reviews the claim, determines the coverage based on the patient’s insurance policy, and calculates the amount the patient needs to pay out-of-pocket. The insurance company then reimburses the healthcare provider for the covered services.
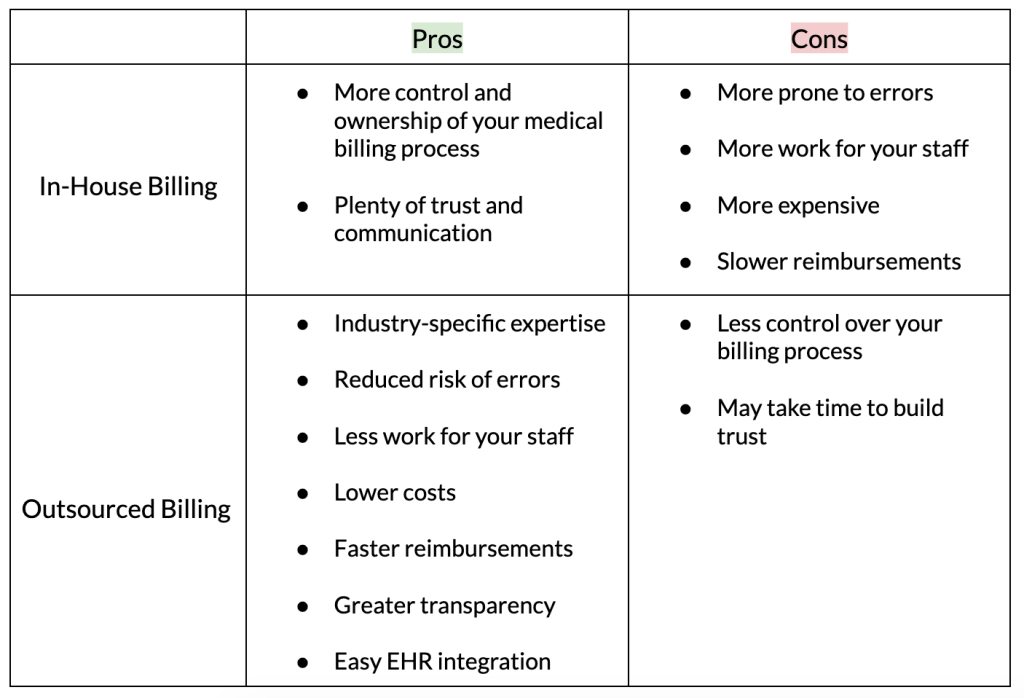
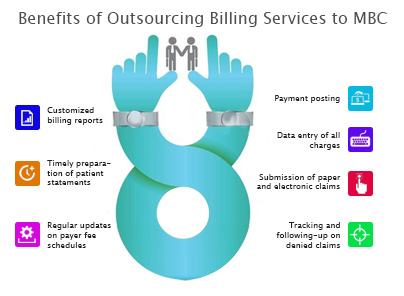
Role of Medical Billing Companies
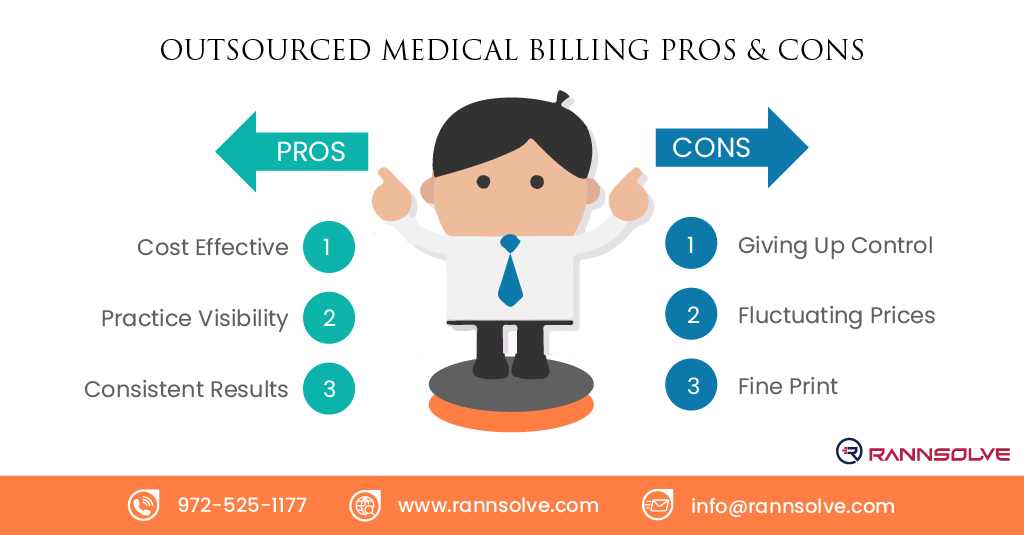
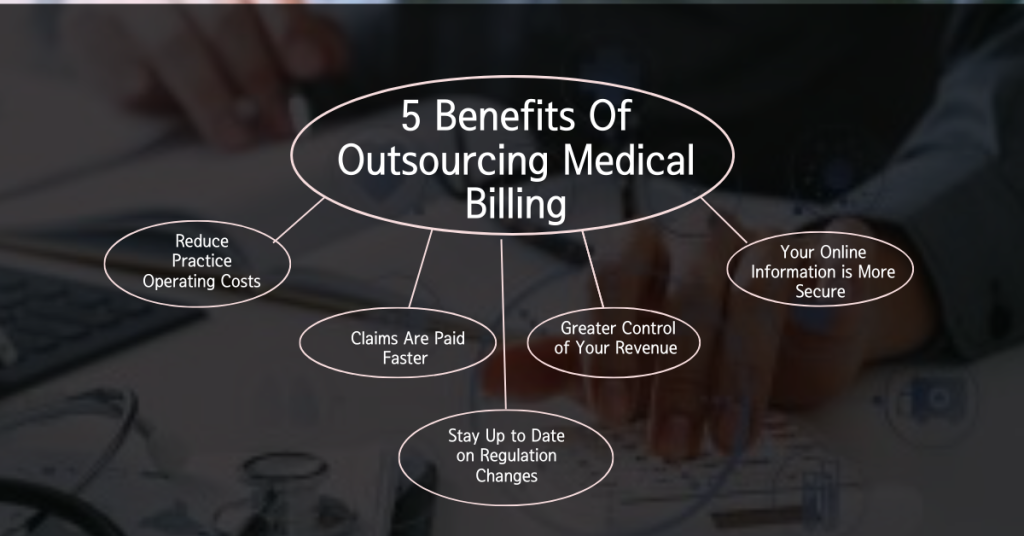
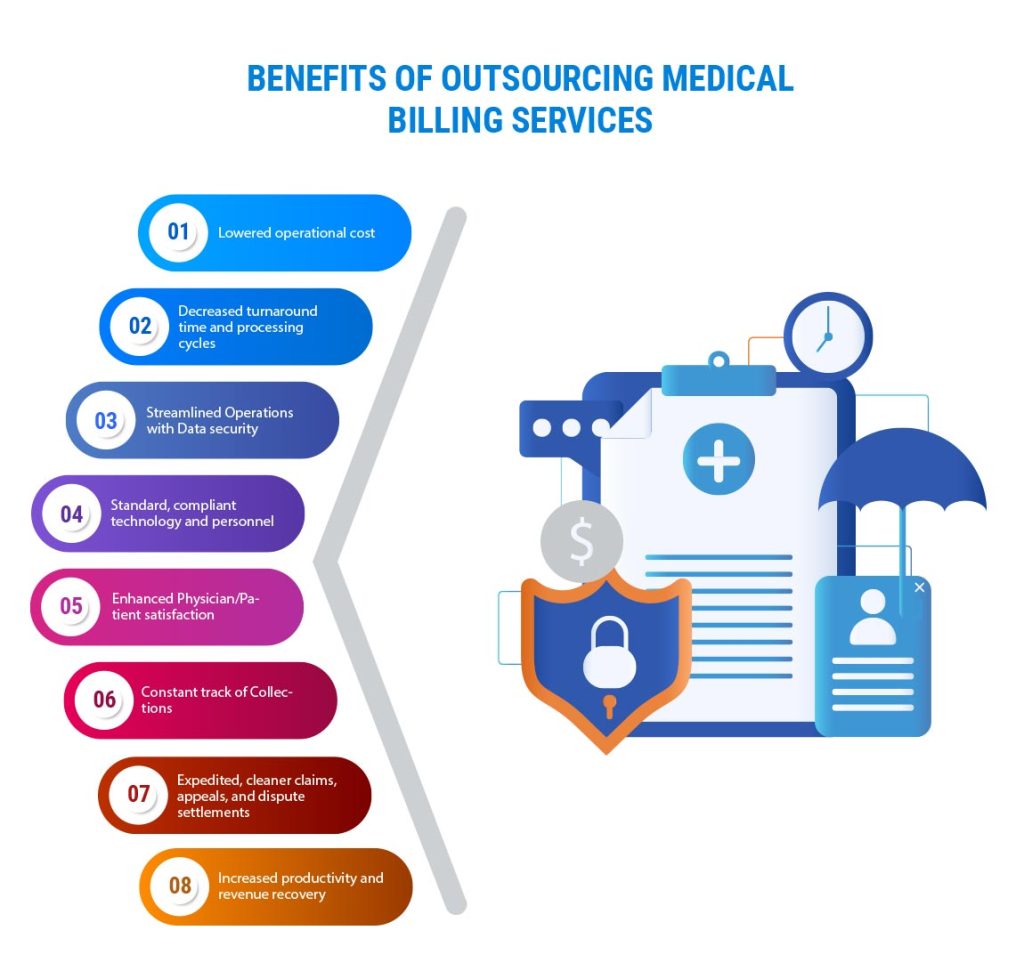
Medical billing companies act as intermediaries between healthcare providers and insurance companies. They specialize in managing the billing process, which includes submitting claims to insurance companies on behalf of healthcare providers. These companies handle the complex coding requirements, ensure accurate documentation, and follow up on rejected or denied claims. Their expertise allows healthcare providers to focus on delivering quality care to patients.
