In the realm of healthcare, billing systems play a crucial role in the financial operations of medical facilities. Understanding the various types of billing systems is essential for healthcare providers to efficiently manage and accurately process patient payments. This article examines three distinct billing systems commonly utilized in the healthcare industry, shedding light on their functionalities, advantages, and potential drawbacks. By delving into the intricacies of these billing systems, healthcare professionals can enhance their billing processes while ensuring compliance with industry standards and regulations.
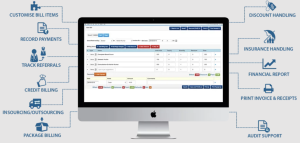
This image is property of cdn-aeclo.nitrocdn.com.
Overview of Billing Systems in Healthcare
Billing systems in healthcare play a crucial role in the financial management of healthcare organizations. These systems are designed to accurately process and generate bills for the services rendered to patients. By utilizing different billing systems, healthcare providers can streamline their revenue cycle management and ensure timely reimbursement for their services. In this article, we will explore the different types of billing systems used in healthcare, their key features, advantages, disadvantages, and their role in the future of healthcare billing.
Fee-for-Service Billing System
The fee-for-service billing system is one of the most common billing systems used in healthcare. Under this system, healthcare providers charge patients based on the services provided or procedures performed. Each service or procedure is assigned a specific fee, and the final bill is calculated by multiplying the fee with the quantity of services rendered.
Key Features
The key features of the fee-for-service billing system include:
- Service-Based Billing: Charges are calculated based on the specific services rendered to the patient.
- Individual Pricing: Each service or procedure has its own predetermined fee.
- Flexibility: Healthcare providers have the freedom to choose and perform services as needed.
Advantages
The fee-for-service billing system offers several advantages, including:
- Financial Incentives: Providers have the potential to earn more revenue by performing more services.
- Patient Flexibility: Patients have the freedom to choose their healthcare providers and services.
Disadvantages
Despite its advantages, the fee-for-service billing system has some disadvantages, including:
- Fragmented Care: Providers may focus on maximizing their revenue rather than coordinating care effectively.
- Cost Inflation: Unnecessary services may be performed to increase revenue, leading to higher healthcare costs.
Capitation Billing System
The capitation billing system is an alternative approach to healthcare billing where healthcare providers are paid a fixed, per-member-per-month fee for the services they provide to a specific group of patients, regardless of the actual services rendered. This system aims to promote cost-effective care and better coordination among healthcare providers.
Key Features
The key features of the capitation billing system include:
- Fixed Payments: Providers receive a predetermined payment for each patient assigned to them.
- Population Health Management: Providers are incentivized to provide preventive and coordinated care to improve patient outcomes.
Advantages
The capitation billing system offers several advantages, including:
- Cost Control: Providers are motivated to deliver efficient and cost-effective care to maximize their profit margins.
- Quality Improvement: Coordinated care and population health management can lead to improved patient outcomes.
Disadvantages
However, there are also some disadvantages to the capitation billing system, including:
- Inadequate Reimbursement: Providers may receive fixed payments that do not sufficiently cover the costs of providing care.
- Incentive Misalignment: Providers may prioritize cost savings over necessary treatments, potentially compromising patient care.
Bundled Payment Billing System
The bundled payment billing system is a payment model where healthcare providers receive a single payment for a specific episode of care, which includes all the services and procedures related to that episode. This system aims to incentivize providers to deliver coordinated and efficient care.
Key Features
The key features of the bundled payment billing system include:
- Episode-Based Payments: Providers receive a single payment for the entire episode of care.
- Care Coordination: Providers are encouraged to collaborate to ensure efficient and high-quality care.
Advantages
The bundled payment billing system offers several advantages, including:
- Cost Savings: Providers are motivated to streamline care delivery and reduce unnecessary services or procedures.
- Quality Improvement: Care coordination and collaboration among providers can lead to improved patient outcomes.
Disadvantages
However, there are also some disadvantages to the bundled payment billing system, including:
- Financial Risk: Providers may bear financial losses if the cost of care exceeds the bundled payment amount.
- Limited Scope: This system may not be suitable for all types of healthcare services and may require customization for different specialties.
This image is property of www.businessintegrityservices.com.
Resource-Based Relative Value Scale (RBRVS) Billing System
The Resource-Based Relative Value Scale (RBRVS) billing system is a widely used method of determining the payment for medical services based on the resources required to perform those services. It assigns relative values to different services based on factors such as physician work, practice expense, and malpractice insurance.
Key Features
The key features of the RBRVS billing system include:
- Relative Value Units (RVUs): Services are assigned specific RVUs based on the resources involved in providing them.
- Conversion Factor: RVUs are multiplied by a conversion factor to calculate the payment for a particular service.
Advantages
The RBRVS billing system offers several advantages, including:
- Standardization: It provides a standardized method for determining the payment for medical services.
- Transparency: The RVU-based payment system allows for more transparency in billing and reimbursement.
Disadvantages
However, there are also some disadvantages to the RBRVS billing system, including:
- Complexity: The calculation of RVUs and the conversion factor can be complex and may require specialized knowledge.
- Potential Inaccuracy: The system may not always accurately reflect the resources required to provide a specific service.
