In the realm of medical billing, the term AOB holds significant importance. AOB, which stands for Assignment of Benefits, plays a crucial role in the financial transactions between healthcare providers and insurance companies. Particularly, it refers to the legal agreement that allows healthcare providers to receive payment directly from the insurance company, reducing the burden on patients. Understanding the concept of AOB is vital in the complex landscape of medical billing, as it can greatly affect both patients and healthcare providers.
Definition of AOB in Medical Billing
AOB stands for Assignment of Benefits in the context of medical billing. An Assignment of Benefits is a written agreement between a healthcare provider and a patient that authorizes the provider to directly receive payment from the patient’s insurance company for services rendered. In simpler terms, it is a legal document that allows healthcare providers to be paid directly by the patient’s insurance rather than requiring the patient to pay out-of-pocket and then seek reimbursement.
Explanation of AOB in the context of medical billing
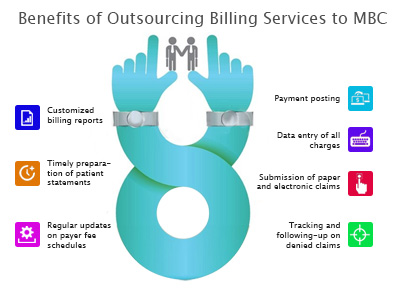
In medical billing, an AOB is a crucial element that streamlines the payment process for healthcare providers, patients, and insurance companies. By utilizing an AOB, providers can avoid the hassle of dealing directly with patients’ insurance companies and instead be paid promptly and directly for the services they provide. This arrangement benefits patients as well, as it minimizes their financial burden by reducing or potentially eliminating the need to pay the full cost of medical services upfront.
Purpose and Importance of AOB

Why is AOB important in medical billing?
AOB plays a significant role in medical billing as it facilitates the seamless flow of payment between the healthcare provider, the patient, and the insurance company. It eliminates the need for patients to manage their own claims and ensures that providers receive timely payment for the care they deliver. AOB is especially vital for patients who have limited financial resources or rely on health insurance coverage to access necessary medical treatment.
Role of AOB in the billing process
The AOB serves as an agreement that allows healthcare providers to receive direct payment from the patient’s insurance company. Without an AOB, patients may be required to pay out-of-pocket and then seek reimbursement from their insurance company. This process can be time-consuming and often leads to delays in payment. By obtaining an AOB from patients, providers eliminate these delays and can focus on delivering quality care rather than dealing with administrative complexities.
Impact of AOB on healthcare providers and patients
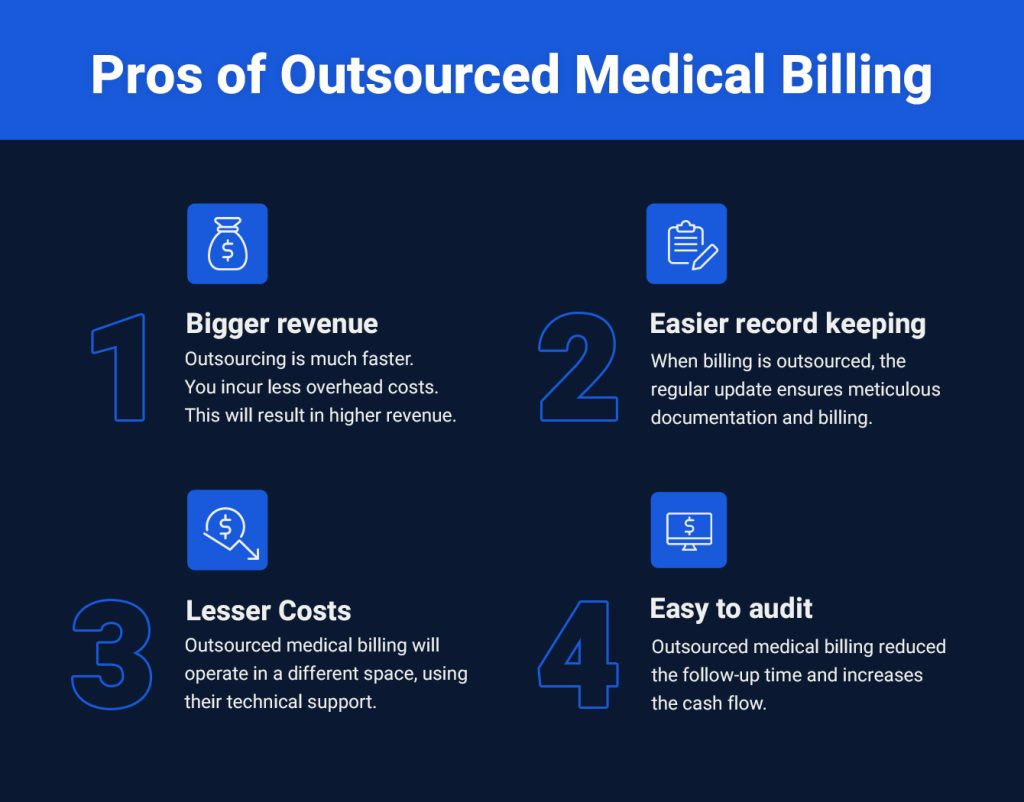
For healthcare providers, utilizing AOBs streamlines the billing and payment process, reduces paperwork, and ensures more predictable cash flow. Providers can avoid the burden of collecting payment directly from patients and instead receive prompt payment from the insurance companies. This results in improved financial stability for healthcare practices.
For patients, AOBs minimize their financial burden by allowing providers to bill their insurance directly. Patients are not required to pay the full cost of services upfront, alleviating the stress associated with managing medical bills. AOBs also promote transparency, as patients are aware of the services covered by their insurance and the portion they may be responsible for paying out-of-pocket.
AOB Documentation