Understanding the process of medical billing involves recognizing the role of healthcare providers, insurance companies, and medical billing companies. By having a clear understanding of these key players, you can navigate the complexities of medical billing with confidence and ensure that the financial aspect of your healthcare is efficiently managed.
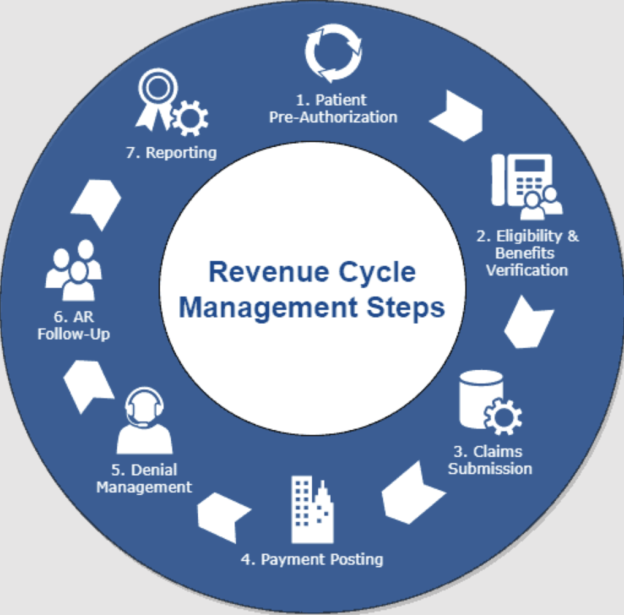
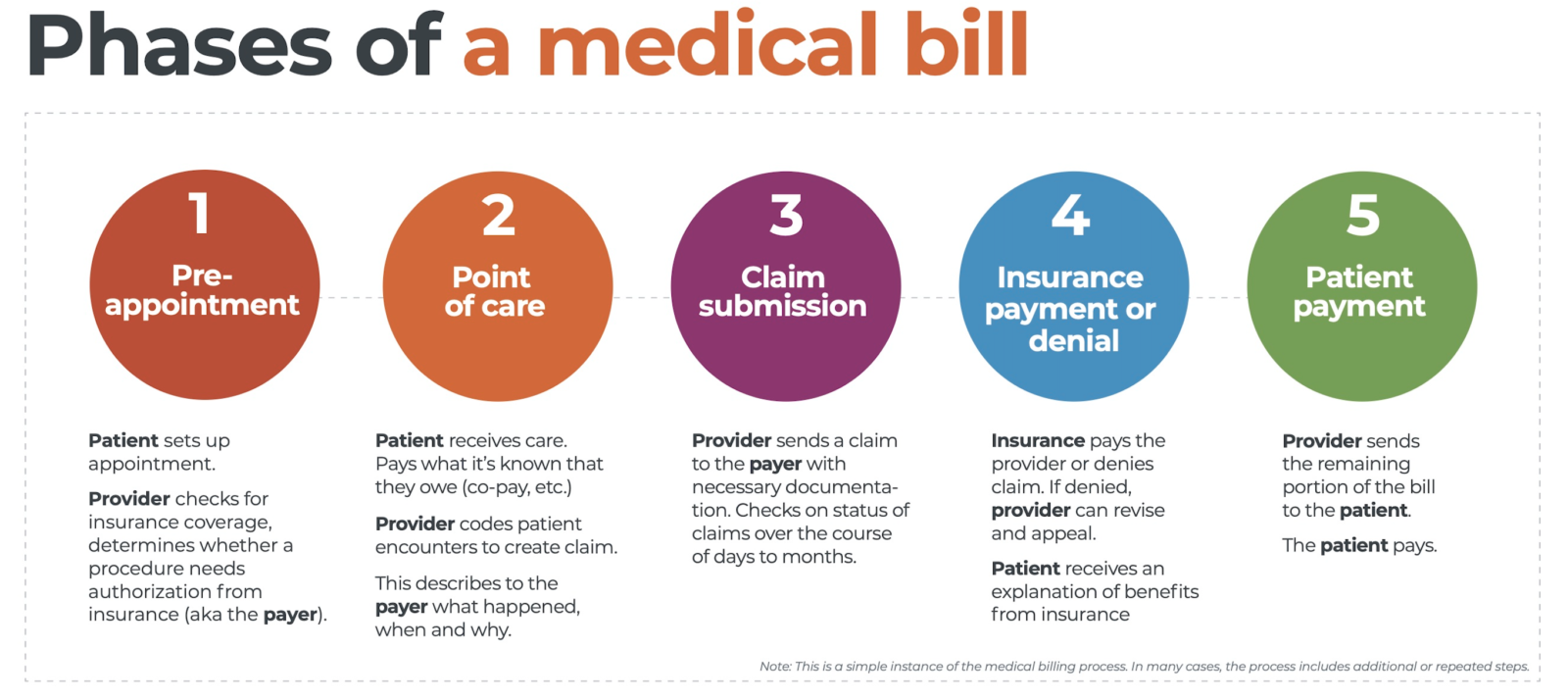