Prospective Payment System (PPS)
The Prospective Payment System (PPS) is a reimbursement methodology used primarily by government payers like Medicare and Medicaid. Under this system, predetermined payment rates are established for specific healthcare services or procedures based on various factors such as diagnosis, procedure codes, and patient characteristics.
Key Features
The key features of the Prospective Payment System (PPS) include:
- Diagnosis-Related Groups (DRGs): Services are categorized into DRGs, each associated with a predetermined payment rate.
- Fixed Payments: Providers receive a predetermined payment based on the patient’s diagnosis and the assigned DRG.
Advantages
The Prospective Payment System (PPS) offers several advantages, including:
- Cost Predictability: Providers can anticipate and plan their revenues based on the established payment rates.
- Incentive for Efficiency: Providers are motivated to deliver cost-effective care to maximize their revenue.
Disadvantages
However, there are also some disadvantages to the Prospective Payment System (PPS), including:
- Potential Underpayment: The fixed payment rates may not adequately cover the cost of providing certain healthcare services.
- Limited Flexibility: Providers may face challenges if the predetermined payment rates do not align with the actual costs incurred.
Electronic Billing Systems
Electronic billing systems, also known as e-billing systems, utilize electronic documentation and processing to streamline the billing and reimbursement process in healthcare. These systems replace paper-based billing with electronic records, making it more efficient, accurate, and secure.
Benefits
The benefits of electronic billing systems include:
- Improved Efficiency: Electronic billing systems automate various billing processes, reducing manual tasks and saving time.
- Enhanced Accuracy: These systems minimize human errors and ensure accurate billing and claims processing.
- Cost Savings: Electronic billing systems eliminate paper-related expenses and reduce administrative costs.
Implementation Challenges
While electronic billing systems offer numerous benefits, there are also implementation challenges to consider, including:
- Infrastructure Requirements: Healthcare organizations need the necessary infrastructure and technology to support electronic billing systems.
- Training and Adoption: Healthcare providers and staff must be trained to effectively use and adapt to electronic billing systems.
Management and Evaluation of Billing Systems
Efficiency Assessment
Efficiency assessment is a crucial aspect of managing billing systems in healthcare. It involves analyzing key performance indicators (KPIs) such as claim acceptance rates, denial rates, and revenue collection to identify areas for improvement. Regular monitoring and evaluation help identify bottlenecks and optimize the billing process for maximum efficiency.
Risk Management
Effective risk management is essential in billing systems to mitigate potential compliance and financial risks. This involves implementing controls, policies, and procedures to prevent fraud, abuse, and billing errors. Regular audits and internal reviews can help identify and address potential risks in billing practices.
Compliance Monitoring
Billing systems must comply with various regulations and guidelines, such as the Health Insurance Portability and Accountability Act (HIPAA) and the Centers for Medicare and Medicaid Services (CMS) guidelines. Compliance monitoring ensures adherence to these regulations, minimizing the risk of penalties and legal issues. Regular education and training on compliance requirements are also essential for billing system management.
This image is property of www.outsourceaccelerator.com.
Billing Systems and Revenue Cycle Management
Billing systems play a critical role in revenue cycle management (RCM), which involves the financial aspects of patient care from registration to final payment. Integrating billing systems with other RCM components such as patient registration, charge capture, and claims processing streamlines the entire revenue cycle and ensures timely reimbursement.
Workflow Optimization
Optimizing workflows in billing systems improves efficiency and reduces errors in claim submission and payment processing. Workflow optimization includes automating manual tasks, standardizing processes, and utilizing technology to streamline communication and data exchange between different departments involved in the billing process.
Claims Processing
Effective claims processing is a fundamental function of billing systems in healthcare organizations. This involves verifying patient eligibility, submitting accurate and timely claims to payers, and managing denials and appeals. Efficient claims processing ensures proper reimbursement and minimizes revenue leakage.
Future Trends in Healthcare Billing Systems

Value-based Care and Alternative Payment Models
The future of healthcare billing systems is shifting towards value-based care and alternative payment models. These models focus on quality outcomes and incentivize providers to deliver high-value care. Instead of volume-based fee-for-service payments, providers may be reimbursed based on the quality, efficiency, and effectiveness of care provided.
Artificial Intelligence and Automation
Artificial intelligence (AI) and automation are poised to revolutionize healthcare billing systems. AI-powered algorithms can analyze large volumes of data, identify patterns, predict billing errors, and automate claim submission and payment processes. This not only improves accuracy and efficiency but also frees up resources for more complex tasks.
Interoperability and Data Integration
Interoperability and data integration are key drivers for the future of healthcare billing systems. Seamless exchange of patient data between different healthcare systems and payers improves billing accuracy, reduces administrative burden, and enhances the overall patient experience. Standardized data exchange protocols and interoperable systems will be crucial for achieving this goal.
In conclusion, billing systems in healthcare play a vital role in revenue cycle management and ensure timely reimbursement for healthcare services. The various types of billing systems, such as fee-for-service, capitation, bundled payment, RBRVS, and PPS, offer different approaches to billing and reimbursement. Electronic billing systems provide numerous benefits, but their implementation requires careful planning and consideration of infrastructure and training requirements. Efficient management, evaluation, and integration of billing systems are crucial for effective revenue cycle management. The future of healthcare billing systems lies in value-based care, AI, automation, interoperability, and data integration, which will shape the way healthcare services are billed and reimbursed.