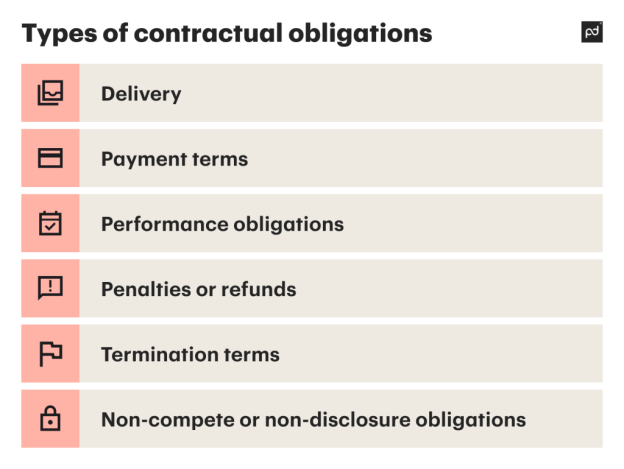
Types of AOB documentation
There are various types of AOB documentation that providers may use to secure authorization for direct payments from insurance companies. These documents include AOB forms, letters of authorization, or clauses within the patient’s registration or consent forms. The specific type of documentation may vary depending on the healthcare provider’s practice and the requirements of the insurance companies they work with.
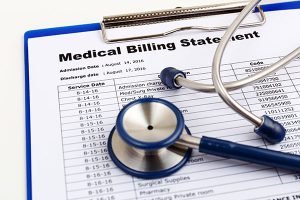
Content and format of AOB forms
AOB forms typically require specific information to fulfill the requirements of insurance companies. The forms generally include the patient’s personal information, the healthcare provider’s details, the insurance company’s information, and a clear statement from the patient authorizing the provider to bill the insurance company directly. The AOB form may also include details about the services covered under the agreement, any limitations or exclusions, and the rights and responsibilities of both the provider and the patient.
AOB Authorization and Consent

Obtaining AOB authorization
Obtaining AOB authorization from patients is an essential step in the medical billing process. Providers must educate patients about the purpose and benefits of an AOB and secure their consent to initiate direct billing with their insurance provider. This can be done during the patient registration process or through a separate consent form specifically addressing AOB authorization.
It is crucial for providers to clearly communicate the implications of granting AOB authorization to patients. They should explain the potential impact on the insurance claims process, insurance coverage, and any financial obligations that may still exist despite the agreement. Providers should ensure that patients fully understand the terms stated in the AOB before proceeding.
Legal requirements for AOB consent
When obtaining AOB consent from patients, healthcare providers must comply with all relevant legal requirements. These requirements may vary depending on the jurisdiction and the specific regulations governing the healthcare industry in that region. Providers should familiarize themselves with applicable laws and regulations to ensure they meet all necessary consent and authorization standards. This may include adhering to privacy and confidentiality laws, providing patients with copies of the AOB agreement, and obtaining a signature or other form of explicit consent.
AOB and Insurance Claims

Role of AOB in insurance claims
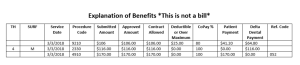
The AOB plays a critical role in the insurance claims process. With an AOB in place, healthcare providers can submit claims directly to the patient’s insurance company on their behalf. This eliminates the need for patients to personally file claims and follow up with the insurance company themselves, streamlining the reimbursement process for both the provider and the patient.
Submitting AOB claims to insurance companies
To submit AOB claims to insurance companies, providers typically follow the standard claim submission process. Providers encode the necessary billing and diagnosis codes, attaching any supporting documentation required by the insurance company. The information included in the AOB form serves as a reference for the insurance company to verify the details of the agreement and process the claim accordingly. The insurance company reviews the claim and reimburses the provider directly according to the terms of the AOB.
AOB and Medical Coding