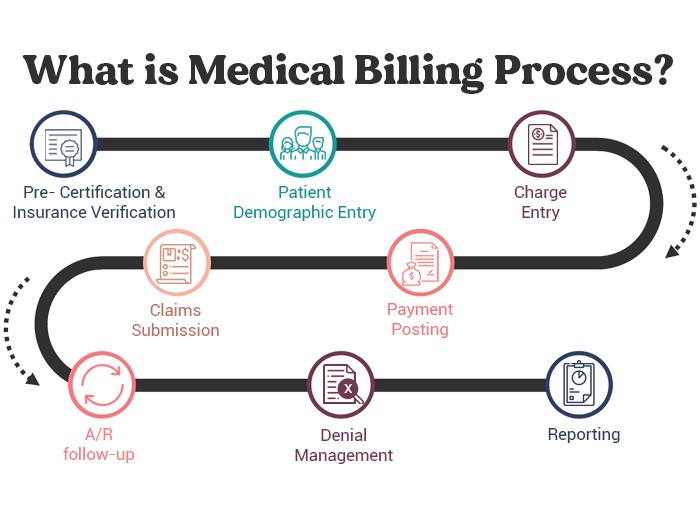
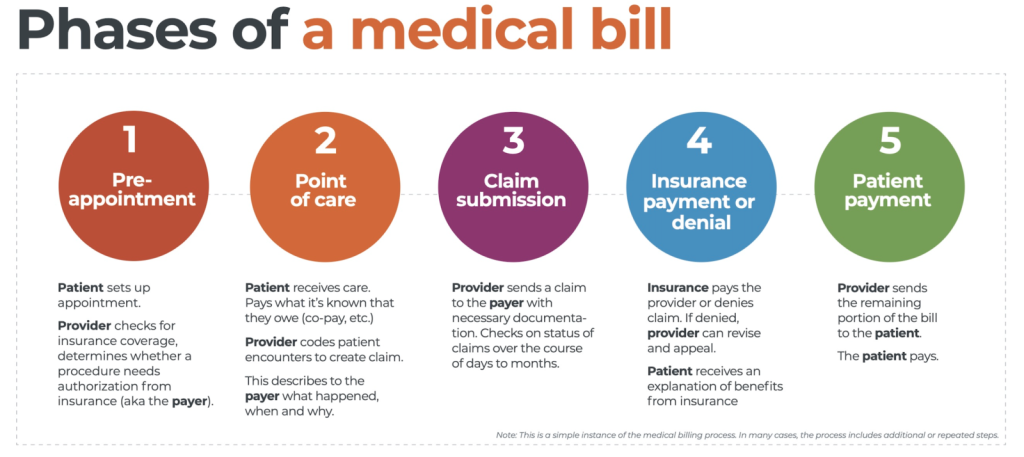
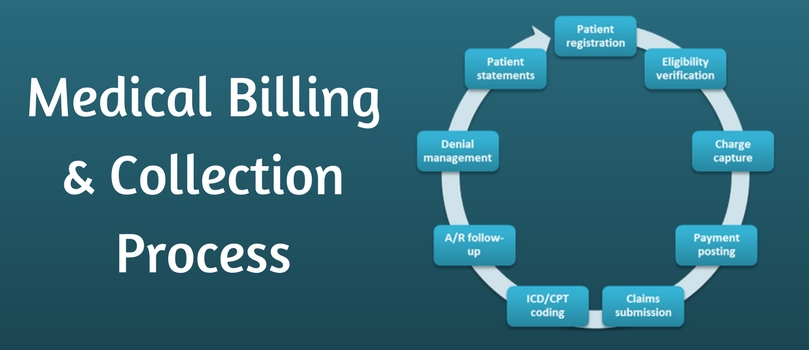
Steps in the Medical Billing Process
When it comes to medical billing, understanding the steps involved can help you navigate through the complex world of healthcare costs more effectively. This article is designed to give you a friendly overview of the entire medical billing process, from patient registration all the way to denial management.
Patient Registration
The first step in the process is patient registration. This involves gathering all necessary personal and insurance information from the patient, such as their name, address, date of birth, and insurance policy details. It is crucial to ensure that all information is accurate and up-to-date to avoid any potential billing issues later on.
Insurance Verification
Once the patient’s information has been collected, the next step is insurance verification. This involves contacting the patient’s insurance company to confirm their coverage and benefits. This step is essential to determine the patient’s financial responsibility and to ensure that the medical services provided are covered by their insurance plan.
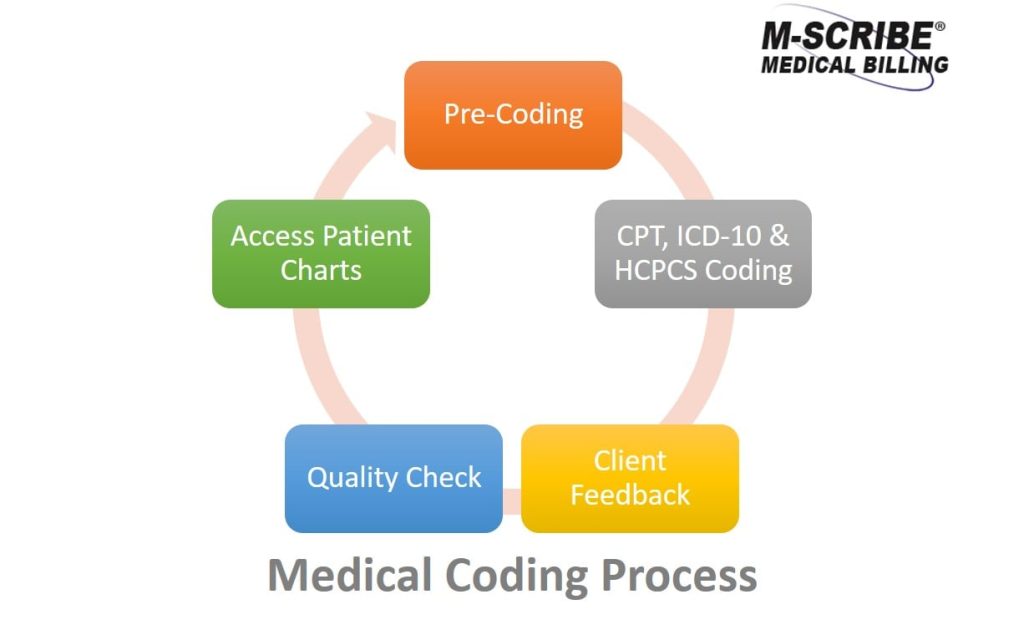
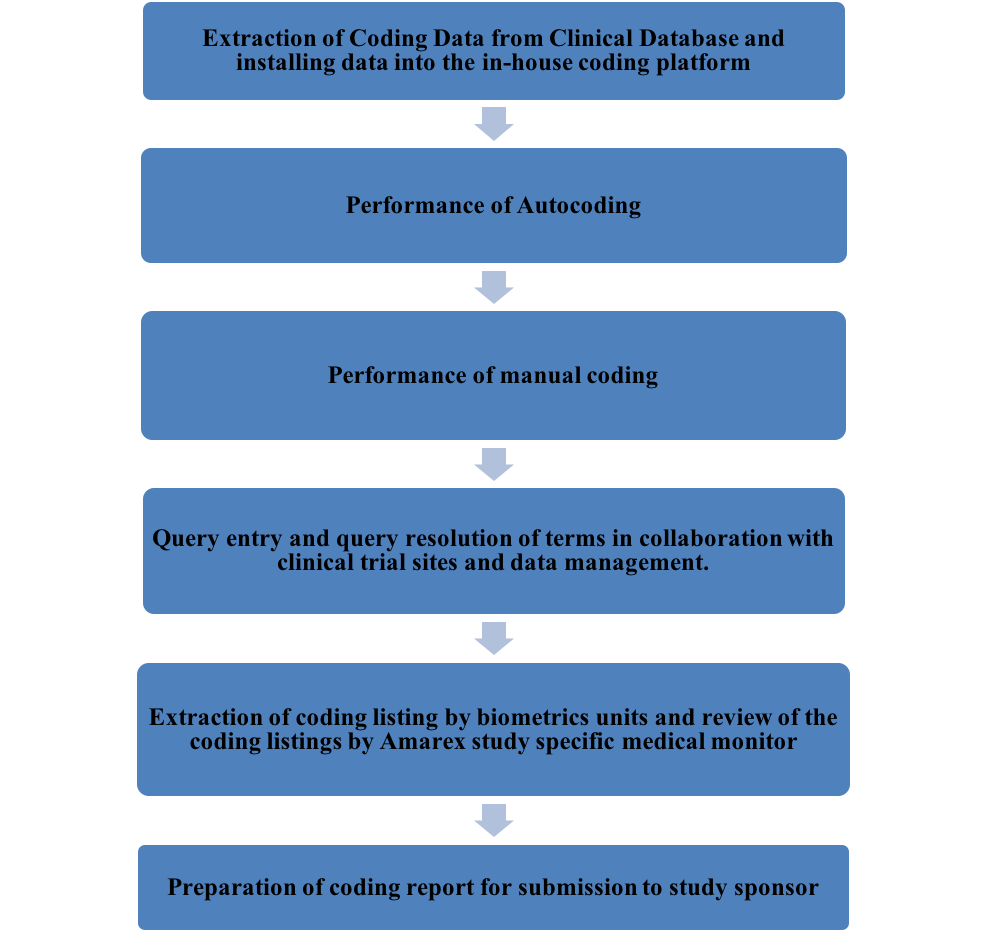
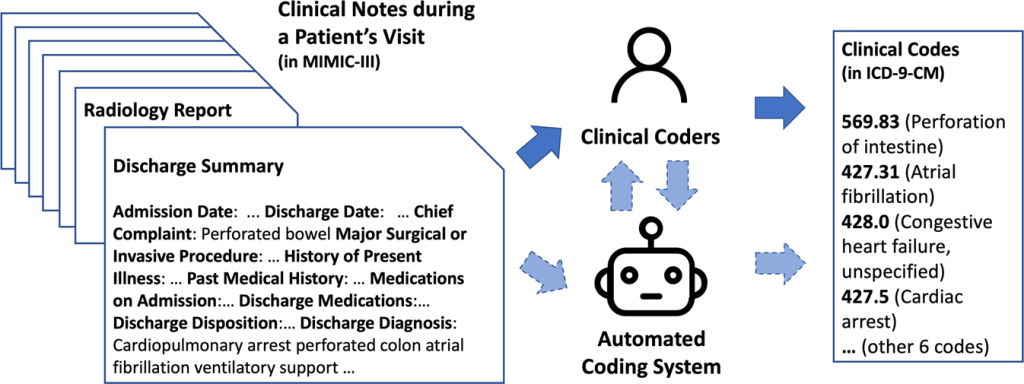
Coding and Documentation
After insurance verification, medical coders assign specific codes to the services provided based on the patient’s medical records. These codes determine the level of reimbursement from the insurance company. Accurate coding and comprehensive documentation are vital to avoid claim rejections and delays in payment.
Claims Submission
Once the coding and documentation are complete, the medical billing team submits the claims electronically or through paper submission to the appropriate insurance companies. This step includes sending all necessary documents and supporting information to substantiate the claim.
Claims Adjudication
Upon receipt of the claims, the insurance company reviews them for accuracy and determines the amount of reimbursement based on contractual agreements. The claims may go through various stages of review, including pre-determination, medical necessity review, and claim edit checks. The insurer then approves or denies the claim accordingly.
Payment Posting