Coding and documentation requirements for AOB
Healthcare providers must adhere to specific coding and documentation requirements when utilizing AOBs. accurate medical coding is essential for ensuring the correct classification and billing of services rendered. Providers must assign appropriate Current Procedural Terminology (CPT) codes, International Classification of Diseases (ICD) codes, and other relevant codes to accurately reflect the services provided. Additionally, proper documentation must support the coded services and justify the medical necessity of the treatments.
Impact of AOB on medical coding
AOBs can influence medical coding by introducing additional considerations for providers. When coding services for AOB claims, providers must align their coding practices with the specific insurance policies and guidelines outlined in the AOB agreement. The agreement may specify certain covered services, exclusions, or limitations that could impact the coding choices made by the provider. Accurate coding within the framework of the AOB agreement ensures proper reimbursement and compliance with insurance regulations.
AOB and Reimbursement
Effects of AOB on reimbursement process
AOBs have a significant impact on the reimbursement process for healthcare providers. By enabling direct payments from insurance companies, providers can receive reimbursement in a more timely and predictable manner. This reduces the likelihood of delayed or denied payments, resulting in improved cash flow for the practice. AOBs also limit the financial burden on patients, as they are no longer responsible for upfront payment or waiting for reimbursement from their insurance.
AOB and payment negotiations with insurance companies
In some instances, healthcare providers may need to negotiate payment terms and rates with insurance companies that differ from the standard reimbursement rates. By leveraging the AOB agreement, providers can engage in payment negotiations with insurance companies to establish mutually acceptable terms. These negotiations may involve discussing specific services, rates, or other financial arrangements. AOBs provide providers with a foundation for payment discussions, ensuring that reimbursement aligns with the value of the services provided.
AOB in Specialized Medical Billing

AOB in specific medical specialties (e.g., dental, physical therapy)
AOBs are relevant across various medical specialties, including dental, physical therapy, and others. In dental practices, AOBs allow dentists to bill insurance directly for services such as cleanings, fillings, and oral surgeries. Similarly, in physical therapy, AOBs help therapists receive payment directly from insurance companies for treatments provided to patients. AOBs streamline the billing process within these specialized fields, making it more efficient for both providers and patients.
Considerations for AOB in specialized practices
While AOBs are applicable in specialized practices, providers must consider the unique requirements and regulations specific to their field. Some insurance companies may have specific AOB forms or guidelines tailored to certain specialties, which providers need to adhere to during the billing process. It is crucial for specialized healthcare providers to stay updated on industry-specific billing practices and regulations to ensure AOB implementation is done accurately and compliantly.
Challenges and Pitfalls of AOB
Implementing AOBs in medical billing can present certain challenges. One common challenge is obtaining accurate patient information and insurance details necessary for submitting claims. Poor documentation or incomplete patient information can lead to claim denials or delays. Providers must also ensure that patients fully understand the terms and implications of the AOB and that their consent is properly documented.
Additionally, insurance companies may have specific requirements or restrictions regarding AOBs, potentially leading to claim rejections or reduced reimbursement rates. Providers must familiarize themselves with insurance policies and guidelines to mitigate these challenges. Maintaining open lines of communication with insurance companies and staying informed about industry changes can help navigate potential obstacles effectively.
Risks and consequences of mishandling AOB
Mishandling AOBs can result in financial risks and consequences for both healthcare providers and patients. Inaccurate coding, improper documentation, or failing to comply with AOB regulations can lead to denied claims, delayed payments, or even legal disputes. Providers may experience financial strain if they are unable to collect payment for services rendered, impacting their ability to provide quality care. Patients may also face financial repercussions if their insurance claims are mishandled, potentially leading to unexpected out-of-pocket expenses for services they believed were covered. Therefore, it is crucial for providers to diligently follow AOB guidelines and maintain accurate records to minimize these risks.
AOB Regulations and Compliance

Applicable laws and regulations related to AOB
AOBs are subject to regulations and laws that healthcare providers must comply with. The specifics of these regulations may vary depending on factors such as the location, healthcare system, and insurance industry. Providers must be familiar with laws related to patient consent, insurance billing practices, privacy, and any specific requirements set by insurance companies. Staying informed about relevant regulations ensures that providers maintain compliance and avoid potential legal pitfalls.
Compliance guidelines for healthcare providers
To ensure compliance with AOB regulations, healthcare providers should establish comprehensive internal policies and procedures. These guidelines should cover key areas such as AOB authorization, coding practices, documentation requirements, and consistent communication with insurance companies. Regular staff training, ongoing monitoring, and audits for compliance can help providers identify and rectify any compliance gaps. By adhering to compliance guidelines, providers can minimize the risk of legal issues, protect patient interests, and maintain ethical billing practices.
In summary, the Assignment of Benefits (AOB) plays a critical role in medical billing. From streamlining the payment process for healthcare providers and patients to facilitating efficient insurance claims and reimbursement, AOBs offer numerous benefits to all stakeholders. By understanding the importance of AOB documentation, obtaining proper authorization and consent, and complying with applicable regulations, healthcare providers can effectively navigate the complexities of AOBs in medical billing, ensuring financial stability and improved patient experiences.