Once the insurance company approves the claim, they issue payment to the healthcare provider. The billing team then posts the payment to the patient’s account, taking into consideration any patient co-pays or deductibles.
Denial Management
In some cases, claims may be denied for various reasons, such as incorrect coding or lack of medical necessity. Denial management involves reviewing denied claims, identifying the reasons for denial, and taking necessary steps to rectify the issues and resubmit the claim for reimbursement.
By understanding the steps involved in the medical billing process, you can be better prepared to navigate your healthcare journey and ensure a smoother experience when it comes to managing your medical expenses.
Medical cost concept with stethoscope and medical bill
Medical billing is an essential aspect of the healthcare industry that ensures healthcare providers receive payment for the services they render. If you’ve ever visited a doctor or hospital, you may have wondered how the billing process works. In this article, we will provide an overview of medical billing, focusing specifically on electronic medical billing.
Electronic Medical Billing
Electronic Medical Billing, also known as EMR (Electronic Medical Records) billing, is the process of submitting and tracking medical claims electronically. It has become the preferred method of billing due to its efficiency and accuracy. Here are some advantages of electronic medical billing:
Advantages of Electronic Medical Billing
- Streamlined Workflow: EMR systems automate the billing process, reducing the need for manual data entry and paperwork. This streamlines workflow and saves time for both healthcare providers and insurance companies.
- Reduced Errors: By eliminating the possibility of human error associated with manual data entry, electronic medical billing significantly reduces errors and ensures accuracy in claim submission.
Implementation and Integration of EMR Systems
EMR systems are implemented in healthcare facilities to streamline their billing processes. These systems are integrated with the facility’s electronic health record (EHR) system, allowing for seamless flow of patient data between clinical and billing departments. This integration ensures accurate billing by capturing all necessary information for claim submission.
understanding the process of medical billing, particularly electronic medical billing, is crucial in today’s healthcare landscape. It offers numerous advantages, such as streamlined workflow and reduced errors, making it an integral part of the healthcare industry.
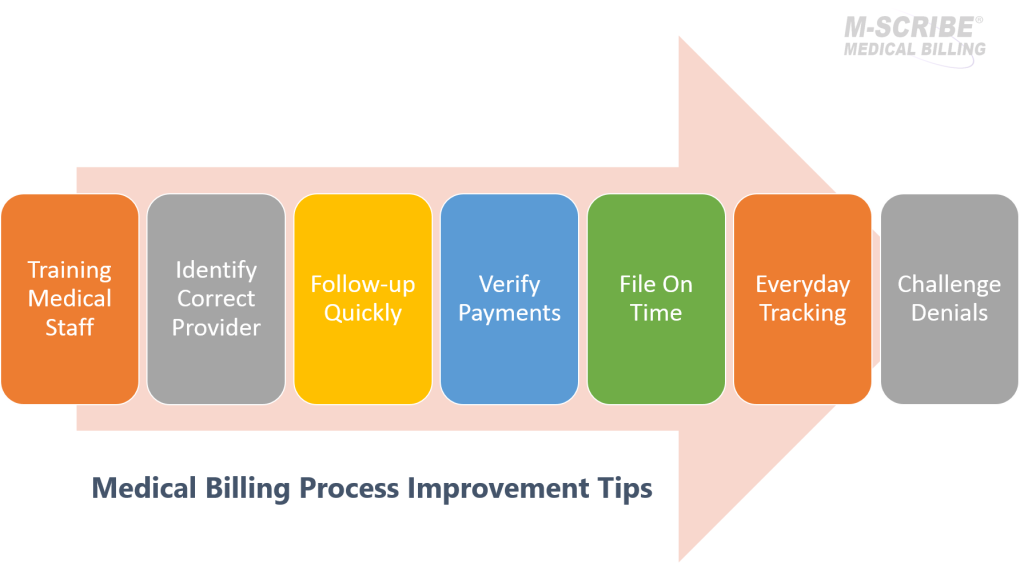
Challenges in Medical Billing

Medical Coding Errors
One of the main challenges in medical billing is dealing with medical coding errors. Medical coders play a crucial role in translating the healthcare services provided by doctors and hospitals into standardized numeric codes. These codes are then used for billing purposes and to communicate with insurance companies. However, errors can occur in this complex process. Common coding errors include entering incorrect codes, omitting important information, or failing to document the necessary details. Such errors can result in claim delays, denials, and even financial loss.
Insurance Claim Denials
Another challenge faced in medical billing is insurance claim denials. Insurance companies have their own set of guidelines and requirements for reimbursement. Claim denials can occur due to various reasons, such as incomplete or inaccurate documentation, lack of medical necessity, or non-covered services. Dealing with claim denials requires thorough understanding of insurance policies and regulations, and it often involves extensive follow-up and appeals.
Reimbursement Delays
Reimbursement delays are a common frustration for healthcare providers. After submitting claims to insurance companies, it can take a significant amount of time for the providers to receive payment. These delays can have a negative impact on cash flow and hinder the financial stability of medical practices. It is crucial for healthcare providers to closely monitor the status of their claims and follow up with insurance companies to ensure timely reimbursement.
Compliance with Changing Regulations
Lastly, medical billing professionals must stay updated with the ever-changing regulations and requirements in the healthcare industry. From updates to coding guidelines and billing rules to changes in insurance policies, it is important to be aware of these changes to avoid claim denials and ensure accurate billing. Failure to comply with the changing regulations can result in penalties or legal issues.
In understanding the process of medical billing, it is crucial to be aware of the challenges that can arise. Medical coding errors, insurance claim denials, reimbursement delays, and compliance with changing regulations can all impact the billing process. By recognizing and addressing these challenges, healthcare providers and billing professionals can ensure smooth and efficient operations.
This image is property of reliancemm.com.
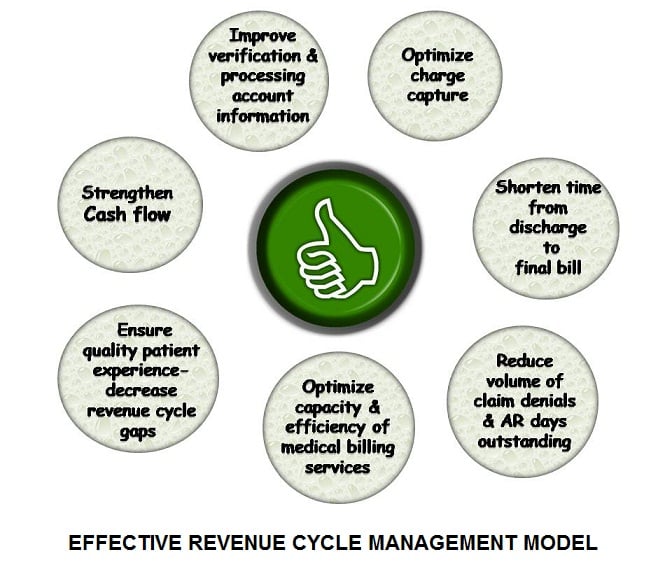
Importance of Accuracy and Compliance
Ensuring accurate documentation and compliance with regulations is integral to the process of medical billing. This section will delve into the significance of accuracy and compliance in medical billing, highlighting the importance of proper documentation, up-to-date knowledge of coding systems, and adherence to HIPAA regulations.
Ensuring Accurate Documentation
Accurate documentation plays a crucial role in medical billing. It ensures that all relevant patient information, diagnoses, treatments, and procedures are correctly recorded. By maintaining precise records, healthcare providers can expedite the billing process, minimize errors, and prevent potential issues with insurance claims. This not only avoids delays in reimbursement but also enhances patient care by facilitating accurate medical history tracking.
Up-to-date Knowledge of Coding System
Medical coders play a pivotal role in medical billing, as they assign codes to various medical procedures, diagnoses, and treatments. Having an extensive understanding of the coding system, such as the Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes, is essential. Accurate coding ensures timely claims submission, appropriate reimbursement, and compliance with insurance requirements.
HIPAA Compliance
Maintaining compliance with the Health Insurance Portability and Accountability Act (HIPAA) is vital in medical billing. HIPAA sets strict regulations to protect patient confidentiality and safeguard electronic health information. Adhering to HIPAA guidelines ensures that sensitive patient data is securely transmitted and stored, minimizing the risk of data breaches or unauthorized access. By prioritizing HIPAA compliance, healthcare providers reassures patients that their personal health information is safeguarded.
accuracy and compliance are paramount in the medical billing process. Ensuring accurate documentation, maintaining up-to-date coding knowledge, and adhering to HIPAA regulations not only streamline the billing process but also protect patient privacy and maximize reimbursement efficiency. Are you curious about how medical billing works? Medical billing is an essential process in the healthcare industry that ensures timely payment for services rendered. By understanding how it works, you can gain insight into the intricacies of medical billing and make informed decisions.
Latest Trends in Medical Billing

Automation and Artificial Intelligence
One of the latest trends in medical billing is the integration of automation and artificial intelligence (AI). These technologies streamline the billing process by automating repetitive tasks, such as coding and claim submissions. This not only reduces the chances of errors but also increases efficiency, allowing healthcare providers to focus more on patient care.
Telehealth and Remote Billing
Telehealth has become increasingly popular in recent years, particularly with the rise of remote consultations. This trend has spurred the development of remote billing services, enabling medical professionals to bill for their services provided via telehealth platforms. With the growing adoption of telehealth, remote billing plays a vital role in ensuring accurate and timely reimbursement.
Transparency in Pricing
Transparency in pricing is another significant trend in medical billing. Patients are becoming more empowered and involved in their healthcare financial decisions. As a result, healthcare providers are increasingly offering transparent pricing information, allowing patients to make informed choices about their treatments and understand the costs associated with their care.
Understanding these latest trends in medical billing will be crucial as you navigate the complex world of healthcare costs. By staying informed, you can make better decisions regarding your medical expenses and ensure a smooth billing process.
Conclusion
In conclusion, understanding the process of medical billing is crucial for both healthcare providers and patients alike. By familiarizing yourself with the steps involved, you can ensure a smooth and efficient billing experience.
Summary of Medical Billing Process
The medical billing process begins with the registration and scheduling of a patient’s appointment. Once the appointment is completed, the healthcare provider creates a detailed record of the services provided, including diagnosis, treatment, and any additional procedures. This information is then translated into medical codes, which are used to generate a claim. The claim is then submitted to the patient’s insurance company for reimbursement. If the claim is approved, the insurance company will remit payment directly to the healthcare provider. If the claim is denied or only partially paid, the patient is responsible for the remaining balance.
Future Outlook and Growth
The field of medical billing is expected to continue growing in the coming years. With advances in technology and changes in healthcare regulations, there will likely be a greater demand for skilled medical billers. Additionally, as more individuals gain access to healthcare coverage, the number of claims and reimbursements will increase, requiring efficient billing processes.
By understanding the intricacies of medical billing, you can navigate the system with confidence. Whether you are a healthcare provider or a patient, having knowledge of the medical billing process can help ensure fair and accurate reimbursement for medical services rendered.